Carles Javierre Petit1, Ashish A. Tamhane2, Arnold M. Evia1, Nazanin Makkinejad1, Gady Agam3, David A. Bennett2, Julie A. Schneider2, and Konstantinos Arfanakis1,2
1Biomedical Engineering, Illinois Institute of Technology, Chicago, IL, United States, 2Rush Alzheimer’s Disease Center, Rush University Medical Center, Chicago, IL, United States, 3Computer Science, Illinois Institute of Technology, Chicago, IL, United States
1Biomedical Engineering, Illinois Institute of Technology, Chicago, IL, United States, 2Rush Alzheimer’s Disease Center, Rush University Medical Center, Chicago, IL, United States, 3Computer Science, Illinois Institute of Technology, Chicago, IL, United States
This work shows EPVS
associations with gross infarcts and cerebral amyloid
angiopathy, and independent contributions on cognition above and beyond neuropathologies and demographics in a large community cohort of older adults after quantitative
assessment of EPVS using deep learning.
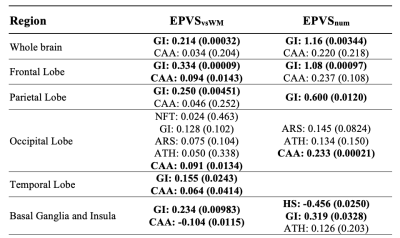
Figure 5: Neuropathologic correlates of EPVS. Pathologies
with significant associations with EPVS in the single pathology models were
included in the same multiple linear regression model and are listed in each
element of this table. Abbreviations: AB=amyloid beta plaques, NFT=neurofibrillary
tangles, HS=hippocampal sclerosis, GI=gross infarcts, MI=microscopic infarcts,
ARS=arteriolosclerosis, ATH=atherosclerosis, CAA=cerebral
amyloid angiopathy, LB=Lewy bodies, TDP=TDP-43 pathology. Significant
pathologies are in bold. [PATH: COEFFICIENT (P-VALUE)].

