Scientific Session
Women's Imaging
Session Topic: Women's Imaging
Session Sub-Topic: Placenta
Oral
Body
| Tuesday Parallel 3 Live Q&A | Tuesday, 11 August 2020, 14:30 - 15:15 UTC | Moderators: Simon Shah & KyungHyun Sung |
Session Number: O-29
0576.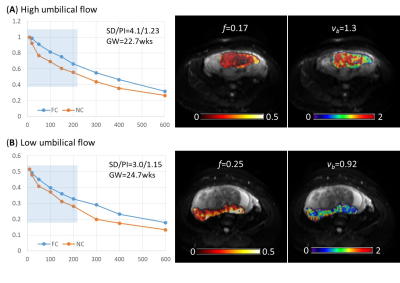 |
Probing ballistic flow in the placenta using flow-compensated and non-compensated diffusion MRI
Ling Jiang1,2, Taotao Sun1,2, Yuhao Liao3, Yi Sun4, Yi Zhang3, Zhaoxia Qian1,2, and Dan Wu3
1Maternity and Child Health Hospital, School of Medicine, Shanghai Jiao Tong University, Shanghai, China, 2Shanghai Key Laboratory of Embryo Original Diseases, Shanghai, China, 3Key Laboratory for Biomedical Engineering of Ministry of Education, Department of Biomedical Engineering, College of Biomedical Engineering & Instrument Science, Zhejiang University, Hangzhou, China, 4MR Collaboration, Siemens Healthcare Ltd., Shanghai, China
Intravoxel incoherent motion (IVIM) imaging is frequently used to evaluate microcirculatory flow. With the conventional diffusion MRI, IVIM effects include both pseudo-diffusive microcirculatory flow and bulk (or ballistic) blood flow. We propose a joint use of flow-compensated (FC) and non-FC diffusion gradient waveforms to specifically probe the fraction and velocity of ballistic flow in the placenta. The measured ballistic flow velocity showed a high correlation with umbilical flow based on Doppler ultrasound and a negative correlation with gestational age. These results demonstrated the potential of using FC/NC dMRI to noninvasively measure flow velocity inside the placenta.
|
|
0577.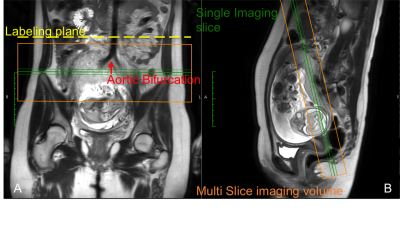 |
Quantitative Perfusion Measurements of the Human Placenta with FAIR and pCASL Arterial Spin Labeling at 3T: Initial Feasibility
Quyen N. Do1, Christina Herrera2, Matthew A. Lewis1, Yin Xi1,3, Catherine Y. Spong2, Diane M. Twickler1,2, and Ananth J. Madhuranthakam1,4
1Radiology, UT Southwestern Medical Center, Dallas, TX, United States, 2Obstetrics and Gynecology, UT Southwestern Medical Center, Dallas, TX, United States, 3Population and Data Sciences, UT Southwestern Medical Center, Dallas, TX, United States, 4Advanced Imaging Research Center, UT Southwestern Medical Center, Dallas, TX, United States
Quantitative measurement of placental perfusion is important for the assessment of placental function. We have developed and optimized a non-contrast perfusion MR imaging technique utilizing pseudo-continuous arterial spin labeling (pCASL) to quantitatively measure human placental perfusion at 3T. Placental perfusion was also assessed using flow-sensitive alternating inversion recovery (FAIR). The average placental blood flow (108±47 mL/100g/min) was comparable to published literature values.
|
|
0578.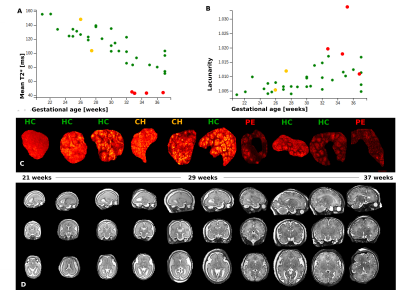 |
CARdiac and Placental imaging (CARP) in pregnancy to assess etiology of preeclampsia and predict cardiovascular disease risk in later life
Jana Hutter1, Kathleen Colford1, Anthony Price1, Johannes Steinweg1, Lisa Story1, Kuberan Pushparajah1, Laura McCabe1, Alison Ho2, Adam J Lewandowski3, Joseph Hajnal1, Lucy Chappell2, Pablo Lamata1, and Mary Rutherford1
1Biomedical Engineering Department, School of Biomedical Engineering and Imaging Sciences, King's College London, London, United Kingdom, 2Academic Women's Health, King's College London, London, United Kingdom, 3Division of Cardiovascular Medicine, University of Oxford, Oxford, United Kingdom
Pre-eclampsia (PE) is one of the most common, yet serious, complications of pregnancy. Its manifestations during pregnancy -high blood pressure, proteinuria and placental lesions- are associated with both maternal and fetal morbidity and mortality. Maternal symptoms resolve after delivery but a lifelong elevated risk for cardiovascular disease (CVD) remains. The CARP study combines functional placental and fetal MRI with (maternal) cardiovascular MR during pregnancy at the time of maximal stress to the maternal heart, in an attempt to disentangle the complex cardiac and placental interactions in disease etiology and to predict maternal cardiovascular risk in later life.
|
|
 |
0579.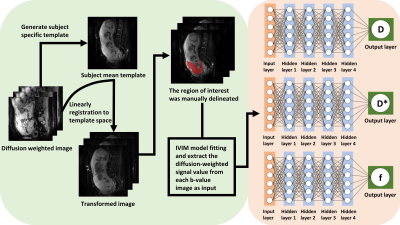 |
Learning-based approach for accelerated IVIM imaging in the placenta
Fan Huang1, Shi-Ming Wang2, Guohui Yan3, Zhihao Wen4, Yuhao Liao1, Yi Zhang1, Yu Zou3, and Dan Wu1
1Key Laboratory for Biomedical Engineering of Ministry of Education, Department of Biomedical Engineering, College of Biomedical Engineering & Instrument Science, Zhejiang University, Hangzhou, China, 2Department of Medical Imaging and Radiological Sciences, Chang Gung University, Taoyuan, Taiwan, 3Department of Radiology,Women's Hospital,School of Medicine, Zhejiang University, Hangzhou, China, 4Purple-river software corporation, Shenzhen, China
Q-space learning has shown its potential in accelerating Q-space sampling in diffusion MRI. This study proposed a new deep learning framework to accelerate intravoxel incoherent motion (IVIM) imaging and to estimate IVIM parameters from a small number of b values in the human placenta. The results demonstrated the feasibility of a reduced IVIM protocol using the proposed framework, which may help to accelerate the acquisition and reduce motion for placental IVIM.
|
 |
0580.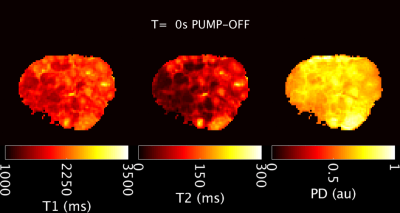 |
Placental MRI: Using a novel ex vivo placental perfusion chamber to validate in vivo magnetic resonance fingerprinting (MRF) relaxometry
Jeffrey N Stout1, Shahin Rouhani1,2, Congyu Liao3, Esra Abaci Turk1, Christopher G Ha1, Karen Rich4, Lawrence L. Wald3, William H. Barth, Jr5, Drucilla J. Roberts2, Elfar Adalsteinsson6, and P. Ellen Grant1
1Fetal-Neonatal Neuroimaging & Developmental Sciences Center, Boston Children's Hospital, Boston, MA, United States, 2Department of Pathology, Massachusetts General Hospital, Boston, MA, United States, 3A. A. Martinos Center for Biomedical Imaging, Massachusetts General Hospital, Boston, MA, United States, 4Department of Radiology, Massachusetts General Hospital, Boston, MA, United States, 5Maternal-Fetal Medicine, Obstetrics and Gynecology, Massachusetts General Hospital, Boston, MA, United States, 6Institute for Medical Engineering and Science; Department of Electrical Engineering and Computer Science, Massachusetts Institute of Technology, Cambridge, MA, United States
The placenta is a challenging MRI target. Acquisition schemes developed for other organs, with implicit assumptions about motion, tissue composition and perfusion, should be vetted for applicability to the placenta. We have developed an ex vivo placental perfusion chamber with integrated MRI receive coil for high SNR and imaging acceleration to validate in vivo acquisitions in a controlled environment. Here we examine the effect of flowing spins on MRF relaxometry. We offer evidence that T1 is sensitive to overall fluid volume, while T2 is additionally sensitive spin inflow. Our placental perfusion system appears promising for validating in vivo quantitative MRI.
|
0581.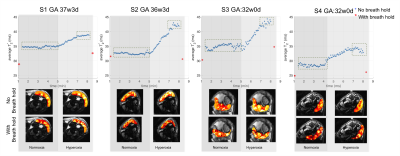 |
Placental MRI: Effect of maternal position, breath hold and oxygen state on placental T2* measurements
Esra Abaci Turk1, Jeffrey N. Stout1, Borjan Gagoski1, Mary Katherine Manhard2, Elfar Adalsteinsson3,4,5, Kawin Setsompop2, Polina Golland3,6, Drucilla J. Roberts7, William H. Barth Jr8, and P. Ellen Grant1
1Fetal-Neonatal Neuroimaging & Developmental Science Center, Boston Children's Hospital, Boston, MA, United States, 2Athinoula A. Martinos Center for Biomedical Imaging, Massachusetts General Hospital, Charlestown, MA, United States, 3Department of Electrical Engineering and Computer Science, Massachusetts Institute of Technology, Cambridge, MA, United States, 4Harvard-MIT Health Sciences and Technology, Massachusetts Institute of Technology, Cambridge, MA, United States, 5Institute for Medical Engineering and Science, Massachusetts Institute of Technology, Cambridge, MA, United States, 6Computer Science and Artificial Intelligence Laboratory (CSAIL), Massachusetts Institute of Technology, Cambridge, MA, United States, 7Pathology, Massachusetts General Hospital, Boston, MA, United States, 8Maternal-Fetal Medicine, Massachusetts General Hospital, Boston, MA, United States
T2* relaxometry has been proposed as a semi-quantitative measure for placental oxygen transport. However, to use T2* as a diagnostic tool, it is necessary to define the normal range of results and factors that influence those results. In this study we investigated the effect of maternal position, breath-holds and oxygen state on placental T2*. We observed lower T2* with breath-hold protocol compared to no breath-hold protocol in left lateral position. Additionally, lower T2* was measured in supine position during normoxic episode compared to left lateral position with no breath-hold protocol.
Further studies are needed to understand these factors better.
|
|
0582.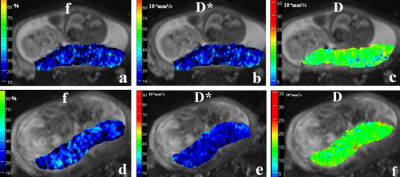 |
Placental perfusion in Fetuses with congenital heart disease and normal pregnancy assessed with intravoxel incoherent motion imaging
Cong Sun1, Xin Chen1, Jinxia Zhu2, Robert Grimm3, and Guangbin Wang1
1Shandong Medical Imaging Research Institute, Shandong University, Jinan, China, 2MR Collaboration, Healthcare Siemens Ltd., Beijing, China, Beijing, China, 3Healthcare GmbH, Erlangen, Germany, Erlangen, Germany
To determine whether placental perfusion alterations are evident in utero in fetuses with congenital heart disease (CHD), we quantitatively investigated perfusion in 28 fetuses with CHD and 39 healthy gestational age–matched controls using intravoxel incoherent motion imaging (IVIM). We found that the f values were significantly higher in the CHD group compared with the normal pregnancy group (37.8% vs. 30.2%, p<0.0001), and there was no significant difference in the D value and D* value between the two groups. The increased placental perfusion in fetuses with CHD might represent an attempt to compensate for a perfusion deficit in fetal circulation.
|
|
0583.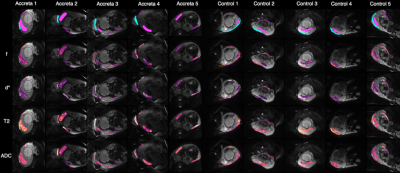 |
Placenta Accreta Spectrum (PAS) Disorders Investigated with Multi-Compartment Placental MRI
Nada Mufti1,2, Patrick O'Brien3, George Attilakos3, Magdalena Sokolska4, Priya Narayanan3, Rosalind Aughwane1, Neil Sebire5, Imen Ben-Salha3, Nafisa Wilkinson3, Giles Kendall1,3, Jan Deprest1,3,6, David Atkinson7, Tom Vercauteren2,6,
Sebastien Ourselin2, Anna L David1,3,6, and Andrew Melbourne2,8
1Institute for Women's Health, University College London (UCL), London, United Kingdom, 2School of Biomedical Engineering and Imaging Sciences (BMEIS), Kings College London, London, United Kingdom, 3University College London Hospital, London, United Kingdom, 4Department of Medical Physics and Biomedical Engineering, University College London Hospital (UCLH), London, United Kingdom, 5Great Ormond Street Hospital for Children, London, United Kingdom, 6University Hospitals, KU Leuven, Leuven, Belgium, 7Centre for Medical Imaging (CMI), University College London (UCL), London, United Kingdom, 8Department of Medical Physics and Biomedical Engineering, University College London (UCL), London, United Kingdom
Uterine scarring from caesarean section (CS) can lead to subsequent abnormally adherent or invasive placenta. Failure to recognise Placenta Accreta Spectrum disorders prior to delivery can potentially cause catastrophic bleeding and death. Complex surgical interventions may be required to remove placental invasion of the uterine myometrium and nearby organs. Antenatal detection and correct PAS grading are important to plan delivery. Current ultrasound and MRI imaging are limited to subjective assessment of vascular invasion. We propose a multi-compartment model1 that can quantify vascularity and proportion of abnormal placentation across the previous CS scar for objective diagnosis and to assist surgical planning.
|
|
0584.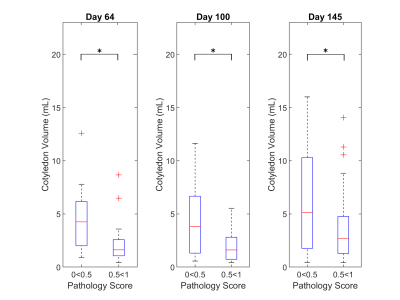 |
Quantitative Ferumoxytol Dynamic Contrast Enhanced (DCE) MRI Evaluation of the Placenta after Zika Virus Infection in the Rhesus Macaque
Daniel Seiter1, Kai D. Ludwig1, Sydney Nguyen2,3,4, Megan E Murphy2,3,4, Kathleen M Antony2,3,4, Ruiming Chen1, Terry K Morgan5, Ante Zhu6,7, Archana Dhyani8, Sean B Fain1,6,7, Kevin M Johnson1,7, Thaddeus G. Golos2,3,4, and Oliver Wieben1,7
1Medical Physics, University of Wisconsin-Madison, Madison, WI, United States, 2Comparative Biosciences, University of Wisconsin-Madison, Madison, WI, United States, 3Wisconsin National Primate Research Center, University of Wisconsin-Madison, Madison, WI, United States, 4Obstetrics & Gynecology, University of Wisconsin-Madison, Madison, WI, United States, 5Pathology, Oregon Health & Science University, Portland, OR, United States, 6Biomedical Engineering, University of Wisconsin-Madison, Madison, WI, United States, 7Radiology, University of Wisconsin-Madison, Madison, WI, United States, 8Computer Science, University of Wisconsin-Madison, Madison, WI, United States
Proper placental development is crucial to fetal health. Here we report preliminary results characterizing the effects of Zika virus on the placenta of the rhesus macaque using dynamic contrast enhanced (DCE) MRI scans. DCE data were processed to identify individual cotyledons, their volume, and blood flow at three time points during gestation and were compared with pathological findings from term placenta dissection. Analysis shows a statistically significant decrease in cotyledon volume with pathology, measurable as early as 64 days gestation.
|
|
 |
0585.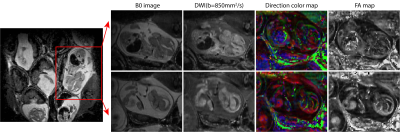 |
High resolution diffusion and perfusion MRI of normal, preeclamptic and growth-restricted mice models reveal clear fetoplacental differences
Qingjia Bao1, Eddy Solomon1, Ron Hadas1, Stefan Markovic1, Odelia Chitrit1, Maxime Yon1, Michal Neeman1, and Lucio Frydman1
1Weizmann Institute of Science, Rehovot, Israel
DWI can evaluate pregnancy-related dysfunctions, yet EPI’s sensitivity to motions and air/water/fat heterogeneities complicate these studies in preclinical settings. We have developed DWI methodologies based on SPatiotemporal ENcoding (SPEN) for overcoming these obstacles, delivering single-shot images at ≈100µm in-plane resolutions. These methods were used to monitor fetoplacental differences between naïve and knockout mice strains mimicking preeclampsia and IUGR. High definition ADC/DTI maps could resolve the placental layers (maternal, fetal, trophoblastic), umbilical cords, and various brain compartments in the developing fetuses. Daily monitoring also showed differences in the development of placental and fetal (e.g. brain) structures among normal and disease models.
|

 Back to Program-at-a-Glance
Back to Program-at-a-Glance Watch the Video
Watch the Video Back to Top
Back to Top