| |
16:00
|
1000.
 |
Automatic adaption of ASL labeling parameters: Walsh-sorted
time-encoded pCASL with a dynamic feedback algorithm 
Nora-Josefin Breutigam1, Federico von
Samson-Himmelstjerna1, and Matthias Günther1
1MR Physics, Fraunhofer MEVIS, Bremen, Germany
A dynamic feedback algorithm to find the optimal free-lunch
(FL) bolus-length in a multi-TI Hadamard-encoding scheme is
presented. An estimated FL bolus-length is often not ideal
for the examined subject. In arterial spin labeling (ASL)
this frequently results in unwanted arterial transit-delay (ATD)
artefacts. The proposed method allows approaching the
optimal FL bolus-length individually by analyzing
intermediate decoded perfusion-weighted images during a
running MRI scan. The aim is to reduce the FL bolus-length
as much as necessary, but to keep it as long as possible to
yield maximal signal.
|
| |
16:12
 |
1001.
 |
Combined Angiography and Perfusion using Radial Imaging and
Arterial Spin Labeling 
Thomas W. Okell1
1FMRIB Centre, Nuffield Department of Clinical
Neurosciences, University of Oxford, Oxford, United Kingdom
A new golden angle radial arterial spin labeling acquisition
method is proposed in which labeled blood water is
continuously imaged as it passes through the large arteries
and into the tissue. Both angiographic and perfusion images
can then be reconstructed from the same raw data set at any
retrospectively chosen time points and temporal resolution.
This makes efficient use of the post-labeling delay dead
time to provide a more complete assessment of blood flow
into the brain, which may be of use in a variety of
cerebrovascular diseases.
|
| |
16:24
 |
1002.
 |
Comparison of perfusion signal acquired by ASL prepared IVIM and
conventional IVIM to unravel the origin of the IVIM-signal 
Xingxing Zhang1, Carson Ingo1, and
Matthias J.P. van Osch1,2
1C. J. Gorter Center for High Field MRI,
Department of Radiology, Leiden University Medical Center,
Leiden, Netherlands, 2Leiden
Institute for Brain and Cognition, Leiden, Netherlands
ASL-prepared IVIM is proposed to study the arterial IVIM
signal as a function of post-labeling-delay. The D*-value as
calculated from ASL-IVIM decreases as a function of PLD,
reaching a plateau for PLDs>2000ms. Signal from conventional
IVIM shows an intermediate D*-value corresponding to the
ASL-IVIM-signal for a PLD of ~1750ms indicating the IVIM
signal does not only originate from the microvasculature,
but also includes vascular signal. The alternative
explanation of extravasation of labeled spins into the
extravascular compartment seems unlikely, since the observed
D* at these PLDs are still a factor 3~4 higher than the
diffusion coefficient of the slow compartment.
|
| |
16:36
|
1003.
 |
Flow territory instability may provide a new measure of
hemodynamic reserve capacity in patients with intracranial
stenosis 
Daniel Arteaga1, Megan Strother1,
Taylor Davis1, Carlos Faraco1, Lori
Jordan2, Allison Scott1, and Manus
Donahue1
1Radiology, Vanderbilt University, Nashville, TN,
United States, 2Neurology,
Vanderbilt University, Nashville, TN, United States
Non-invasive, hemodynamic markers are needed to better
characterize stroke risk in patients with symptomatic
intracranial (IC) stenosis. We developed and applied a
planning-free vessel-encoded pseudo-continuous arterial spin
labeling sequence in IC stenosis patients during room air
and hypercapnia to examine the extent of geometrical changes
in cerebral blood flow territories. IC stenosis patients
demonstrated increased shifting relative to healthy
controls; among IC stenosis patients, shifting was higher in
those who experienced non-cardioembolic stroke within
two-years. Shifting of cerebral blood flow territories may
provide a novel marker of hemodynamic impairment and stroke
risk.
|
| |
16:48
|
1004.
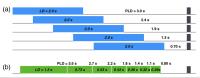 |
Comparing Single-Delay, Sequential Multi-delay, and Hadamard
Multi-delay ASL for Measuring CBF and Arterial Transit Delay in
Normal Subjects and Patients with Cerebrovascular Disease - Permission Withheld
Samantha Holdsworth1, Audrey Fan1,
Marc Lebel2, Zungho Zun3, Ajit
Shankaranarayanan4, and Greg Zaharchuk1
1Department of Radiology, Stanford University,
Stanford, CA, United States, 2GE
Healthcare, Calgary, Canada, 3George
Washington University, Washington, DC, United States, 4GE
Healthcare, Menlo Park, CA, United States
One promising approach to multi-delay ASL is to perform the
labeling using a Hadamard-encoded method, which promises to
improve the SNR efficiency compared with sequential
multi-delay ASL. In this study, we compared single-delay
ASL, sequential multi-delay ASL, and Hadamard-encoded
multi-delay ASL in normal subjects and in patients with
cerebrovascular disease. Consistent with theory,
Hadamard-encoding had better SNR than sequential multi-delay
ASL for measuring CBF and arterial transit delay.
|
| |
17:00
 |
1005.
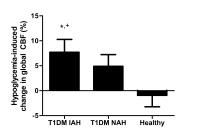 |
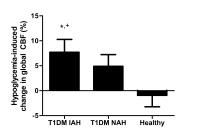
Hypoglycemia-induced changes in global and regional cerebral
blood flow; impact of type 1 diabetes and impaired awareness of
hypoglycemia 
Evita Wiegers1, Kirsten Becker1, Hanne
Rooijackers2, Cees Tack2, Arend
Heerschap1, Bastiaan de Galan2, and
Marinette van der Graaf1,3
1Radiology and Nuclear Medicine, Radboud umc,
Nijmegen, Netherlands, 2Internal
Medicine, Radboud umc, Nijmegen, Netherlands, 3Pediatrics,
Radboud umc, Nijmegen, Netherlands
Hypoglycemia-induced changes in global and regional cerebral
blood flow (CBF) were investigated in patients with type 1
diabetes (T1DM) and impaired (IAH) or normal awareness of
hypoglycemia (NAH) and in healthy subjects. CBF-weighted
images were acquired using pseudo-continuous arterial spin
labeling MRI. Global CBF increased in response to
hypoglycemia in T1DM IAH subjects, but not in T1DM NAH or in
healthy controls. Hypoglycemia induced regional relative
increases in CBF in the thalamus of both T1DM NAH and
healthy controls, and in the frontal lobes of T1DM NAH,
while no such increases were found in the T1DM IAH group.
|
| |
17:12
 |
1006.
 |
Fast measurement of blood T1 in the internal carotid artery at
3T 
Wenbo Li1,2, Peiying Liu1, Hanzhang Lu1,
John J. Strouse3, Peter C.M. van Zijl1,2,
and Qin Qin1,2
1Radiology, Johns Hopkins University School of
Medicine, Baltimore, MD, United States, 2F.M.
Kirby Research Center for Functional Brain Imaging, Kennedy
Krieger Institute, Baltimore, MD, United States,3Division
of Pediatric Hematology, Johns Hopkins University School of
Medicine, Baltimore, MD, United States
The knowledge of arterial blood T1 is important to quantify
cerebral blood flow with ASL or the inversion time for VASO
experiments. We used a fast blood T1 protocol to measure
the arterial T1 values in the internal carotid artery in
vivo. Ex-vivo experiments were conducted to validate our
method. Excellent correlation and agreement was found
between in vivo and ex vivo results. The group-averaged
arterial blood T1 value over 9 healthy volunteers was
1864+/-92ms (Hct=0.41+/-0.04), which is 200 ms longer than
the widely adopted number obtained from bovine blood
experiments. The arterial T1 value per subject was found to
have significant correlation with the individual Hct values.
|
| |
17:24
 |
1007.
 |
Non-contrast Pulmonary Perfusion at 3T using FAIR with inflow
saturation and background suppression 
Joshua S. Greer1,2, Yue Zhang2,
Christopher Maroules2, Orhan K. Oz2,
Ivan Pedrosa2,3, and Ananth J. Madhuranthakam2,3
1Bioengineering, University of Texas at Dallas,
Richardson, TX, United States, 2Radiology,
UT Southwestern Medical Center, Dallas, TX, United States, 3Advanced
Imaging Research Center, UT Southwestern Medical Center,
Dallas, TX, United States
Flow Alternating Inversion Recovery (FAIR) has been studied
extensively for pulmonary perfusion imaging at 1.5T, but
suffers from low SNR, and is often corrupted by bright
signal in the major vasculature and image misregistration
artifacts due to respiratory motion. The purpose of this
study was to evaluate FAIR at 3T for increased SNR and
compare against SPECT perfusion, to combine FAIR with inflow
saturation to reduce signal in the major pulmonary vessels,
and to combine FAIR with background suppression strategies
to minimize artifacts due to image misregistration.
|
| |
17:36
|
1008.
 |
Velocity Selective Adiabatic Pulses for Arterial Spin Labeling 
Luis Hernandez-Garcia1, Jon-Fredrik Nielssen2,
and Douglas Noll1
1FMRI Laboratory, University of Michigan, Ann
Arbor, MI, United States, 2Biomedical
Engineering, University of Michigan, Ann Arbor, MI, United
States
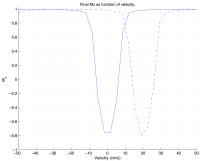
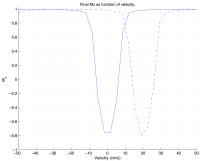
We introduce a class of adiabatic RF pulses that can invert
the magnetization of spins moving at specific velocity
bands, regardless of their position within the coil.
Velocity selective adiabatic pulses (VSAI) are more robust
to B1 inhomogeneity than their non-adiabatic counterparts.
We discuss the theory and design considerations and
demonstrate their utility in an ASL experiment on a human
brain at 3T.
|
| |
17:48
 |
1009.
 |
Incorporation of labeling efficiency measurement into a normal
pCASL perfusion scan without SNR-penalty 
Zhensen Chen1, Xihai Zhao1, Wouter
Teeuwisse2, Bida Zhang3, Peter Koken4,
Jouke Smink5, and Matthias J.P. van Osch2
1Certer for Biomedical Imaging Research, School
of Medicine, Tsinghua University, Beijing, China, People's
Republic of, 2C.
J. Gorter Center for High Field MRI, Department of
Radiology, Leiden University Medical Center, Leiden,
Netherlands, 3Philips
Research China, Beijing, China, People's Republic of, 4Innovative
Technologies, Research Laboratories, Philips Technologie
GmbH, Hamburg, Germany, 5Philips
Healthcare, MR Clinical Science, Best, Netherlands
The pCASL perfusion sequence was modified to incorporate a
labeling efficiency measurement during the post-labeling
delay. Our in vivo data showed that the incorporated
labeling efficiency measurement had no influence on SNR of
the perfusion measurements, with almost no additional time
penalty. The additional labeling efficiency measurement was
demonstrated its ability to identify severe underestimation
of CBF caused by sub-optimal labeling, proofing its clinical
potential. Moreover, the measured labeling efficiency is
artery-specific, which is important because arteries may
have different labeling efficiency due to differences in
flow velocity and/or off-resonance effects.
|
|