10:45
|
|
What Makes for a Clinically Useful MR Exam? 
Scott Reeder1
1University of Wisconsin, Madison, WI, United
States
Development, validation, and translation of advanced new
imaging methods is an exciting and important area of
scientific development and clinical medicine. The
development of standardized approaches and objective
measures of new imaging technologies such as SNR and CNR,
and subjective ordinal metrics are extremely helpful
particularly in the early stages of technical
development and translation. Subsequent studies
comparing new imaging techniques with accepted reference
standards, is the next step to establish the diagnostic
performance of a technique for the detection and staging
of disease. Ultimately, clinical effectiveness and
patient outcomes are the most important metric of the
impact of new technologies. Finally, there are many
practical barriers that should be considered, including
work flow, post-processing, that are needed to garner
acceptance by technologists, radiologists, and referring
physicians.
|
11:10
|
|
From k-Space to Pasteur’s Quadrant: Your Research Can Make
the World a Better Place 
Richard L Ehman1
1Radiology, Mayo Clinic, Rochester, MN,
United States
The ISMRM has launched the “MR Value Initiative”, to
encourage innovative optimization the value of
MR-based diagnostic technologies. Both the numerator
(clinical benefit) and the denominator (cost) of the
value ratio can be targeted by scientific and technical
innovation. Studies have shown that investigators in
medical imaging generate innovations at a high rate, and
that these inventions can often be readily translated,
with extraordinary impact on patient care. This
presentation focuses on identifying time-tested
strategies that aspiring innovators can use to improve
the chances that their work will have an impact and
perhaps make the world a better place.
|
11:35
|
|
Panel Discussion |
11:45
|
0086.
 |
Reperfusion beyond 6 hours impacts Tissue Fate of Moderate
Ischemia 
Hongyu An1, Andria L Ford2, Cihat
Eldeniz1, Yasheng Chen2, Katie D
Vo3, Hongtu Zhu4, William J Powers5,
Weili Lin6, and Jin-Moo Lee2
1Washington University in St. Louis, St.
Louis, MO, United States, 2Neurology,
Washington University in St. Louis, St. Louis, MO,
United States, 3Radiology,
Washington University in St. Louis, St. Louis, MO,
United States, 4Biostatistics,
University of North Carolina At Chapel Hill, Chapel
Hill, NC, United States, 5Neurology,
University of North Carolina At Chapel Hill, Chapel
Hill, NC, United States, 6Radiology,
University of North Carolina At Chapel Hill, Chapel
Hill, NC, United States
The fate of mild to moderate ischemic tissue is greatly
impacted by both hyperacute (3-6 hr) and acute (6-24hr)
perfusion changes. Thus, such regions could be targeted
for intervention beyond current treatment windows.
|
11:57
 |
0087.
 |
Cost Effectiveness of MRI Before Prostate Biopsy 
Shivani Pahwa1, Nicholas Schiltz2,
Lee Ponsky3, Ziang Lu1, Sara
Dastmalchian1, Robert Abouassaly3,
Mark Griswold4, and Vikas Gulani5
1Radiology, Case Western Reserve University,
Cleveland, OH, United States, 2Epidemiology
and Biostatistics, Case Western Reserve University,
Cleveland, OH, United States, 3Urology,
Case Western Reserve University, Cleveland, OH, United
States, 4Radiology
and Biomedical Engineering, Case Western Reserve
University, Cleveland, OH, United States, 5Radiology,
University Hospitals Case Medical Center, Cleveland, OH,
United States
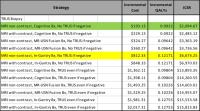
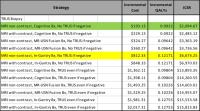
The perception that MRI inflates health care costs
impedes its incorporation into prostate cancer treatment
algorithms, despite robust evidence of its accuracy. We
evaluated the cost effectiveness of 13 different
strategies using a decision tree model in which MRI is
performed before non-targeted, transrectal ultrasound
guided prostate (TRUS) biopsy. Our results show that MRI
is cost effective in each of these strategies, and also
adds incremental quality adjusted life years (QALY) to
the patient over and above the standard practice of
performing non-targeted TRUS biopsy.
|
12:09
|
0088.
 |
Progress towards Robust Spiral MRI for Rapid Brain Exams 
James Grant Pipe1, Ashley Gould Anderson1,
Akshay Bakhru2, Zhiqiang Li1,
Suthambhara Nagaraj2, Melvyn B Ooi3,
Ryan K Robison1, Dinghui Wang1,
and Nicholas R Zwart1
1Imaging Research, Barrow Neurological
Institute, Phoenix, AZ, United States, 2MRI,
Philips Healthcare, Bangalore, India, 3MRI,
Philips Healthcare, Phoenix, AZ, United States
This work gives an overview of an effort to build the
infrastructure for rapid, robust clinical Spiral MRI of
the brain. The current goal is to achieve comparable or
better Image quality than conventional scans with
reduced overall scan time. A long-term (future) goal is
to achieve a comprehensive high-quality brain MR exam in
5 minutes.
|
12:21
|
0089.
 |
The value of MRI in Traumatic Brain Injury: experiences in
the Collaborative European NeuroTrauma Effectiveness
Research in TBI study 
Pim Pullens1, Andrew IR Maas2,
David Menon3, Wim van Hecke4, Jan
Verheyden4, Lene Claes4, Paul M
Parizel1, and On behalf of CENTER-TBI
participants and investigators5
1Radiology, Antwerp University Hospital &
University of Antwerp, Antwerp, Belgium, 2Neurosurgery,
Antwerp University Hospital & University of Antwerp,
Antwerp, Belgium, 3Anaesthesia,
University of Cambridge, Cambridge, United Kingdom, 4icometrix
NV, Leuven, Belgium, 5University
Hospital Antwerp, Antwerp, Belgium
Traumatic Brain Injury (TBI) is regarded as “the most
complex disease in our most complex organ”. Clinical
outcome is unpredictable, especially in repetitive mild
TBI, in terms of behavior, cognition, emotion and
associated long-term effects such as dementia. The
Collaborative European NeuroTrauma Effectiveness
Research in TBI (CENTER-TBI) study is a pan-European
prospective longitudinal observational study aiming to
improve care for TBI patients. One of the key goals is
to improve the quality of imaging-derived data by the
application of a clinical standardized MR imaging
protocol including structural, SWI, DTI and rs-fMRI,
across up to 25 clinical sites in a large, heterogeneous
sample of TBI patients. Harmonization of these protocols
has been a challenging task. As data collection is
underway, 265 datasets have been inspected for quality.
Data quality is variable across sites and scanners. In
order for such large-scale observational studies to be
really effective, sequence harmonization and
standardization is of key importance, but lacking at the
moment.
|
12:33
|
0090.
 |
Capturing clinical MRI complexity: a first step towards
realizing the maximum research value of neuroradiological
MRI. 
Marzena Wylezinska-Arridge1, Mark J White1,2,
Indran Davagnanam1, M Jorge Cardoso3,
Sjoerd B Vos3,4, Sebastien Ourselin3,
Olga Ciccarelli5, Tarek Yousry1,
and John Thornton1,2
1Neuroradiological Academic Unit, UCL
Institute of Neurology, University College London,
London, United Kingdom, 2Lysholm
Department of Neuroradiology, National Hospital for
Neurology and Neurosurgery, London, United Kingdom, 3Translation
Imaging Group, Centre for Medical Imaging Computing,
University College London, London, United Kingdom, 4MRI
Unit, Epilepsy Society, Chalfont, St Peters, United
Kingdom,5Institute of Neurology, University
College London, London, United Kingdom
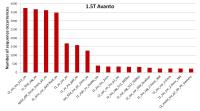
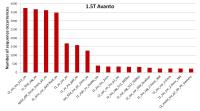
The huge number of hospital MRI examinations routinely
obtained for clinical purposes offers a potentially
valuable “big data” resource for largescale experimental
neurology. However, acquisition-scheme variation may
compromise the research value of clinical imaging data.
A first step towards reducing variation by prospective
protocol harmonization is to systematically capture
sequence-use statistics. Using an in-house tool
developed to automate capture of long-term, MRI sequence
deployment statistics in routine practice within our
neuroradiological service, we identified “core“, most
used sequences and the deployment frequency of their
respective variants, to enable efficient, targeted
protocol harmonization.
|
12:45
|
|
Adjournment & Meet the
Teachers |
|