|
Osteoarthritis: The (W)Holy Grail
Combined Educational & Scientific Session
ORGANIZERS: Edwin Oei, Jung-Ah Choi, Emily McWalter, Miika Nieminen
Tuesday, 19 June 2018
| S01 |
13:45 - 15:45 |
Moderators: Miika Nieminen, Jung-Ah Choi |
Skill Level: Intermediate
Session Number: Tu-05
Overview
In this session current whole-organ concepts in osteoarthritis (OA) will be discussed, emphasizing the variety of joint tissues that are affected. Changes in these tissues due to OA are reviewed along with their appearance on morphological MRI sequences as well as quantitative MRI techniques.
Target Audience
Researchers and clinicians with an interest in MR imaging of osteoarthritis.
Educational Objectives
As a result of attending this course, participants should be able to:
-Describe which joint tissues are predominantly involved in osteoarthritis according to the whole-organ concept of osteoarthritis;
-Identify the most important osteoarthritis-induced morphological changes in various joint tissues on MRI; and
-Describe the advantages of quantitative MRI techniques to assess tissue changes in osteoarthritis.
13:45
|
|
 Physiology of Joint Tissues in Osteoarthritis Physiology of Joint Tissues in Osteoarthritis
James MacKay
|
14:15
|
|
 Whole Joint Imaging of Osteoarthritis with Morphological & Quantitative MRI Whole Joint Imaging of Osteoarthritis with Morphological & Quantitative MRI
Ashley Williams
Imaging tools are needed to detect and stage joint status early enough in the disease process that osteoarthritis modifying interventions might have a chance. The purpose of this talk is to introduce MRI methods for morphologic and quantitative evaluation of osteoarthritis of the knee. Compositional MRI measures of OA will also be discussed.
|
14:45
|
0458.
 |
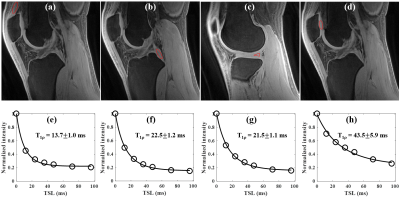
 Three Dimensional Adiabatic T1rho Prepared Ultrashort Echo Time Cones (3D AdiabT1rho UTE-Cones) Sequence for Whole Knee Imaging Three Dimensional Adiabatic T1rho Prepared Ultrashort Echo Time Cones (3D AdiabT1rho UTE-Cones) Sequence for Whole Knee Imaging
Yajun Ma, Michael Carl, Adam Searleman , Xing Lu, Eric Chang, Jiang Du
To propose a combination of a three dimensional ultrashort echo time sequence employing cones trajectories with an AdiabT1rho preparation (3D AdiabT1rho UTE-Cones) for volumetric T1rho assessment of both short and long T2 tissues in the knee joint on a clinical 3T scanner. Simulation, phantom, ex vivo and in vivo studies were carried out in this feasibility study.
|
14:57
 |
0459.
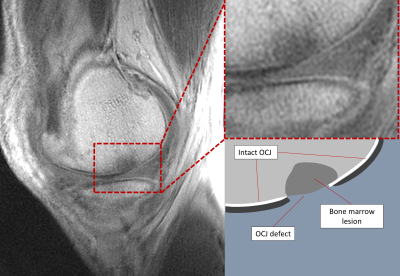 |
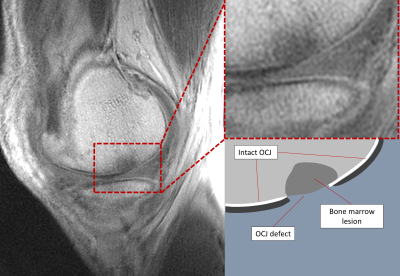
 Ultrashort Echo Time Imaging of the Osteochondral Junction in Subjects with Knee Osteoarthritis and Age-matched Healthy Volunteers Ultrashort Echo Time Imaging of the Osteochondral Junction in Subjects with Knee Osteoarthritis and Age-matched Healthy Volunteers
James MacKay, Josh Kaggie, Alexandra Morgan, Robert Janiczek, Scott Reid, Stephen McDonnell, Wasim Khan, Martin Graves, Fiona Gilbert, Andrew McCaskie
We describe in vivo translation of ultrashort TE (UTE) imaging of the osteochondral junction (OCJ) at the knee in 9 subjects with osteoarthritis (OA) and 4 age-matched healthy volunteers. The OCJ plays an important role in onset and progression of OA. Our study demonstrates that UTE imaging of the OCJ is repeatable and demonstrates OCJ defects in OA subjects but not in healthy volunteers. Areas of OCJ damage commonly co-locate to other osteochondral pathology (bone marrow lesions and cartilage defects). UTE imaging of the OCJ may be a helpful tool for assessing OCJ damage in clinical studies of OA.
|
15:09
|
0460.
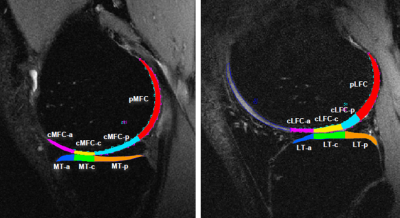 |
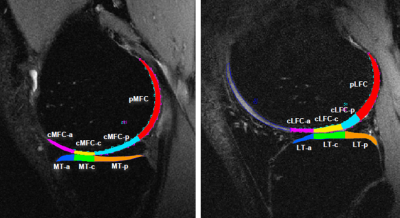
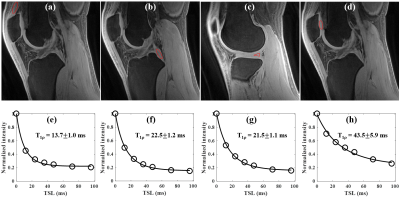
 T1? and T2 of articular cartilage and medial meniscus at baseline and 6-month can predict the degenerative changes of cartilage at 3 years after ACL reconstruction T1? and T2 of articular cartilage and medial meniscus at baseline and 6-month can predict the degenerative changes of cartilage at 3 years after ACL reconstruction
Kenji Mamoto, Kaipin Xu, Tomohiro Shimizu, Matthew Tanaka, Alexander Markes, Valentina Pedoia, C. Benjamin Ma, Xiaojuan Li
Patients with anterior cruciate ligament (ACL) injury have a high risk of development of early post-traumatic osteoarthritis (PTOA) even after ACL reconstruction. The aim of this study was to investigate the risk factors that may predict the longitudinal cartilage degeneration by using MR T1ρ/T2 imaging. The first 6-month changes of T1ρ/T2 values of the cartilage and anterior horn of medial meniscus significantly correlated with the 3-year cartilage degenerative change after ACL reconstruction. And also, T2 values of the posterior horn of medial meniscus prior to surgery significantly correlated with the cartilage degeneration of anterior medial tibia 3-year after the reconstruction.
|
15:21
|
0461.
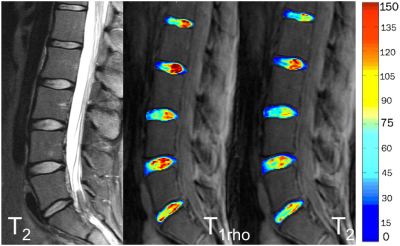 |
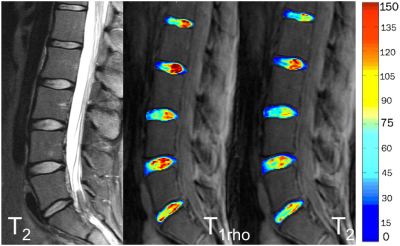
 Quantitative Assessment of Disc Biochemical Composition and Vertebral Body Fat in Patients with Low Back Pain Quantitative Assessment of Disc Biochemical Composition and Vertebral Body Fat in Patients with Low Back Pain
Roland Krug, Misung Han, Aaron Fields, Gabby Joseph, Justin Cheung, Maya Mundada, Alice Rochette, Jeannie Bailey, Alexander Ballatori, Thomas Link, Zachary McCormick, Conor O'Neill, Jeffrey Lotz
We present a cross sectional study of 53 subjects with chronic lower back pain (n=39) and healthy controls (n=14). We have assessed disc biochemical composition (T1rho and T2 mapping) and vertebral bone marrow fat (6-point chemical-shift based imaging) as well as Pfirrmann grading. We have found significant associations between mean and standard-deviation of T1rho and T2 with vertebral bone marrow fat content in the adjacent vertebral body. We have also found strong associations of T1rho and T2 with clinical Pfirrmann grading.
|
15:33
|
0462.
 |
 New Diffusion Tensor and Dixon Imaging Results in Human Skeletal Muscle from the GESTALT Longitudinal Study of Aging New Diffusion Tensor and Dixon Imaging Results in Human Skeletal Muscle from the GESTALT Longitudinal Study of Aging
Donnie Cameron, David Reiter, Fatemeh Adelnia, Kenneth Fishbein, Christopher Bergeron, Richard Spencer, Luigi Ferrucci
This work investigates how aging influences skeletal muscle diffusion tensor imaging (DTI) measures in a healthy cohort with a broad age range. Sixty participants, from 23-87 years old, were recruited and tract-based DTI indices were calculated in their thigh quadriceps muscles. Through piecewise regression, we identified trends in DTI indices and Dixon fat measures with respect to age, including a previously undocumented decline in fractional anisotropy (FA) in older age, particularly in men (r=-0.46, p=0.06). Our results also show statistically significant differences in FA between quadriceps muscles (p<0.001) that may reflect differences in composition and patterns of use.
|
15:45
|
|
Adjournment & Meet the Teachers |
|