Scientific Session
Prostate MRI
| Wednesday Parallel 3 Live Q&A | Wednesday, 12 August 2020, 13:45 - 14:30 UTC | Moderators: Nandita de Souza & Andreas Loening |
 |
0703.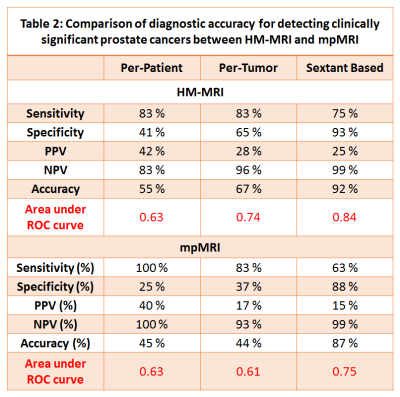 |
Prospective Validation of an Automated Hybrid Multidimensional MRI Based Tool to Identify Areas for Prostate Cancer Biopsy: Preliminary results
Aritrick Chatterjee1, Carla Harmath1, Roger Engelmann1, Ajit Devaraj2, Ambereen Yousuf1, Scott Eggener3, Glenn Gerber3, Gregory Karczmar1, and Aytekin Oto1
1Department of Radiology, University of Chicago, Chicago, IL, United States, 2Philips Research North America, Chicago, IL, United States, 3Department of Urology, University of Chicago, Chicago, IL, United States
This prospective clinical trial evaluates whether HM-MRI identifies PCa more reliably than random biopsy and/or targets detected based on PI-RADSv2. Patients underwent 3T mpMRI along with HM-MRI. Patients received 12-core TRUS-guided sextant random biopsy. Additional biopsy targets selected by radiologist (≥PI-RADS 3) and suspected PCa based on HM-MRI tissue composition estimates were biopsied, using a Uronav MR-US fusion biopsy device. The diagnostic accuracy of HM-MRI for detecting clinically significant cancers was higher than that of mpMRI on per-tumor (0.74 vs 0.61) and sextant analysis (0.84 vs 0.75). HM-MRI had higher accuracy, sensitivity, specificity and PPV than mpMRI, with similar NPV.
|
 |
0704.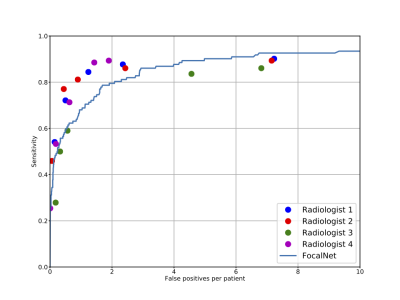 |
A Comparison between Radiologists versus Deep Learning for Prostate Cancer Detection in Multi-parameter MRI
Ruiming Cao1, Xinran Zhong2, Sohrab Afshari Mirak3, Ely Felker3, Voraparee Suvannarerg3,4, Teeravut Tubtawee3,5, Fabien Scalzo6, Steve Raman3, and Kyunghyun Sung3
1Bioengineering, UC Berkeley, Berkeley, CA, United States, 2UT Southwestern, Dallas, TX, United States, 3Radiology, UCLA, Los Angeles, CA, United States, 4Radiology, Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok, Thailand, 5Radiology, Faculty of Medicine, Prince of Songkla University, Songkhla, Thailand, 6Computer Science, UCLA, Los Angeles, CA, United States
We evaluated our recently developed deep learning system, FocalNet, for prostate cancer detection in multi-parametric MRI (mpMRI). This study performed a head-to-head comparison between FocalNet and four genitourinary radiologists in an independent evaluation cohort consisting of 126 mpMRI scans untouched during the development. FocalNet demonstrated similar detection performance to radiologists under the high specificity condition or the high sensitivity condition, while radiologists outperformed FocalNet in moderate specificity and sensitivity.
|
0705.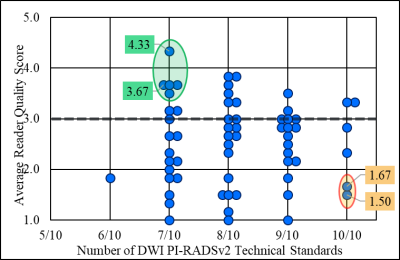 |
Does Compliance with PIRADSv2 Technical Requirements Guarantee Image Quality or Adequacy in Prostate mpMRI Reads?
Jonathan J. Sackett1, Joanna Shih1, Sarah Reese1, Jeffrey R. Brender1,2, Stephanie Harmon1, Tristan Barrett1, Mehmet Coskun1, Manuel Madariaga 1, Jamie Marko 1, Yan Mee Law 1, Evrim Turkbey 1, Sherif Mehralivand 1, Thomas Sanford 1,
Nathan Lay 1, Peter A. Pinto 1, Bradford J. Wood2, Peter L. Choyke2, Murali C. Krishna2, and Baris I Turkbey2
1Molecular Imaging Program, National Cancer Institute, National Institutes of Health, Bethesda, MD, MD, United States, 2National Cancer Institute, National Institutes of Health, Bethesda, MD, MD, United States
High quality MRIs are needed for prostate cancer screening and accurate targeting in MRI guided biopsies. Based on blind image quality assessment by image readers, compliance with the PIRADSv2 Minimum Technical Standards was determined to be neither necessary nor sufficient in ensuring quality in prostate T2 and DWI images.
|
|
0706.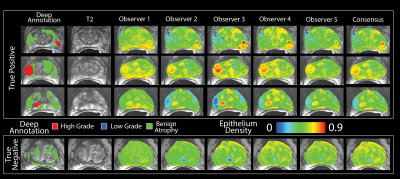 |
Radio-pathomic mapping models trained with annotations from multiple pathologists reliably distinguish high-grade prostate cancer
Sean D McGarry1, John D Bukowy2, Kenneth Iczkowsk3, Allison K Lowman2, Michael Brehler2, Samuel Bobholz1, Alex Barrington2, Kenneth Jacobsohn4, Jackson Unteriner2, Petar Duvnjak2, Michael Griffin2, Mark Hohenwalter2, Tucker Keuter5,
Wei Huang6, Tatjana Antic7, Gladell Paner7, Watchareepohn Palanghmonthip3,8, Anjishnu Banerjee5, and Peter S LaViolette2
1Biophysics, Medical College of Wisconsin, Milwaukee, WI, United States, 2Radiology, Medical College of Wisconsin, Milwaukee, WI, United States, 3Pathology, Medical College of Wisconsin, Milwaukee, WI, United States, 4Urological Surgery, Medical College of Wisconsin, Milwaukee, WI, United States, 5Biostatistics, Medical College of Wisconsin, Milwaukee, WI, United States, 6Pathology, University of Wisconsin Madison, Madison, WI, United States, 7Pathology, University of Chicago, Chicago, IL, United States, 8Pathology, Chiang Mai University, Chiang Mai, Thailand
This study demonstrates that radio-pathomic maps of epithelium density derived from annotations performed by different pathologists distinguish high-grade prostate cancer from G3 and benign atrophy. In a test set of 5 patients epithelium density maps consistently demonstrate an AUC greater than 0.9 independent of which pathologist’s annotations trained the model or which pathologist’s annotations the model is applied to. The results in a larger test set largely mirror the results in the small test set. We also showed that radio-pathomic maps of epithelium density out-performed ADC maps independent of which observer was used to train the model.
|
|
 |
0707.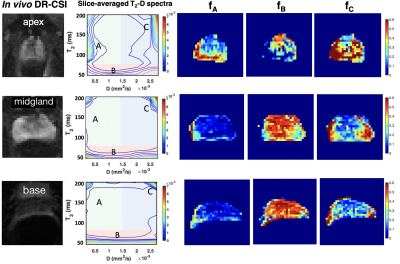 |
Towards In Vivo Prostate Microstructure Mapping Using Diffusion-Relaxation Correlation Spectrum Imaging
Zhaohuan Zhang1,2 and Holden Wu1,2
1Department of Radiological Sciences, University of California, Los Angeles, Los Angeles, CA, United States, 2Department of Bioengineering, University of California, Los Angeles, Los Angeles, CA, United States
Recent work has demonstrated the ability of Diffusion-Relaxation Correlation Spectrum Imaging (DR-CSI) to quantify prostate microscopic tissue compartments (epithelium, stroma and lumen) in ex vivo prostate specimens at 3T using whole-mount digital histopathology as the reference. This study further developed DR-CSI for in vivo characterization of prostate microstructure using high resolution ex vivo DR-CSI as the reference. Consistent trends in DR-CSI signal component fraction variations in different prostate regions were found using in vivo DR-CSI across subjects, and agreed with trends on ex vivo DR-CSI.
|
 |
0708.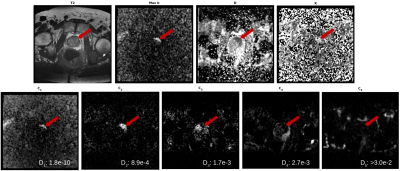 |
Improved characterization of prostate tumors through multi-compartmental analysis of restriction spectrum imaging data
Christopher C Conlin1, Christine H Feng2, Ana E Rodriguez-Soto1, Roshan A Karunamuni2, Joshua M Kuperman1, Dominic Holland1, Rebecca Rakow-Penner1, Tyler M Seibert2, Anders M Dale1,3, and Michael E Hahn1
1Department of Radiology, UC San Diego School of Medicine, La Jolla, CA, United States, 2Department of Radiation Medicine and Applied Science, UC San Diego School of Medicine, La Jolla, CA, United States, 3Department of Neurosciences, UC San Diego School of Medicine, La Jolla, CA, United States Restriction spectrum imaging (RSI) is an advanced multi-shell diffusion technique that models the diffusion-weighted signal as a linear combination of exponential decays. While RSI shows promise for assessing prostate cancer, an optimal RSI model that effectively characterizes the diffusion properties of both normal and cancerous prostate tissue is essential to ensuring an accurate evaluation of prostate cancer lesions. In this study, we determined optimal ADC values for several RSI models of the prostate and assessed the number of tissue compartments required to best describe diffusion in both normal and cancerous prostate tissue. |
0709.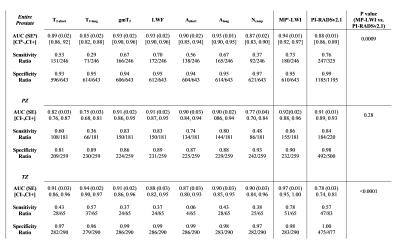 |
Comparing the Diagnostic Accuracy of Luminal Water Imaging versus PI-RADSv2.1 in Detection of Prostate Cancer
Shirin Sabouri1, Silvia Chang2,3,4, Emily Pang2, Rehab Mohammedeid2, Edward Jones5, Larry Goldenberg3,4, Peter Black3,4, and Piotr Kozlowski1,2,3,4
1UBC MRI Research Centre, Vancouver, BC, Canada, 2Department of Radiology, The University of British Columbia, Vancouver, BC, Canada, 3Department of Urologic Sciences, The University of British Columbia, Vancouver, BC, Canada, 4Vancouver Prostate Centre, Vancouver, BC, Canada, 5Department of Pathology and Laboratory Medicine, The University of British Columbia, Vancouver, BC, Canada
Luminal water imaging (LWI) is an MRI technique that detects regions of decreased lumen volume in prostate. Recent studies on LWI have shown promising results regarding the accuracy of this technique in diagnosis of prostate cancer. However, to the best of our knowledge no study has yet compared the performance of LWI against the current clinical assessment. In this study, we perform a comparison between the diagnostic accuracy of LWI with the PI-RADSv2.1 assessment. Our results show that LWI performs similar to the PI-RADSv2.1 in the entire prostate and peripheral zone, and outperforms significantly in transition zone.
|
|
0710. |
Relaxed-VERDICT: decoupling relaxation and diffusion for comprehensive microstructure characterization of prostate cancer.
Marco Palombo1, Saurabh Singh2, Hayley Whitaker2, Shonit Puwani2, Daniel C. Alexander1, and Eleftheria Panagiotaki1
1Centre for Medical Image Computing, Department of Computer Science, University College London, London, United Kingdom, 2Centre for Medical Imaging, University College London, London, United Kingdom
This work presents a comprehensive VERDICT prostate model (relaxed-VERDICT) that includes compartment-specific relaxation effects providing prostate microstructural estimates unbiased by the relaxation properties of the tissue. We compare relaxed-VERDICT with the original VERDICT model and use it to provide estimates of T2 and T1 in benign and tumor prostate tissue. Our results suggest that original VERDICT’s fic contrast is mostly driven by diffusion, supporting its use as imaging marker of apparent cellular volume fraction. Relaxed-VERDICT estimates of T1/T2 values are in very good agreement with literature. Finally, we propose a machine learning based processing pipeline that provides ultra-fast quantitative maps.
|
|
0711.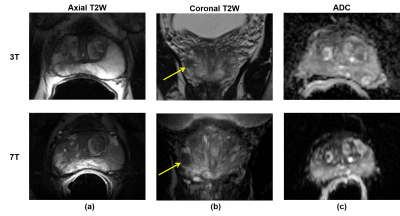 |
Prostate cancer multiparametric MRI comparison study of 3T versus 7T: lesion detection and study design considerations
Ethan Leng1, Benjamin Spilseth2, Anil Chauhan2, Joseph Gill2, Ana Rosa2, Arcan Erturk1, Naoharu Kobayashi1, Xiaoxuan He1, Christopher Warlick3, and Gregory Metzger1
1Center for Magnetic Resonance Research, University of Minnesota, Minneapolis, MN, United States, 2Radiology, University of Minnesota, Minneapolis, MN, United States, 3Urology, University of Minnesota, Minneapolis, MN, United States
Recent works have demonstrated the feasibility of prostate multiparametric MRI (mpMRI) at 7T with improved resolution compared to mpMRI at 3T. However, the clinical relevance of finer anatomic details versus the drawbacks of increased imaging artifacts at 7T has yet to be investigated. In this work, we conducted a retrospective, multi-reader clinical evaluation of 19 paired mpMRI studies at 3T and 7T. The primary outcome of interest was accuracy of prostate cancer detection, with image quality and artifacts as secondary outcomes.
|

 Back to Program-at-a-Glance
Back to Program-at-a-Glance Watch the Video
Watch the Video Back to Top
Back to Top