Lung Power
| Power Pitch Session: How it Works | |
|
1st Hour: 2-minute Power Pitches inside the Power Pitch Theater. 2nd Hour: 60-minute Digital Poster Presentations at the numbered plasma screens outside the Power Pitch Theater. |
1st Hour
Pitch: Lung PowerPower Pitch
Body: Breast, Chest, Abdomen, Pelvis
Monday, 13 May 2019
Power Pitch Theater A - Exhibition Hall
08:15 - 09:15
Moderators: Kevin Johnson
2nd Hour
Poster: Lung PowerPower Pitch Poster
Body: Breast, Chest, Abdomen, Pelvis
Monday, 13 May 2019
Power Pitch Theater A - Exhibition Hall
09:15 - 10:15
| Plasma # | |||
 |
0001. 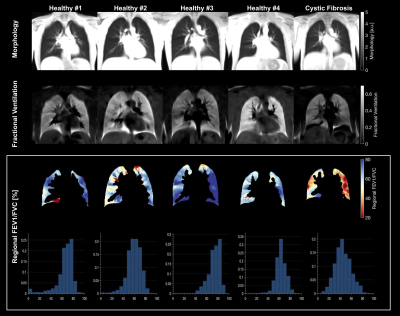 |
1 | FEV1/FVC Mapping with Dynamic MRI - A New Regional Lung Function Test
Andreas Voskrebenzev, Agilo Kern, Lea Behrendt, Filip Klimes, Marcel Gutberlet, Gesa Pöhler, Frank Wacker, Jens Vogel-Claussen
Pulmonary function parameters like the ratio of expiratory volume in one second (FEV1) and forced vital capacity (FVC) are the current gold standard for disease diagnosis and monitoring. However, early disease detection remains limited due to missing regional information. In this study the forced expiratory maneuver was captured with a dynamic MRI acquisition, as used in Fourier decomposition or phase-resolved functional lung imaging (PREFUL), for FEV1/FVC mapping. Results were compared with spirometry, PREFUL and hyperpolarized MRI in four healthy subjects and one patient with cystic fibrosis and suggest a potentially increased sensitivity in comparison with the tidal breathing approach.
|
 |
0002. 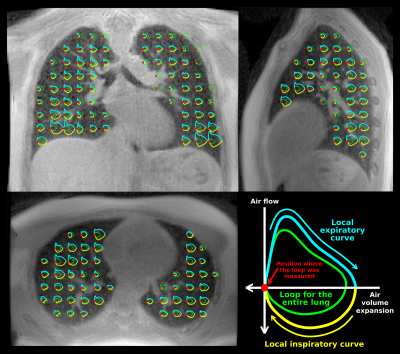 |
2 | 3D Magnetic Resonance Spirometry
Tanguy Boucneau, Brice Fernandez, Peder Larson, Luc Darrasse, Xavier Maître
Spirometry is a routine tool in pulmonology to challenge lung function. It is sensitive and specific to several common lung diseases. Nevertheless, spirometry provides a global measurement at the mouth that only characterizes the pulmonary response as a whole, and cannot specifically address regional affections. We developed a 3D MRI-based technique to non-invasively perform local spirometry throughout the lung. The final outcome is a 3D map with voxel-wise flow-volume loops over the organ. The potential of this technique is demonstrated by its sensitivity to normal, thoracic, and diaphragmatic breathings and its related regional specificity in a healthy subject.
|
 |
0003. 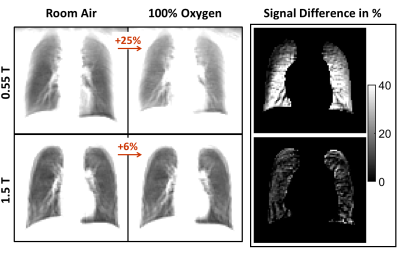 |
3 | Improved lung imaging and oxygen enhancement at 0.55T
Ipshita Bhattacharya, Rajiv Ramasawmy, Delaney McGuirt, Christine Mancini, Robert Lederman, Joel Moss, Marcus Chen, Robert Balaban, Adrienne Campbell-Washburn
Signal dephasing at high field and low proton density, has limited the use of MRI for lung imaging. We revisit the problem, using a low field (0.55T) scanner which, due to low magnetic susceptibility, improves the signal at air-tissue boundaries like lung. Moreover, because oxygen has increased r1 relaxativity at low field, oxygen inhalation can be used to significantly increase lung signal at 0.55T. Combined, these advantages makes lung MRI lucrative at low field. In this abstract we demonstrate oxygen-enhanced lung MRI at 0.55T in healthy volunteers and Lymphangioleiomyomatosis (LAM) patients.
|
 |
0004. 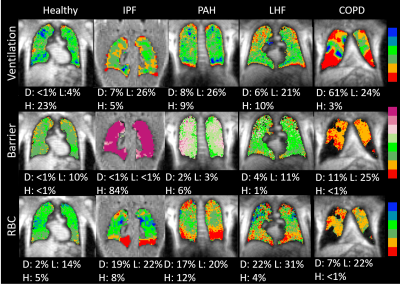 |
4 | Using 129Xenon MR Imaging and Spectroscopic Signatures to Differentiate Pulmonary Arterial Hypertension from Other Cardiopulmonary Diseases
Elianna Bier, Ziyi Wang, Aparna Swaminathan, John Nouls, Mu He, Joseph Mammarappallil, Sheng Lou, Sudarshan Rajagopal, Bastiaan Driehuys
This work sought to identify a non-invasive means to detect pulmonary arterial hypertension (PAH). 129Xenon MRI and dynamic spectroscopy were acquired in healthy volunteers and subjects with chronic obstructive pulmonary disease (COPD), idiopathic pulmonary fibrosis (IPF), left heart failure (LHF), and PAH. COPD was differentiated from PAH by increased ventilation and barrier defects, while IPF was differentiated by increased barrier uptake. PAH and LHF subjects had similar imaging features but could be differentiated by their RBC signal oscillation amplitudes. 129Xe MR imaging and spectroscopy appears capable of differentiating PAH from COPD, IPF, and LHF.
|
 |
0005. 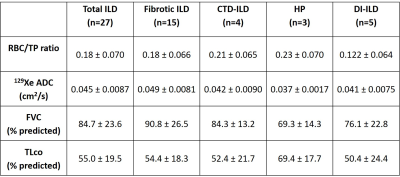 |
5 | Hyperpolarised xenon-129 MR spectroscopy and diffusion-weighted xenon-129 MRI at baseline in patients with interstitial lung disease
James Eaden, Paul Hughes, Ho-Fung Chan, Oliver Rodgers, Guilhem Collier, Graham Norquay, Matthew Austin, Laurie Smith, Jim Lithgow, Nicholas Weatherley, Helen Marshall, Andrew Swift, Stephen Renshaw, Colm Leonard, Sarah Skeoch, Nazia Chaudhuri, Geoff Parker, Stephen Bianchi, Jim Wild
Preliminary findings are presented from a prospective, longitudinal, multicentre MRI biomarker study of patients presenting with interstitial lung disease (ILD) including drug induced ILD, hypersensitivity pneumonitis, idiopathic pulmonary fibrosis and connective tissue disease ILD. At the time of writing, 27 patients have undergone baseline hyperpolarised xenon-129 (129Xe) MR spectroscopy (MRS) and 129Xe diffusion-weighted MRI. Our findings suggest significant differences in mean 129Xe apparent diffusion coefficient between the ILD subtypes at baseline but no significant differences in the red blood cell / tissue plasma ratio from dissolved 129Xe MRS. We also demonstrate correlation between pulmonary function tests and 129Xe MRI measures.
|
 |
0006. 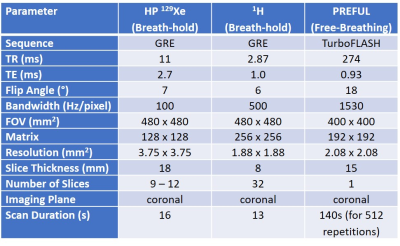 |
6 | Comparison of Phase-Resolved Functional Lung (PREFUL) MRI and Hyperpolarized 129Xe MRI in Pediatric Cystic Fibrosis
Marcus Couch, Jonathan Rayment, Robert Grimm, Andreas Voskrebenzev, Jens Vogel-Claussen, Felix Ratjen, Giles Santyr
Hyperpolarized 129Xe MRI provides robust measurements of ventilatory function through the measurement of the ventilation defect percent (VDP). Recent progress in 1H-based free-breathing techniques (phase-resolved functional lung; PREFUL) allows for the calculation of fractional ventilation maps, which can be similarly processed to calculate VDP. While hyperpolarized 129Xe is an established research technique, PREFUL MRI is simple to implement on any MRI scanner and therefore has good potential for use in future clinical trials in cystic fibrosis (CF). In this study, VDP measurements performed using hyperpolarized 129Xe and PREFUL MRI were compared and correlated with pulmonary function tests in pediatric CF.
|
 |
0007. 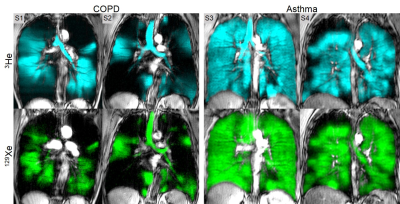 |
7 | Differences Between 3He and 129Xe Ventilation Heterogeneity Explained Using Oscillometry
Rachel Eddy, Andrew Westcott, Geoffrey Maksym, David McCormack, Grace Parraga
129Xe MRI ventilation defects were previously shown to be greater and more numerous than 3He MRI ventilation defects in patients with chronic obstructive pulmonary disease (COPD) and asthma, however the underlying biomechanical explanation for these differences has not been determined. Here we evaluated the relationships of 3He and 129Xe MRI ventilation defect percent (VDP) with oscillometry measurements acquired in patients to better understand the lung biomechanical constraints that lead to such differences. 129Xe VDP was significantly related to total respiratory-system resistance whereas 3He was not which may suggest increased sensitivity of 129Xe to resistance throughout the entire airway tree.
|
 |
0008. 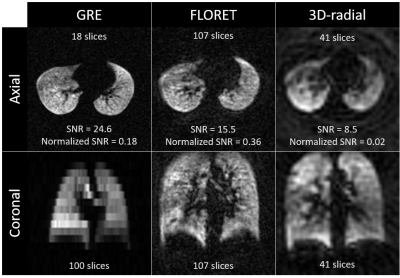 |
8 | Improved Pulmonary 129Xe Ventilation Imaging via 3D-Spiral UTE MRI
Matthew Willmering, Peter Niedbalski, Hui Wang, Laura Walkup, Ryan Robison, James Pipe, Zackary Cleveland, Jason Woods
Functional lung imaging via inhaled hyperpolarized 129Xe MRI has been shown to provide sensitive regional maps of ventilation and gas-exchange. Traditionally, ventilation images are acquired via standard Cartesian or less commonly radial sequences. Previously reported results have shown promise for 2D-spiral sequences with increased SNR and/or shorter acquisition lengths. In this study, a 3D-spiral sequence (FLORET) was implemented and compared to Cartesian, radial, and 2D-spiral acquisition techniques. This is the first implementation and comparison of a 3D-spiral UTE technique to acquire hyperpolarized gas images.
|
 |
0009. 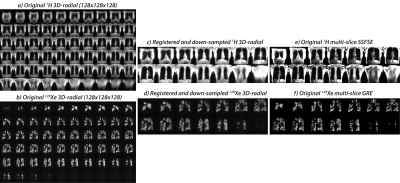 |
9 | The Accuracy of Hyperpolarized 129Xe Ventilation Derived from 3D Radial Gas Exchange MRI versus Multi-Slice Gradient Echo Imaging
Mu He, Ziyi Wang, Leith Rankine, Elianna Bier, John Nouls, Bastiaan Driehuys
Both multi-slice GRE and 3D-radial acquisitions can image regional ventilation in the lungs. Here, we sought to evaluate the accuracy of the ventilation images acquired as part of a 3D-radial gas-exchange acquisition by comparing them with those acquired with a standard GRE acquisition. Linear-binning quantification was applied on both acquisitions to derive the quantitative metrics, through which we found good qualitative and modest pixel-wise agreement between the two ventilation scans. With further reconciliation of bias-field correction and threshold-setting for the 3D-radial pipeline, it could become a one-stop shop for single-breath ventilation and gas exchange imaging.
|
0010. 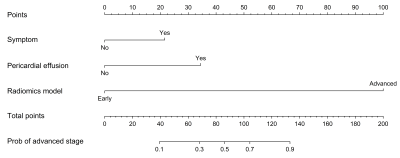 |
10 | MR radiomics analysis in predicting the pathological classification and TNM staging of thymic epithelial tumors Presentation Not Submitted
Gang Xiao, Wei-Cheng Rong, Zhong-Qiang Shi, Xiao-Cheng Wei, Wen Wang, Yu-Chuan Hu, Guang-Bin Cui
To explore the performance of MR radiomics in predicting the pathological classification and staging of thymic epithelial tumors (TETs), we built two radiomics models based on support vector machine. Besides, we developed a radiomics nomogram for predicting risk stratification of advanced TETs. The models achieved an area under the curve of 77.1% or 90.8% in the test cohort in distinguishing low-, high-risk thymomas and thymic carcinomas or early and advanced TETs. The radiomics model, symptom, and pericardial effusion constituted a radiomics nomogram, with a C-index of 0.957 in the test cohort. Thus, MR radiomics can be useful for assessing TETs.
|
|
 |
0011. 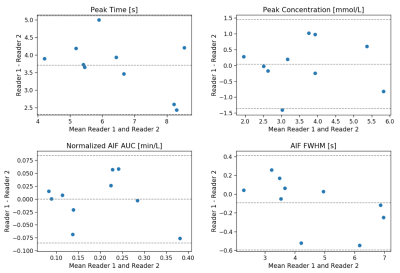 |
11 | Evaluation of automatic methods for arterial input function extraction for perfusion quantification in the lung.
Marta Tibiletti, Josephine Naish, Paul Hughes, Helen Marshall, Colm Leonard, Sarah Skeoch, Nazia Chaudhuri, Ian Bruce, James Eaden, Stephen Bianchi, Jim Wild, Geoff Parker
We developed automatic methods to extract the AIF for lung first pass perfusion DCE and compared their performance with manual selection of an ROI in the pulmonary artery (PA). Dynamic enhancement was calculated by simple subtraction and with a shuffle subtraction. Early enhancing voxels with the highest enhancing values were selected. We demonstrated that the shuffle subtraction is a more robust method, since it avoids including the early enhancing subclavian vein. Our results suggest obtaining the AIF automatically from pixels within the RV may be more robust against partial volume effects and removes inter-reader variability.
|
0012. 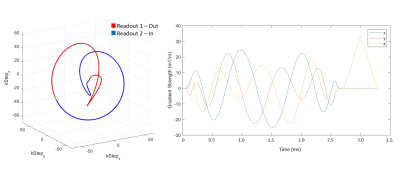 |
12 | 3D UTE Yarn Ball Acquisition MRI for Quantification of Lung Water Content
William Meadus, Richard Thompson, Robert Stobbe, Christian Beaulieu
The goal of this study was to develop and validate a fast, robust and quantitative MRI method for the evaluation of lung water density, for the detection of pulmonary edema. Short lung T2* necessitates ultrashort TE (UTE) acquisitions. We propose a novel optimized UTE Yarn-Ball k-space trajectory that uses ~15% of the pure radial readouts arms required to achieve full sampling. Phantom studies validated accurate water density quantification. A dual-echo approach enabled automated lung tissue segmentation. An optimized Yarn-Ball k-space trajectory yields three-dimensional spin-density weighted lung water images (2.5mm isotropic resolution), without the need for breath-holding, in ~2 minutes.
|
|
 |
0013. 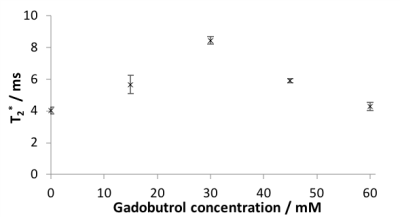 |
13 | Combined ventilation and perfusion imaging using dynamic susceptibility contrast 19F-MRI of inhaled perfluoropropane
Mary Neal, Ben Pippard, A John Simpson, Pete Thelwall
19F-MRI of inhaled perfluoropropane (PFP) can be used to assess pulmonary ventilation. PFP has a short in vivo T2* (~2ms) arising from magnetic field inhomogeneity in the lung, reflecting the different magnetic susceptibilities of adjacent alveolar walls and gas components. Intravenous injection of a paramagnetic contrast agent to the pulmonary circulation can transiently reduce these magnetic susceptibility gradients, raising the T2* of inhaled PFP in regions directly adjacent to well-perfused lung. We present the first in man demonstration of combined pulmonary ventilation and perfusion assessment using 19F-MRI of inhaled PFP with concurrent administration of a gadolinium-based contrast agent.
|
0014. 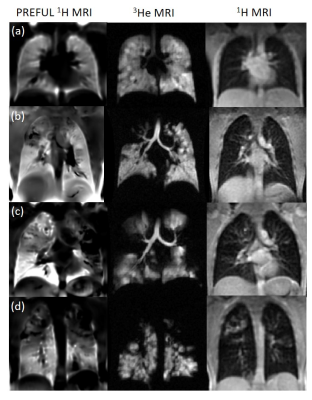 |
14 | Investigating the relationship between free-breathing 1H and breath-hold 3He MRI in patients with cystic fibrosis
Helen Marshall, Andreas Voskrebenzev, Alberto Biancardi, Bilal Tahir, Laurie Smith, Jim Wild, Jens Vogel-Claussen
Free-breathing non-contrast enhanced 1H MRI techniques show promise as a surrogate for ventilation imaging but more validation against methods which directly image lung ventilation is needed in patients. The aim of this work was to investigate the relationship between 1H free-breathing and 3He breath-hold ventilation images in patients with CF. Phase-resolved functional lung (PREFUL) 1H and 3He ventilation images were compared in 10 patients with CF. Qualitative similarities were observed between techniques to varying degrees. Ventilation defect percentage showed strong correlation between methods and with FEV1, although median and inter-quartile range fractional ventilation values were not related.
|
|
0015. 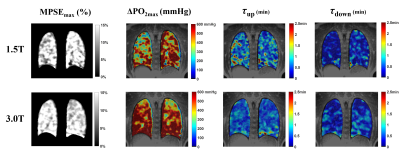 |
15 | Oxygen-enhanced UTE MRI for Quantification of Dynamic Lung Function
Wei Zha, Kevin Johnson, Robert Cadman, Scott Nagle, Sean Fain
Three-dimensional dynamic imaging using free-breathing oxygen-enhanced (OE) ultrashort echo time (UTE) MRI can measure change of partial pressure of oxygen (ΔPO2) and wash-in/out time constants. Nine healthy subjects underwent the dynamic OE MRI protocol at 1.5T. A subset of 4 subjects underwent repeated exams and 2 of these 4 underwent the same protocol at 3.0T on the same day. The inter-exam variations at 1.5T suggest good quantitative measurements of lung function and wash-in/out dynamics with variations observed in ΔPO2max. The parametric maps imply comparable wash-in/out time constants and normal ventilation measured at 1.5T vs. 3.0T.
|
 Back to Program-at-a-Glance |
Back to Program-at-a-Glance |  Back to Top
Back to Top