Muscle Imaging
Muscle Imaging
Combined Educational & Scientific Session
Combined Educational & Scientific Session
ORGANIZERS: Jung-Ah Choi, Riccardo Lattanzi, Emily McWalter, Miika Nieminen, Jan Fritz, Edwin Oei
Tuesday, 14 May 2019
| Room 518A-C | 13:30 - 15:30 | Moderators: Melissa Hooijmans, Ravinder Regatte |
Skill Level: Intermediate to Advanced
Session Number: TU-05
Overview
Muscles are the actuators of the musculoskeletal system and their function is of utmost importance in healthy and diseased joints. In this session, state-of-the-art MRI of muscle will be discussed, including fat content and other quantitative assessments.
Target Audience
Researchers and clinicians with an interest in MR imaging of muscle.
Educational Objectives
As a result of attending this course, participants should be able to:
- List the advanced MRI techniques used study fat in muscle;
- Describe the advanced quantitative MRI techniques used study muscle; and
- Identify differences in features of healthy and diseased muscle.
Overview
Muscles are the actuators of the musculoskeletal system and their function is of utmost importance in healthy and diseased joints. In this session, state-of-the-art MRI of muscle will be discussed, including fat content and other quantitative assessments.
Target Audience
Researchers and clinicians with an interest in MR imaging of muscle.
Educational Objectives
As a result of attending this course, participants should be able to:
- List the advanced MRI techniques used study fat in muscle;
- Describe the advanced quantitative MRI techniques used study muscle; and
- Identify differences in features of healthy and diseased muscle.
| 13:30 |
|
Imaging Fat in Muscle
Dimitrios Karampinos
The present educational lecture will provide an overview of the technical aspects of measuring skeletal muscle fat fraction and will discuss recent applications of measuring muscle fat fraction in neuromuscular disorders, orthopedics, metabolic diseases and aging.
|
| 14:00 |
|
Quantitative MRI of Muscle Video Permission Withheld
Gustav Strijkers
In this educational I will introduce the use of quantitative MRI to study muscle injury and disease and discuss various applications.
|
| 14:30 |
0495. 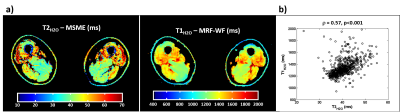 |
Quantification of water T1 and fat fraction in inclusion body myositis using MR fingerprinting with water and fat separation (MRF-WF)
Benjamin Marty, Harmen Reyngoudt, Pierre Carlier
We evaluated the accuracy of MR fingerprinting with water and fat separation (MRF-WF) in 22 patients with inclusion body myositis and investigated the potential of water T1 for monitoring disease activity in this inflammatory myopathy characterized by a combination of inflammatory and myodegenerative features. FF and B1 values derived from MRF-WF were highly correlated to reference values and we observed a significant relationship between water T1 and water T2 in the patients. MRF-WF may represent a competitor to the multi-component fitting of MSME data, or to the IDEAL-CPMG method to simultaneously extract biomarkers of disease progression and activity in neuromuscular diseases.
|
14:42 |
0496. 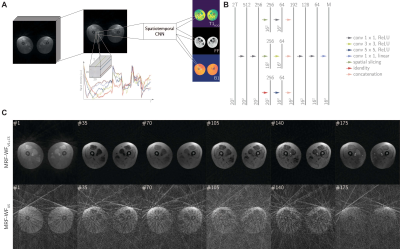 |
Accurate and Fast Reconstruction of Magnetic Resonance Fingerprinting for Water-Fat Separation in Neuromuscular Diseases
Fabian Balsiger, Olivier Scheidegger, Pierre Carlier, Mauricio Reyes, Benjamin Marty
The MR fingerprinting sequence MRF-WF is tailored for water and fat separation imaging for neuromuscular diseases (NMDs). Currently, the adoption of MRF-WF in the clinics is hindered by the long MR map reconstruction time of four hours per image slice. We propose a spatiotemporal convolutional neural network (CNN) to reconstruct the MR maps. We show that our CNN is robust to a highly heterogeneous dataset including patients with various NMDs. The method might be a possible solution for
|
14:54 |
0497. 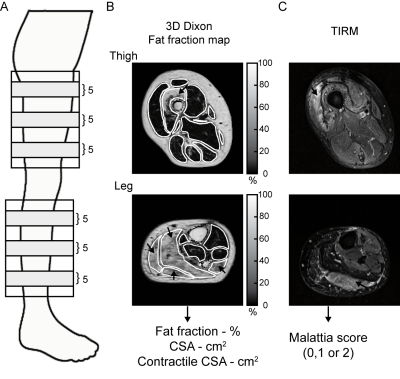 |
Behavioural intervention in myotonic dystrophy type 1 assessed by longitudinal MRI of skeletal muscles
Linda Heskamp, Kees Okkersen, Marlies van Nimwegen, Marieke Ploegmakers, Guillaume Bassez, Jean-Francois Deux, Baziel van Engelen, Arend Heerschap
A behavioural intervention, directed to increase physical activity, had a beneficial effect on lower extremity muscle function in patients with myotonic dystrophy type 1 (DM1). Here, we evaluated potential causes of the effect of this intervention with quantitative MRI in the 20 lower extremity muscles of 27 DM1 patients. We showed that it leads to a ~4% average increase in muscle mass, especially in healthy appearing muscle. Fat infiltration was not decelerated. Therefore, we conclude that some muscles in DM1 patients are trainable, preferably early on in the course of the disease.
|
15:06 |
0498. 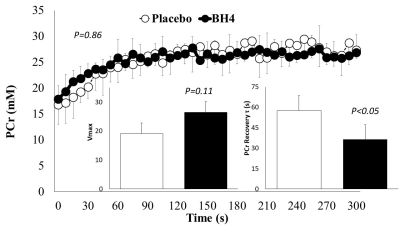 |
Effects of Tetrahydrobiopterin on Limb Blood Flow and Muscle Metabolism in Patients with COPD
Stephen Decker, Oh-Sung Kwon, Taylor Thurston, Yann Le Fur, Eun-Kee Jeong, Gwenael Layec
Exercise intolerance is an important predictor of mortality in patients with COPD, and evidence shows reduced nitric oxide (NO) bioavailability is a contributing factor. Thus, restoration of NO using BH4, a cofactor involved in NO production, is a novel therapy for improving oxygenation and metabolism in these patients. Patients with COPD performed dynamic plantar flexion exercise with 31P-MRS and vascular Doppler ultrasound assessments following supplementation of BH4. Limb blood flow during exercise was unchanged, however, exercise-induced changes in metabolic measurements were improved with BH4 supplementation. Therefore, BH4 supplementation in patients with COPD appears a promising therapy to improve muscle metabolism.
|
15:18 |
0499. 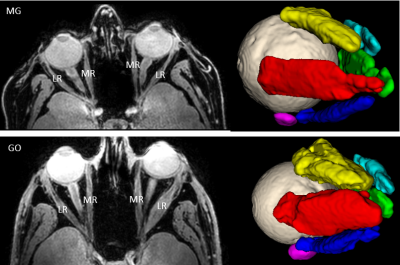 |
Increased fatty infiltration of individual extraocular muscles in myasthenia gravis and graves’ orbitopathy
Kevin Keene, Luc Van Vught, Isabeau Ciggaar, Irene Notting, Stijn Genders, Jan Verschuuren, Martijn Tannemaat, Hermien Kan, Jan-Willem Beenakker
We explored the feasibility of 7 Tesla quantitative MRI for quantifying fat fraction and muscle volume of individual extraocular muscles in myasthenia gravis (MG) and Graves’ orbitopathy (GO) patients and healthy controls. The Dixon scans show a high reproducibility for individual extraocular muscles. The fat fractions are higher in MG and GO patients than in healthy controls. Quantitative MRI of individual extraocular muscles may provide a first step to understand the pathophysiology and pattern of muscle involvement of the eyes in MG and GO patients.
|
| 15:30 |
|
Adjournment |
 Back to Program-at-a-Glance |
Back to Program-at-a-Glance |  Back to Top
Back to Top