Prostate
Oral
Body: Breast, Chest, Abdomen, Pelvis
Wednesday, 20 June 2018
| S04 |
08:15 - 10:15 |
Moderators: Winfried Willinek, Valeria Panebianco |
08:15
|
0713.
 |
 Four-dimensional T2-weighted imaging in prostate MRI with T2 shuffling Four-dimensional T2-weighted imaging in prostate MRI with T2 shuffling
Albert Roh, Jonathan Tamir, Jamil Shaikh, Kim Vu, Valentina Taviani, Michael Lustig, Shreyas Vasanawala
High-quality T2-weighted imaging is critical in the evaluation of the prostatic transition zone for cancer. We adapted an acquisition technique currently used mostly in musculoskeletal MRI termed T2 Shuffling (T2Sh) by incorporating outer volume suppression (OVS) and optimizing it for the prostate. Our retrospective review of 20 patients assessed T2Sh in the evaluation of the prostate. The overall image quality of T2Sh was comparable to that of 2D T2 FSE with water-fat separation and superior to that of 3D T2 FSE with OVS and water-fat separation.
|
08:27
|
0714.
 |
 Added value of magnetic resonance spectroscopic imaging to multiparametric MRI for detection of prostate cancer using PIRADS version 2 Added value of magnetic resonance spectroscopic imaging to multiparametric MRI for detection of prostate cancer using PIRADS version 2
Virendra Kumar, Vivek Lanka, Sanjay Sharma, Rishi Nayyar, Chandan Das
We report increase in sensitivity, specificity and accuracy of PIRADSv2 by addition of MRSI to mpMRI protocol for detection of cancer of prostate (CaP). 26 patients having a biopsy-proven CaP, were investigated at 3.0T using mpMRI including MRSI, followed by radical prostatectomy within 1 month. PIRADSv2 score for mpMRI, PIRADSv1 score for MRSI and Gleason grade group from radical prostatectomy specimens were determined. ROC curve analysis was used to determine the accuracy for cut-offs. A combination of MRSI PIRADSv1 cut-off ≥4 and PIRADSv2 cut-off ≥3 showed the best accuracy (96.2%) for CaP detection. When MRSI was added to PIRADSv2 scoring we found an improvement from 71.4% sensitivity and 91.9% specificity of PIRADSv2 to 91.8% sensitivity and 98% specificity for detecting CaP.
|
08:39
|
0715.
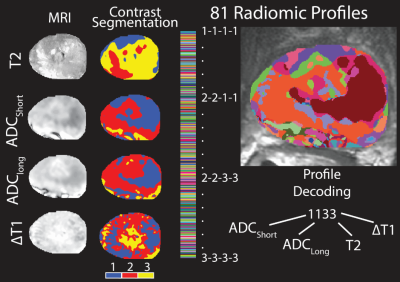 |
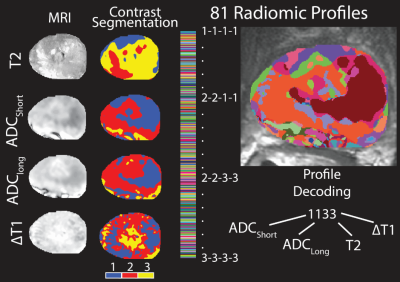
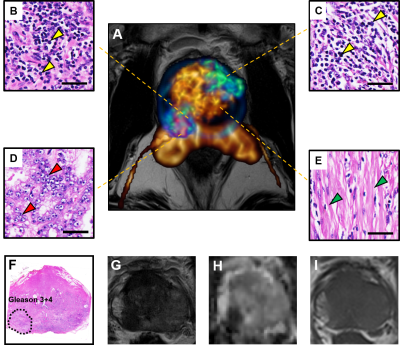
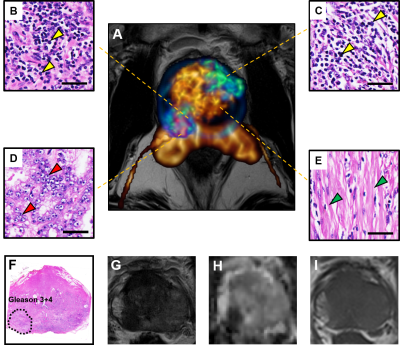
 Gleason Probability Maps: A Radiomics Tool for Mapping Tumor Likelihood in MRI Space Gleason Probability Maps: A Radiomics Tool for Mapping Tumor Likelihood in MRI Space
Sean McGarry, Sarah Hurrell, Mark Hohenwalter, Petar Duvnjak, Michael Griffin, Kenneth Iczkowski, Kenneth Jacobsohn, Andrew Nencka, Peter LaViolette
Intra and intertumoral heterogeneities are well recognized in prostate cancer. These differences affect the macroscopic imaging contrast characteristics of tumor and surrounding tissue. This study aims to generate three new, interpretable image contrasts by combining radiomic profiling with annotated, whole mount pathology. We show that these new image contrasts, Gleason probability maps, are indicative of prostate cancer in na´ve data.
|
08:51
|
0716.
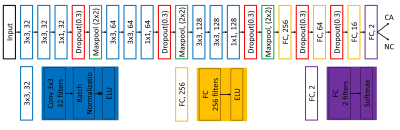 |
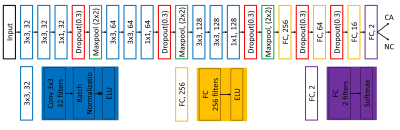
 A Patch-Based Convolutional Neural Network Model for the Diagnosis of Prostate Cancer using Multi-Parametric Magnetic Resonance Images A Patch-Based Convolutional Neural Network Model for the Diagnosis of Prostate Cancer using Multi-Parametric Magnetic Resonance Images
Yang Song, Yu-Dong Zhang, Xu Yan, Bingwen Hu, Guang Yang
We proposed a patch-based convolutional neural network (CNN) model to distinguish prostate cancer using multi-parametric magnetic resonance images (mp-MRI). Our CNN model was trained in 182 patients including 193 cancerous (CA) vs. 259 normal (NC) regions, and tested independently in 21 patients including 21 CA vs 31 NC regions. The model produced an area under the receiver operating characteristic curve of 0.869, sensitivity of 90.5% and specificity of 67.7% for the differentiation of CA from normal regions, showing its potential for the diagnosis of prostate cancer in clinical application.
|
09:03
|
0717.
 |
 Delineation accuracy of prostate cancer for focal therapy: comparison of MR imaging and histopathology characteristics Delineation accuracy of prostate cancer for focal therapy: comparison of MR imaging and histopathology characteristics
Petra van Houdt, Ghazaleh Ghobadi, Stijn Heijmink, Ivo Schoots, Jeroen de Jong, Iris Walraven, Henk van der Poel, Floris Pos, Susanne Rylander, Lise Bentzen, Karin Haustermans, Uulke van der Heide
The success of any focal therapy for prostate cancer relies on accurate tumor detection and delineation. Currently there are no guidelines for delineation of prostate tumors. In this study we showed that radiologists are better in delineating parts of tumors with Gleason pattern 4 and 5 than Gleason pattern 3, but still the sensitivity (0.56) needs to be improved for focal therapy and volume estimation.
|
09:15
|
0718.
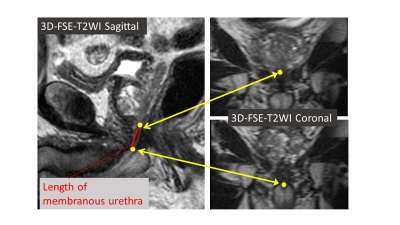 |
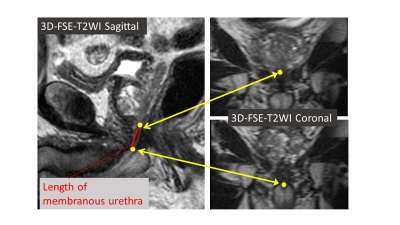
 Measurement using 3D-FSE-T2WI is useful in predicting early recovery of continence following radical prostatectomy in patients with prostate carcinoma. Measurement using 3D-FSE-T2WI is useful in predicting early recovery of continence following radical prostatectomy in patients with prostate carcinoma.
Tatsuya Shimizu, Utaroh Motosugi, Satoshi Funayama, Takahiko Mitsui, Masayuki Takeda, Hiroshi Onishi
We conducted a prospective study to examine if preoperative anatomical evaluation of the urethra using 3D-FSE-T2WI is useful in predicting early recovery of continence following total prostatectomy in patients with prostate carcinoma. The length of the membranous urethra (8.4▒1.7 mm vs. 5.7▒0.6 mm, p=0.005) and the thickness of the pelvic diaphragm (10.8▒1.4 mm vs. 8.8▒0.5 mm, p=0.01) were significantly different between the patients who achieved continence and those who did not achieve continence 1 month after surgery. A longer membranous urethra and thicker pelvic diaphragm measured using 3D-FSE-T2WI are correlated to earlier recovery of continence following radical prostatectomy.
|
09:27
|
0719.
|
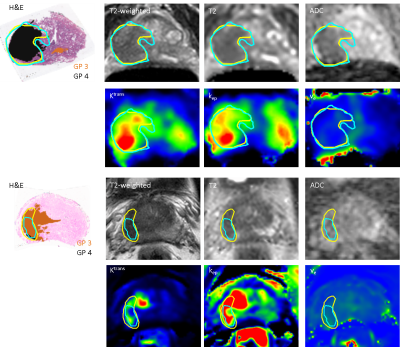
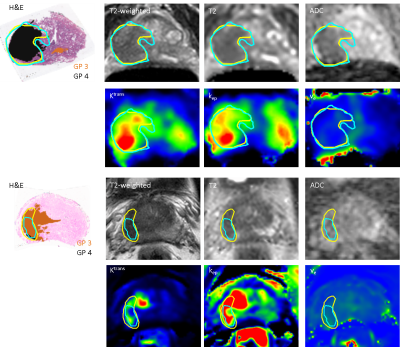
 How to improve the equivocal category PI-RADS score 3? Quantitative multiparametric MRI assessment of prostate cancerous and non-cancerous areas using correlative histopathology. How to improve the equivocal category PI-RADS score 3? Quantitative multiparametric MRI assessment of prostate cancerous and non-cancerous areas using correlative histopathology.
Giovanni Barchetti, Martina Pecoraro, Isabella Ceravolo, Maurizio Del Monte, Carlo Catalano, Valeria Panebianco
To stratify patients with PI-RADSv2 category 3 to define the correct diagnostic work-up (biopsy or follow-up), quantitatively analyzing mpMRI parameters (ADC, k-trans, K-ep and ve). Among 1272 men who underwent mpMRI, we retrospectively enrolled 98 patients treated with radical prostatectomy. Furthermore, we selected 100 negative patients. The 198 mpMRI exams were randomly, blindly reviewed by two radiologists. 95 PI-RADSv2 category 3 were found and quantitatively analyzed. ROC and AUC were determined to identify a cut-off value to define which PI-RADS 3 lesion should be biopsied. Quantitative imaging represents a tool to objectively stratify patients classified as PI-RADSv2 category 3.
|
09:39
|
0720.
 |
 Patient-Specific 3D Printed and Augmented Reality Prostate Cancer Models Derived from MRI Data: Initial Results from Prospective Clinical Study Patient-Specific 3D Printed and Augmented Reality Prostate Cancer Models Derived from MRI Data: Initial Results from Prospective Clinical Study
Nicole Wake, Andrew Rosenkrantz, William Huang, Samir Taneja, James Wysock, Marc Bjurlin, Richard Huang, Daniel Sodickson, Hersh Chandarana
The objective of this study was to determine whether patient-specific 3D printed and augmented reality prostate cancer models derived from multi-parametric MRI data can influence pre-surgical planning and patient outcomes for patients undergoing robotic assisted radical prostatectomy. Initial results from our prospective study are presented.
|
09:51
|
0721.
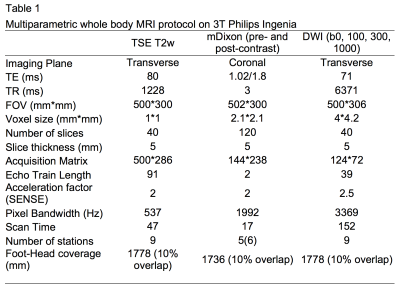 |
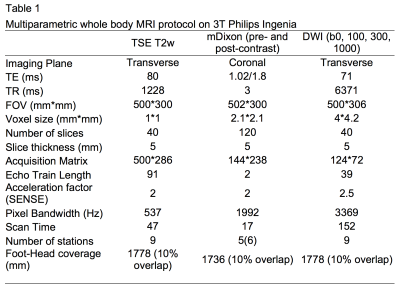
 Quantitative mDixon Fat Fraction can differentiate metastatic nodes from benign nodes in prostate cancer patients. Quantitative mDixon Fat Fraction can differentiate metastatic nodes from benign nodes in prostate cancer patients.
Mrishta Brizmohun Appayya, James O’Callaghan, Arash Latifoltojar, Edward Johnston, Harbir Sidhu, Abdulrhman Alnaim, Asim Afaq, Jamshed Bomanji, Alan Bainbridge, Shonit Punwani
Metastatic nodes in prostate cancer are associated with poor prognosis. Conventional MRI, relying on short-axis diameter (SAD) suffers from poor accuracy in identifying metastatic nodes. In this study, we compare fat fraction signal from MRI mDixon acquisitions (FF) with apparent diffusion coefficients of nodes and quantitative contrast-enhanced two-point mDixon T1 images (CE-mDixon), in discriminating between benign and metastatic nodes using 18F-Choline PET-CT as reference standard. We showed that FF and CE-mDixon discriminate benign from involved lymph nodes that are small in size unlike SAD or ADC of nodes; FF, not necessitating contrast agents, holds promise as a clinical tool.
|
10:03
 |
0722.
 |
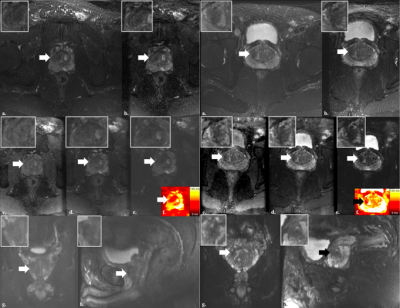
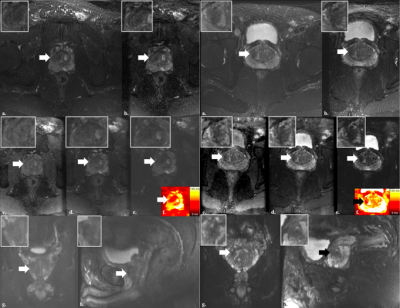
 Diffusion MRI Detects and Differentiates Inflammation from Cancer Cells in Prostate Cancer Patients Diffusion MRI Detects and Differentiates Inflammation from Cancer Cells in Prostate Cancer Patients
Zezhong Ye, Qingsong Yang, Joshua Lin, Jeff Viox, Peng Sun, Joesph Ippolito , Jianping Lu, Sheng-Kwei Song
Recent consensus suggested PCa detection based on mpMRI lacks necessary sensitivity or specificity to differentiate prostatitis from PCa, which results in over-diagnosis and over-treatment. Our novel method, diffusion MRI histology (D-Histo), demonstrated its ability to accurately localize, quantify and distinguish between PCa and prostatitis. D-Histo’s improved diagnosis accuracy could more effectively guide treatment planning and assess treatment efficacy.
|
|