|
|
|
Plasma # |
 |
0182.
 |
1 |
Immune co-stimulatory blockade permits human glioblastoma
xenografting in immunocompetent mice: model validation with MRI
and bioluminescence imaging 
Samantha Lynn Semenkow1, Shen Li2,
Eric Raabe1,3, Jiadi Xu2,4, Miroslaw
Janowski2,5, Byoung Chol Oh6, Gerald
Brandacher6, Jeff W. Bulte2,4, Charles
Eberhart1,3,7, and Piotr Walczak2
1Department of Pathology, Johns Hopkins Medical
Institue, Baltimore, MD, United States, 2Department
of Radiology and Radiological Science, Johns Hopkins Medical
Institue, Baltimore, MD, United States, 3Department
of Oncology, Johns Hopkins Medical Institue, Baltimore, MD,
United States, 4F.
M. Kirby Center for Functional Brain Imaging Kennedy Krieger
Institute, Johns Hopkins Medical Institue, Baltimore, MD,
United States, 5NeuroRepair
Department, Mossakowski Medical Research Centre, Warsaw,
Poland, 6Department
of Plastic and Reconstructive Surgery, Vascularized
Composite Allotransplantation (VCA) Laboratory, Johns
Hopkins Medical Institue, Baltimore, MD, United States, 7Department
of Opthalmology, Johns Hopkins Medical Institue, Baltimore,
MD, United States
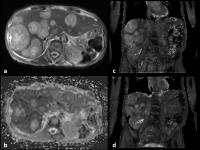
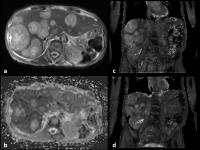
Immunodeficient mice are currently used for modeling human
brain tumor xenografts; however, immunodeficiency is a
serious limitation precluding studies based on immunotherapy
or inducing tumors in a variety of transgenic animal models.
We therefore investigated whether disruption of
co-stimulatory signaling using blocking antibodies induces
tolerance to intracerebrally transplanted human glioblastoma
xenografts in immunocompetent mice. With longitudinal MRI
and bioluminescence we established that the growth rate of
xenografts is comparable between immunodeficient and
tolerance-induced immunocompetent mice. Quantitative MRI
including T2/T1 relaxation time, MTR, diffusion parameters
and perfusion were not significantly different, validating
this new approach as a reliable brain tumor model.
|
 |
0183.
 |
2 |
In vivo 1H MRS and MRI longitudinal assessment of GBM mouse
xenografts derived from freshly injected human cells 
Marta Lai1, Cristina Cudalbu2,
Marie-France Hamou3,4, Mario Lepore2,
Lijing Xin2, Roy Thomas Daniel4,
Andreas Felix Hottinger5, Monika Hegi3,4,
and Rolf Gruetter1,6,7
1Laboratory of Functional and Metabolic Imaging
(LIFMET), Ecole Polytechnique Fédérale de Lausanne,
Lausanne, Switzerland, 2Animal
Imaging and Technology Core (AIT), Center for Biomedical
Imaging (CIBM), Ecole Polytechnique Fédérale de Lausanne,
Lausanne, Switzerland, 3Laboratory
of Brain Tumor Biology and Genetics, Neuroscience Research
Center, Lausanne University Hospital (CHUV), Lausanne,
Switzerland, 4Service
of Neurosurgery, Department of Clinical Neurosciences,
Lausanne University Hospital (CHUV), Lausanne, Switzerland, 5Service
of Neurology, Department of Clinical Neurosciences, Lausanne
University Hospital (CHUV), Lausanne, Switzerland, 6Department
of Radiology, University of Geneva, Geneva, Switzerland, 7Department
of Radiology, University of Lausanne, Lausanne, Switzerland
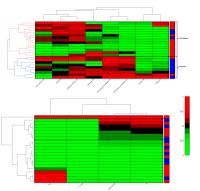
In the present study orthotopic xenograft mice models of
glioblastoma (GBM) derived from freshly dissected human
cells of three different patients were compared at the aim
of assessing patient-to-patient variability related to tumor
metabolism and structural development. Mice were followed
longitudinally in
vivo in a
14.1 Tesla scanner with MRI and 1H
MRS which allowed to precisely quantify a wide range of GBM
biomarkers. Finally spectra examined at late stage revealed
peculiarity linked to each patient-derived xenograft, while
longitudinal evolution of GBM biomarkers showed a close
similarity in their expression within the same group and in
animal lifespan.
|
|
0184.
 |
3 |
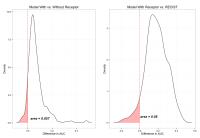
Multi-modal MRI Parametric Maps Combined with Receptor
Information to Optimize Prediction of Pathologic Response to
Neoadjuvant Chemotherapy in Breast Cancer 
Hakmook Kang1,2, Allison Hainline1,
Xia Li3, Lori R. Arlinghaus4, Vandana
G. Abramson5,6, A. Bapsi Chakravarthy5,7,
Brian Bingham8, and Thomas E. Yankeelov2,4,5,9
1Biostatistics, Vanderbilt University, Nashville,
TN, United States, 2Center
for Quantitative Science, Vanderbilt University, Nashville,
TN, United States, 3GE
Global Research, Niskayuna, NY, United States,4Institute
of Imaging Science, Vanderbilt University, Nashville, TN,
United States, 5Ingram
Cancer Center, Vanderbilt University, Nashville, TN, United
States, 6Medical
Oncology, Vanderbilt University, Nashville, TN, United
States, 7Radiation
Oncology, Vanderbilt University, Nashville, TN, United
States, 8School
of Medicine, Vanderbilt University, Nashville, TN, United
States, 9Radiology
and Radiological Sciences, Vanderbilt University, Nashville,
TN, United States
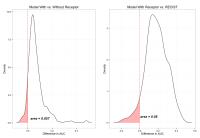
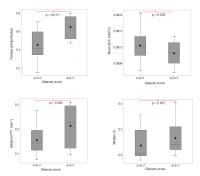
Pathologic complete response (pCR) following neoadjuvant
chemotherapy is used as a short term surrogate marker of
ultimate outcome in patients with breast cancer. Current
imaging tools are suboptimal in predicting this response.
Analyzing voxel-level heterogeneity in multi-modal MRI maps
in conjunction with receptor status data, i.e., DCE- and
DW-MRI, and ER/PR/HER2 status, allows us to improve the
predictive power after the first cycle of neoadjuvant
chemotherapy (NAC).
|
 |
0185.
 |
4 |
Early post-treatment changes of multi-parametric whole-body MRI
quantitative parameters following Bortezomib induction in
multiple myeloma; Preliminary results at 3.0 T 
Arash Latifoltojar1, Margaret Hall-Craggs2,
Alan Bainbridge2, Magdalena Sokolska2,
Kwee Yong1, Neil Rabin2, Liam Watson1,
Michelle Siu2, Matthew Benger2,
Nikolaos Dikaios1, and Shonit Punwani1
1University College London, London, United
Kingdom, 2University
College London Hospital, London, United Kingdom
Whole body magnetic resonance imaging is becoming the gold
standard imaging in initial assessment of multiple myeloma.
Recently, functional imaging is being investigated in
treatment response monitoring in multiple myeloma. We
investigated different functional MRI biomarkers' temporal
changes at early post-treatment stage in multiple myeloma
patients following Bortezomib induction.
|
 |
0186.
 |
5 |
The origins of glucoCEST signal: effect inhibiting glucose
transport in brain tumors 
Xiang Xu1,2, Jiadi Xu1,2, Linda
Knutsson3, Yuguo Li1,2, Huanling Liu1,4,
Guanshu Liu1,2, Bachchu Lal5,6, John
Laterra5,6, Dmitri Artemov7,8, Michael
T. McMahon1,2, Peter C.M. van Zijl1,2,
and Kannie WY Chan1,2
1Radiology, Johns Hopkins University School of
Medicine, Baltimore, MD, United States, 2FM
Kirby Research Center, Kennedy Krieger Institute, Baltimore,
MD, United States, 3Department
of Medical Radiation Physics, Lund University, Lund, Sweden, 4Department
of Ultrasound, Guangzhou Panyu Central Hospital, Panyu,
China, People's Republic of, 5Department
of Neurology, Kennedy Krieger Institute, Baltimore, MD,
United States, 6Department
of Neuroscience, Kennedy Krieger Institute, Baltimore, MD,
United States, 7Division
of Cancer Imaging Research, Johns Hopkins University School
of Medicine, Baltimore, MD, United States, 8JHU
In Vivo Cellular Molecular Imaging Center, Baltimore, MD,
United States
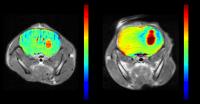
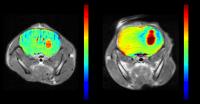
Recently D-glucose has shown potential to be used as a
biodegradable contrast agent for cancer detection. However
the origins of the glucoCEST signal is not yet completely
understood. To identify the contributions to glucoCEST
contrast, we administrated a glucose transporter inhibitor
in a group of mice with implanted glioma. By inhibiting
glucose transport into the cells, the effects of cellular
glucose uptake and metabolism are suppressed and the
perfusion properties of the extravascular extracellular
space are delineated. A greater increase in glucoCEST
contrast was seen in tumors in the group of mice with
glucose transporter inhibitor compared to a group of mice
without. This greater uptake and retention of glucose in the
inhibitor group provides evidence that the intracellular
glucose contribution is minimal.
|
|
0187.
 |
6 |
CEST Metrics for Assessing Early Response to Stereotactic
Radiosurgery in Human Brain Metastases 
Kimberly L. Desmond1,2, Hatef Mehrabian1,2,
Arjun Sahgal1,3, Hany Soliman1,3, and
Greg J. Stanisz1,2
1Physical Sciences, Sunnybrook Research
Institute, Toronto, ON, Canada, 2Medical
Biophysics, University of Toronto, Toronto, ON, Canada, 3Radiation
Oncology, Odette Cancer Centre, Toronto, ON, Canada
Chemical exchange saturation transfer (CEST) spectra were
collected at three timepoints following stereotactic
radiosurgery (SRS). The magnetization transfer ratio (MTR)
and CEST peak properties were evaluated at the offset
frequencies of the NOE, amide and amine pools in the lesion
and in the surrounding tissue. Positive correlation was
found between changes in NOE peak amplitude and amide MTR at
1 week post-therapy and tumour volume change at one month
post-therapy, while negative correlation was found between
amide peak width and NOE peak amplitude at the
pre-treatment timepoint with volume change at one month
post-therapy (p<0.1).
|
|
0188.
 |
7 |
Predicting TP53 mutational status of breast cancers on clinical
DCE MRI using directional-gradient based radiogenomic
descriptors 
Nathaniel Braman1, Prateek Prasanna1,
Donna Plecha2, Hannah Gilmore2,
Lyndsay Harris2, Kristy Miskimen1, Tao
Wan3, Vinay Varadan1, and Anant
Madabhushi1
1Case Western Reserve University, Cleveland, OH,
United States, 2University
Hospitals, Cleveland, OH, United States, 3Beihang
University, Beijing, China, People's Republic of
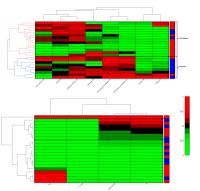
In this work, we report preliminary success in the
prediction of TP53 mutational status in breast cancer from
DCE-MRI using a computer-extracted radiogenomic descriptor
of multi-scale disorder, Co-occurrence of Local Anisotropic
Gradient Orientations (CoLlAGe). A set of 8 distinguishing
CoLlAGe features yielded accuracy of 78% in predicting TP53
mutational status and outperformed standard DCE-MRI
pharmacokinetic parameters in an unsupervised hierarchical
clustering. A non-invasive means of discerning TP53
mutational status may allow clinicians to more easily
determine prognosis, assess treatment response, and inform
treatment strategy.
|
|
0189.
 |
8 |
A Prototype Image Quality Assurance System for Accelerated
Quantitative Breast DCE-MRI 
Yuan Le1, Aneela Afzal2, Xiao Chen3,
Bruce Spottiswoode4, Wei Huang2, and
Chen Lin1
1Radiology and Imaging Science, Indiana
University School of Medicine, Indianapolis, IN, United
States, 2Advanced
Imaging Research Center, Oregon Health and Science
University, Portland, OR, United States, 3Siemens
Healthcare, Princeton, NJ, United States, 4Siemens
Healthcare, Chicago, IL, United States
The goal of this work is to build a prototype quality
assurance (QA) system for the quantitative pharmacokinetic
(PK) analysis of breast DCE-MRI acquired with accelerated
imaging techniques. A 3D digital tumor model with two
sub-regions was constructed by segmenting patient images.
The dynamic contrast enhanced images were synthesized
according to the Tofts and Shutter Speed models with the
TWIST technique. The QA system shows how the TWIST technique
impacts the estimated pharmacokinetic parameters, and
therefore allows necessary adjustments to be made to control
the error.
|
|
0190.
 |
9 |
Model Evolution Concept in Dynamic Contrast Enhanced MRI for
Prediction of Tumor Interstitial Fluid Pressure -
Video Not Available
Hassan Bagher-Ebadian1,2, Azimeh NV Dehkordi3,
Rasha Alamgharibi2, Tavarekere Nagaraja1,
David Nathanson1, Hamid Soltanian-Zadeh1,
Stephen Brown1, Hamed Moradi4, Ali
Arbab5, and James R Ewing1,2
1Henry Ford Hospital, Detroit, MI, United States, 2Oakland
University, Rochester, MI, United States, 3Shahid
Beheshti University, Tehran, Iran, 4Tarbiat
Modares University, Tehran, Iran, 5Georgia
Regents University, Augusta, GA, United States
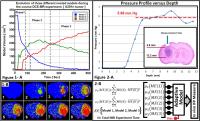
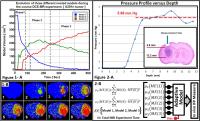
In this study, three physiologically nested models (NM) are
derived from the standard Tofts model to describe possible
physiological conditions of underlying tissue pathology.
Then, using NM selection technique, Model Evolution (ME)
concept is framed to quantify the evolutions of 3 different
model volumes throughout the course of Dynamic Contrast
Enhanced MRI experiment. We hypothesized that three
evolutionary profiles in the course of DCE-MRI experiment
generated from the ME concept, highly depend on the inward
diffusion and outward convection of CA concentration and
contain abundant information for describing the mechanical
properties of solid tumors such as Interstitial Fluid
Pressure (IFP).
|
|
0191.
 |
10 |
Automation of Pattern Recognition Analysis of Dynamic
Contrast-Enhanced MRI Data to Assess the Tumor Microenvironment 
SoHyun Han1, Radka Stoyanova2, Jason
A. Koutcher3, HyungJoon Cho1, and
Ellen Ackerstaff3
1Ulsan National Institute of Science and
Technology, Ulsan, Korea, Republic of, 2Miller
School of Medicine, University of Miami, Miami, FL, United
States, 3Memorial
Sloan Kettering Cancer Center, New York, NY, United States
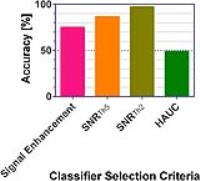
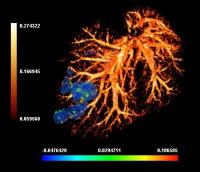
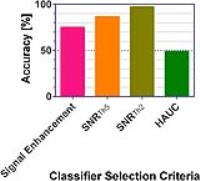
Recently, a novel pattern recognition (PR) approach has been
developed, identifying extent and spatial distribution of
tumor microenvironments based on tumor vascularity. Here,
our goal is to develop methods to minimize user intervention
and errors from model-based approaches by introducing an
automated algorithm for determining the number of
classifiers. An SNR approach showed the highest accuracy at
~97% along five different tumor cell models with 104 slices
total. The visualization of tumor heterogeneity (perfusion,
hypoxia, necrosis) with automated analysis of DCE-MRI can
reduce the need for manual expert intervention, extensive
pharmacokinetic modeling, and could provide critical
information for treatment planning.
|
|
0192.
 |
11 |
In vivo measurement of tumor T1 relaxation time using a whole
body clinically feasible multiple flip angle method can predict
response to chemotherapy 
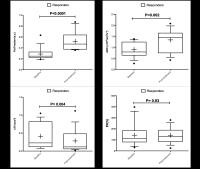
Harbir Singh Sidhu1, Anna Barnes2,
Nikolaos Dikaios1, Scott Rice1, Alan
Bainbridge3, Robert Stein4, Sandra
Strauss5, David Atkinson1, Stuart
Taylor1, and Shonit Punwani1
1Centre for Medical Imaging, University College
London, London, United Kingdom, 2Institute
of Nuclear Medicine, University College London Hospital,
London, United Kingdom, 3Medical
Physics and Biomedical Engineering, University College
London Hospital, London, United Kingdom, 4Medical
Oncology, University College London Hospital, London, United
Kingdom, 5Research
Department of Oncology, University College London, London,
United Kingdom
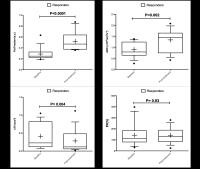
Tumor response assessment currently relies upon measurement
of size change, which may not alter significantly early
during treatment or at all with newer therapies. Patients
may therefore incur significant side-effects (with
associated healthcare cost) without benefit. Assessment of
soft tissue tumor T1 relaxation times before and early
during treatment can predict lesion response whilst being
incorporated within a clinically feasible whole-body MRI
scan duration. Tumors undergoing partial response at the end
of treatment demonstrated significant reduction in T1 values
early during therapy compared to non-responding lesions.
In the future, this could facilitate early response
assessment and complement other imaging biomarkers.
|
 |
0193.
 |
12 |
Quantitative Susceptibility Mapping to Interrogate Colorectal
Metastases in Mouse Liver during Normoxia and Hyperoxia 
Eoin Finnerty1, Rajiv Ramasawmy2,
James O'Callaghan2, Mark F Lythgoe2,
Karin Shmueli1, David L Thomas3, and
Simon Walker-Samuel2
1Medical Physics and Biomedical Engineering,
University College London, London, United Kingdom, 2University
College London, London, United Kingdom, 3Institute
of Neurology, University College London, London, United
Kingdom
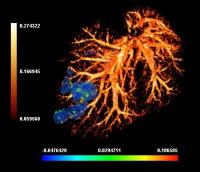
This work examines the application of Quantitative
Susceptibility Mapping (QSM) in a mouse model of colorectal
liver metastases. It was hypothesised that QSM could provide
a novel method of interrogation of liver tumours based on
differences in blood oxygenation. Results under hyperoxic
and normoxic conditions were compared to assess the response
of the liver tissue and tumours. A vascular disrupting agent
was then administered to assess its effect on the QSM
measurements. A significant difference was found between
liver and tumour tissue, and regional differences in
susceptibility were found within a tumour. These differences
were less apparent after VDA administration.
|
 |
0194.
 |
13 |
Early Brain Tumor Detection by Active-Feedback MRI - Permission Withheld
Zhao Li1, Chaohsiung Hsu1, Ryan Quiroz1,
and Yung-Ya Lin1
1Department of Chemistry and Biochemistry, UCLA,
Los Angeles, CA, United States
Early detection of high-grade malignancy, such as
glioblastoma multiforme (GBM), using enhanced MRI techniques
significantly increases not only the treatment options
available, but also the patients’ survival rate. For this
purpose, a conceptually new approach, termed
“Active-Feedback MRI”, was developed. An active feedback
electronic device was homebuilt to implement active-feedback
pulse sequences to generate avalanching spin amplification
and fixed-point spin dynamics, which enhances the local
magnetic-field gradient variations due to irregular water
contents and deoxyhemoglobin concentration in early GBM.
Statistical results (N=22) for in vivo orthotopic xenografts
GBM mouse models at various cancer stages validate the
superior contrast and robustness of this approach (tumor
time constant differs from that of the healthy brain tissue
by +24%) towards early GBM detection than conventional
T1-weighted (+2.6%) and T2-weighted images (-3.1%). This
novel approach provides 4-8 times of improvements in early
GBM tumor contrast, as measured by "tumor to normal tissue
contrast", “contrast-to-noise ratio” (CNR) or “Visibility”.
|
|
0195.
 |
14 |
In Vivo Conductivity Imaging of Rat Tumor Model Using MRI 
Jiaen Liu1, Qi Shao1, Yicun Wang1,
Gregor Adriany2, John Bischof3,
Pierre-Francois Van de Moortele2, and Bin He1,4
1Biomedical Engineering, Univeristy of Minnesota,
Minneapolis, MN, United States, 2Center
for Magnetic Resonance Research, Univeristy of Minnesota,
Minneapolis, MN, United States, 3Mechanical
Engineering, Univeristy of Minnesota, Minneapolis, MN,
United States, 4Institute
for Engineering in Medicine, Univeristy of Minnesota,
Minneapolis, MN, United States
Noninvasive in vivo imaging of the tissue conductivity has
great potential in cancer diagnosis. Recently, electrical
properties tomography (EPT) has been investigated with
increasing effort to noninvasively image tissue conductivity
in vivo using MRI. A preclinical method for imaging tumor
conductivity can be valuable for understanding tumor
development and associated conductivity change due to
fundamental molecular and cellular reasons. In this study,
tumor conductivity was studied based on a xenograft rat
tumor model using a small animal EPT system. The result
showed elevated conductivity in cancerous tissue compared to
healthy tissue, suggesting the clinical value of EPT for
tumor diagnosis.
|
|
0196.
 |
15 |
Evaluation of T2W MRI-derived Textural Entropy for Assessment of
Prostate Cancer Aggressiveness 
Gabriel Nketiah1, Mattijs Elschot1,
Eugene Kim 1,
Tone Frost Bathen 1,
and Kirsten Margrete Selnæs1
1Department of Circulation and Medical Imaging,
Norwegian University of Science and Technology, Trondheim,
Norway
The complexity of the prostatic tissue requires sensitive,
accurate and reproducible assessment methods for
aggressiveness of prostatic carcinomas, especially in
differentiating between Gleason score 3+4 and 4+3 tumors. We
evaluated the applicability of T2W MRI-derived textural
entropy as a potential marker for assessing prostate cancer
aggressiveness. Our study found textural entropy to
correlate moderately positive and negative with Gleason
score and apparent diffusion coefficient (ADC),
respectively. T2W image textural entropy differentiated
Gleason score 3+4 and 4+3 tumors with higher accuracy than
other MRI-derived parameters (ADC, Ktrans and
Ve), indicating the potential of MRI texture
analysis in prostate cancer assessment.
|
|