Digital Posters
MR-Guided Interventions: Devices & Applications
ISMRM & SMRT Annual Meeting • 15-20 May 2021

| Concurrent 3 | 17:00 - 18:00 |
4005.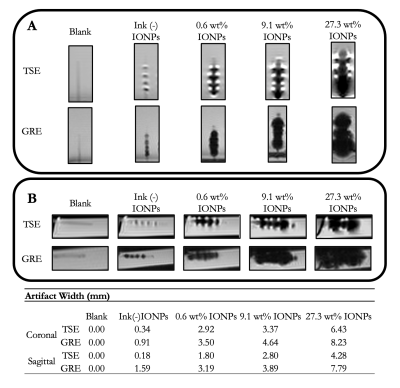 |
Development and Evaluation of an MR-safe Interventional Catheter with Tunable MR Visibility and Radiopacity
Bridget F Kilbride1, Caroline D Jordan2, Andrew Chu3, Dave Barry3, Kerstin Mueller4, Sinyeob Ahn4, Teri Moore5, Mark W Wilson5, and Steven W Hetts5
1Radiology and Biomedical Imaging, University of California San Francisco, San Francisco, CA, United States, 2Texas A&M University, Houston, TX, United States, 3Penumbra, Inc., Alameda, CA, United States, 4Siemens Medical Solutions, Malvern, PA, United States, 5University of California San Francisco, San Francisco, CA, United States
Interventional MRI catheter-based procedures are greatly limited by current devices and their safety profiles, and next-generation MR-safe devices are still in development. We designed and evaluated a polymeric catheter concept that is both safe and visible in MRI and X-ray environments. All imaging was done in a two-room hybrid angio-MR suite to demonstrate compatibility with next-generation image-guided procedures. In a phantom, we acquired GRE and TSE sequences at 3T and imaged on a clinical biplane angiographic system to quantitate MRI visibility and radiopacity, respectively. The catheters exhibited promising tracking characteristics under MRI and X-ray on a polymer-based catheter.
|
|||
4006.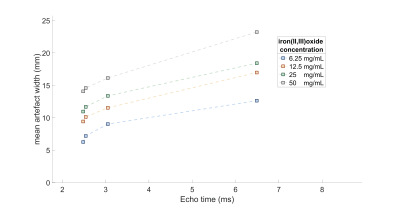 |
Optimized passive marker device visibility for MRI-guided endovascular interventions at 3T: a pulsatile flow phantom study
Han Nijsink1, Kristian G. Overduin1, Sytse F. De Jong1, Paul J.A. Borm2, Torben Pätz3, Dennis G.H. Bosboom4, Michiel C. Warlé1, and Jurgen J. Fütterer1
1Radboudumc, Nijmegen, Netherlands, 2Nano4Imaging, Düsseldorf, Germany, 3Fraunhover MEVIS, Bremen, Germany, 4Soteria Medical B.V., Arnhem, Netherlands
MRI-guidance for endovascular interventions is only eligible with clearly visible endovascular devices. Hence, we quantitatively and qualitatively evaluated marker visibility and artifact size of passive marker guidewires for different MRI sequence types, MRI parameters and marker concentrations at 3T MRI using a pulsatile flow phantom. Artifact size was positively correlated with TE and marker concentration and was significantly larger for bSSFP images compared to GRE images. The GRE images outperformed the bSSFP images in the quantitative image quality assessment. In conclusion, markers were adequately visible in GRE images and artifact visibility can be optimized by adjusting TE and marker concentration.
|
|||
4007.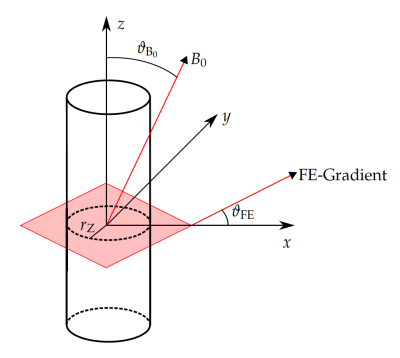 |
MRI Needle Tracking with Phase-only Cross-Correlation (POCC) in the Presence of Susceptibility Artifacts
Andreas Reichert1 and Michael Bock1
1Department of Radiology, Medical Physics, Medical Center – University of Freiburg, Faculty of Medicine, University of Freiburg, Freiburg, Germany
The phase-only cross correlation (POCC) algorithm can be used to accurately detect the orientation of a passive needle guide in needle interventions. A POCC sequence continuously visualizes the planned needle pathway during needle guide movement. The insertion of a needle into the needle guide, however, degrades the POCC detection because of susceptibility artifacts. In this work, susceptibility artifacts of a needle are measured and simulated, and a potential integration integrated into the POCC algorithm is evaluated.
|
|||
4008.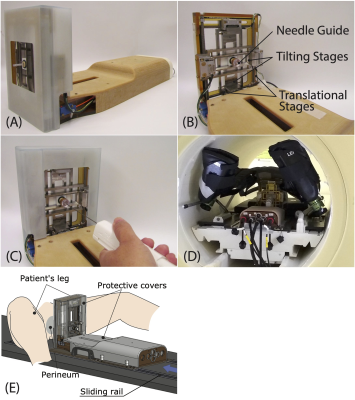 |
4-DoF Needle-Guide Manipulator System for Interactive Real-Time MRI-Guided Prostate Interventions
Junichi Tokuda1,2, Pedro Moreira1,2, Amanda Aleong3, Franklin King1, John P Grimble4, Kemal Tuncali1,2, Ravi Seethamraju5, Gerald Moran6, Himanshu Bhat5, Nick V Iftimia4, and Jesung Park4
1Radiology, Brigham and Women's Hospital, Boston, MA, United States, 2Harvard Medical School, Boston, MA, United States, 3University of Toronto, Toronto, ON, Canada, 4Physical Science Inc., Andover, MA, United States, 5Siemens Medical Solutions USA Inc., Boston, MA, United States, 6Siemens Healthcare Ltd., Oakville, ON, Canada
Accurate needle placement is crucial for MRI-guided targeted prostate biopsy. However, needle placement accuracy is often affected by the deviation of the needle caused by the anatomical structures on the needle path. To avoid anatomical structures that are likely to cause significant needle deviation, we developed a 4-degree-of-freedom (DoF) needle-guide manipulator system named “Smart Template”. The Smart Template allows physicians to insert a needle accurately to the target while monitoring the needle through interactive real-time MRI. We performed a preliminary evaluation of the device to test the feasibility of needle placement using Smart Template.
|
|||
4009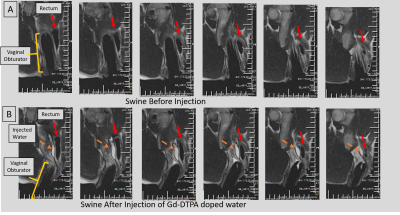 |
An MR-Tracked Metallic injection needle for Distancing Radiation-sources from Sensitive tissues: Construct and Initial testing in Swine Video Permission Withheld
Ehud Jeruham Schmidt1, Marc Morcos2, Anthony Gunderman3, Junichi Tokuda4, Ravi Teja Seethamraju5, Luca Neri1, Carmen Kut2, Henry R. Halperin1, Akila Ninette Viswanathan2, and Yue Chen3
1Medicine (Cardiology), Johns Hopkins School of Medicine, Baltimore, MD, United States, 2Radiation Oncology, Johns Hopkins School of Medicine, Baltimore, MD, United States, 3Mechanical Engineering, University of Arkansas, Fayetteville, AR, United States, 4Radiology, Brigham and Women's Hospital, Boston, MA, United States, 5Siemens Medical Solutions, Boston, MA, United States
A metallic actively-tracked injection needle was constructed for purposes of reducing dose to normal tissues surrounding irradiated tumors in cervical cancer and prostate cancer radiation therapy. Hydrogel is injected into tissue or anatomic cavities between the tumor and normal tissues, increasing the distance from the radiation source. The needle was tested in a gynecological phantom and in swine. It provided 1.2x1.2x1.2mm3 targeting precision @16 frames-per-second navigation, supporting rapid navigation speeds currently possible only under X-ray or Ultrasound guidance. The injected topology over time was visualized during injection, allowing creation of more uniform dose-shielding regions.
|
|||
4010.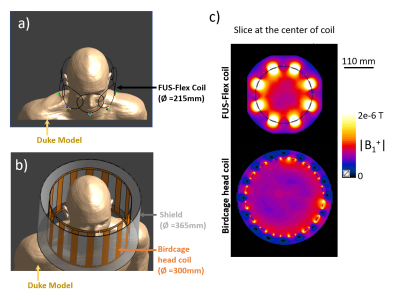 |
Attenuation of the dark band artifact in MR-guided focused ultrasound using an ultra-flexible high-sensitivity head coil
Isabelle Saniour1, Fraser Robb2, Victor Taracila2, Henning U. Voss1, Michael G. Kaplitt3, J. Levi Chazen1, and Simone Angela Winkler1
1Department of Radiology, Weill Cornell Medicine, New York, NY, United States, 2MR Engineering, GE Healthcare, Aurora, OH, United States, 3Department of Neurological Surgery, Weill Cornell Medicine, New york, NY, United States
Transcranial magnetic resonance guided focused ultrasound (MRgFUS) has shown dramatic success in the treatment of various neurodegenerative diseases. However, black band artifacts arise in MR images due to the high-permittivity water bath and the metallically lined helmet-shaped transducer together with the vendor-installed body coil. In this work, we present electromagnetic simulations of a very thin, flexible, and acoustic transparent head coil design (FUS-Flex). Simulations show a signal-to-noise-ratio (SNR) increase of 3.5× and 5× compared to a body coil with and without the transducer, respectively, and an attenuation of the black band artifact in the regions of interest.
|
|||
4011.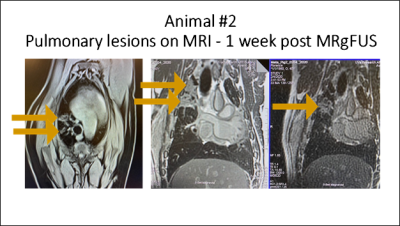 |
MR guided Focused Ultrasound as a Non-Invasive Surgical Treatment of Lung Cancer
Jaime Mata1, Lauren Powlovich2, David Moore2, and Linda Martin1
1University of Virginia, Charlottesville, VA, United States, 2Focused Ultrasound Foundation, Charlottesville, VA, United States
Malignant lung cancer carries a poor prognosis with a 5-year survival rate of about 18%. This new method proposes an innovative minimally invasive procedure for the transcutaneous ablation of lung tumor masses with complete removal or significant debulking of the masses. This new procedure could increase lung cancer survival rates and at the same time decrease morbidity and side effects associated with current treatment therapies. It will also provide a viable treatment for a large group of patients that cannot tolerate resection surgery, radiotherapy and chemotherapy, or who have had prior radiation and cannot have additional radiation to that region.
|
|||
4012.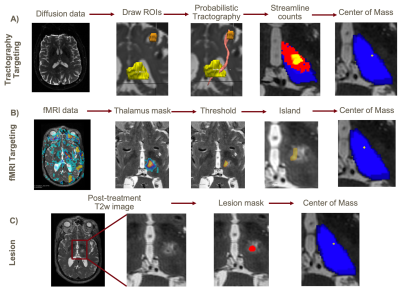 |
Comparison of Diffusion Tractography and fMRI-based Targeting for MRgFUS Treatment of Essential Tremor
Kristin Quah1, Jonathan Samuel Goodman2, Gustavo Loo Kang Chau3, Kim Butts Pauly4, Pejman Ghanouni4, Gary Glover4, and Jennifer McNab4
1Electrical Engineering, Stanford University, Stanford, CA, United States, 2Biophysics, Stanford University, Stanford, CA, United States, 3Bioengineering, Stanford University, Stanford, CA, United States, 4Radiology, Stanford University, Stanford, CA, United States
Probabilistic diffusion tractography and fMRI are two alternative methods for targeting the ventral intermediate nucleus of the thalamus in patients with essential tremor (ET) for treatment with transcranial magnetic resonance imaging-guided focused ultrasound (tcMRgFUS). In this study, three ET subjects underwent MRgFUS thalamotomy with traditional targeting using anatomic landmarks. Tractography and fMRI targeting were compared retrospectively to determine how they relate to one another and to the targets selected by the surgeon. Two of the three subjects showed a consistent spatial relationship between fMRI, tractography and anatomical targets.
|
|||
4013.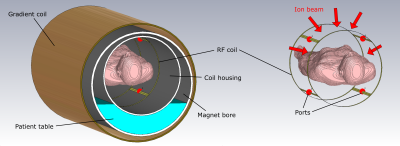 |
Comparison of birdcage resonator designs for clinical MR-guided radiotherapy
Kilian A. Dietrich1,2, Sebastian Klüter2, Benjamin R. Knowles1, Jürgen Debus2,3, Markus E. Ladd1,3, and Tanja Platt1
1Medical Physics in Radiology, German Cancer Research Center (DKFZ), Heidelberg, Germany, 2Radiation Oncology, University Hospital, Heidelberg, Germany, 3Faculty of Medicine, Heidelberg University, Heidelberg, Germany
Electromagnetic field simulations were performed at 0.345T and 1.5T to find an advantageous RF coil design for typical scanners in MR-guided therapy. Hence, different birdcage coil designs were characterized and compared with one another with respect to their corresponding transmit and receive field characteristics.
|
|||
4014.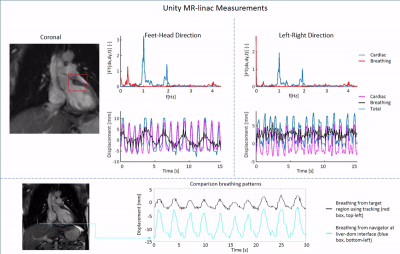 |
Feasibility of free breathing real-time cine-MRI for MR-guided Cardiac Radioablation on the Unity MR-linac
Osman Akdag1, Stefano Mandija1, Pim Borman1, Eveline Alberts2, and Martin Fast1
1Radiotherapy, University Medical Center Utrecht, Utrecht, Netherlands, 2Philips Healthcare, Best, Netherlands Stereotactic arrhythmia radioablation (STAR) is a novel non-invasive treatment technique for ventricular tachycardia patients, refractory to conventional catheter ablation. Here, we investigate the feasibility of integrating real-time, free-breathing, cardiac cine-MRI into the STAR radiotherapy workflow. As a first step towards MRI-guided STAR treatments, we test our imaging approach on a diagnostic 1.5T MRI-simulator (Philips, Ingenia), and on a 1.5T Elekta Unity MR-linac. Our results indicate the feasibility of acquiring real-time, free-breathing, cine MRI images on both systems at 14Hz, enabling real-time motion assessment and delivery adaptation without additional cardiac imaging hardware. |
|||
4015.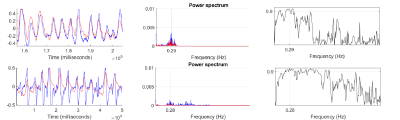 |
Clinical evaluation of 4DMRI for lung cancer radiation treatment planning
Jonathan Goodwin1,2, Satomi Higuchi1, Laura O'Connor1,2, Amy Zafara1, Kate Skehan1, Terry Perkins3, Sanjiv Gupta1, Peter Greer1,2, Jane Ludbrook1,2, and John Simpson1,2
1Calvary Mater Hospital, Newcastle, Australia, 2Univeristy of Newcastle, Newcastle, Australia, 3Blacktown Cancer & Haematology Centre, Blacktown, Australia
4D-CT is routinely acquired for lung cancer treatment planning to visualise the extent of tumour motion, to determine the appropriate treatment target volume. However, it can be unreliable in cases of irregular breathing, is susceptible to image artefact in regions close to the diaphragm, and shows generally poor soft tissue contrast. In this study we evaluated an alternative self-navigating 4D-MRI approach in terms of motion detection accuracy, measured tumour volume, and dosimetric differences observed with respect to patients’ existing lung cancer treatment plans.
|
|||
4016.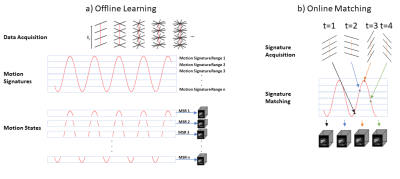 |
MR SIGnature MAtching (MRSIGMA) with retrospective self-validation for real-time volumetric tumor motion imaging
Nathanael Kim1, Kathryn Tringale2, Christopher Crane2, Neelam Tyagi1, and Ricardo Otazo1,3
1Medical Physics, Memorial Sloan Kettering Cancer Center, New York, NY, United States, 2Radiation Oncology, Memorial Sloan Kettering Cancer Center, New York, NY, United States, 3Radiology, Memorial Sloan Kettering Cancer Center, New York, NY, United States
MRSIGMA is a promising real-time volumetric imaging for MRI-guided adaptive radiotherapy using a MR-Linac system. However, the lack of a real-time 3D reference image acquired with similar temporal resolution introduces significant challenges for in vivo validation. This work proposes a retrospective self-validation for MRSIGMA, where the same data used for real-time imaging are used to create a non-real-time reference. MRSIGMA with self-validation is tested in patients with liver tumors using quantitative metrics defined on the tumor and nearby organs-at-risk structures.
|
|||
4017. |
Investigation of A Fast-volumetric Four-dimensional Magnetic Resonance Imaging Technique for Abdominal Radiotherapy Tumor Motion Management
Tian Li1, Haonan Xiao1, Ge Ren1, Weiwei Liu2, Yibao Zhang2, Hao Wu2, Weihu Wang2, and Jing Cai1
1Department of Health Technology and Informatics, The Hong Kong Polytechnic University, Hong Kong, Hong Kong, 2Key Laboratory of Carcinogenesis and Translational Research (Ministry of Education/Beijing), Department of Radiation Oncology, Beijing Cancer Hospital & Institute, Peking University Cancer Hospital & Institute, Beijing, China, Beijing, China
Motion management plays an important role in abdominal cancer radiotherapy. Current motion measurement method using 2D Cine MRI is inefficient. However, there is no commercial four-dimensional MRI available for motion management. In this study, we aim to investigate a fast-volumetric four-dimensional MRI technique using commercial sequence for tumor motion management in liver cancer patient. Our preliminary results shown that the commercially available TWIST-VIBE 4D-MRI sequence is capable of measuring liver tumor motion accurately with an acceptable tumor contrast.
|
|||
4018.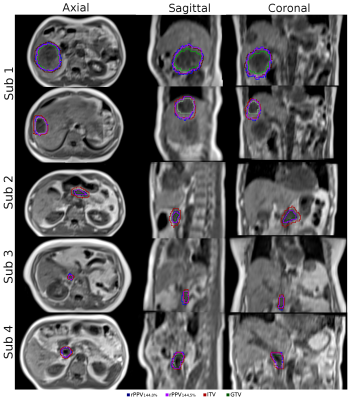 |
Subject-specific positional probability volume mapping for internal target volume determination in Radiotherapy
Oi Lei Wong1, Jing Yuan1, Darren MC Poon2, Yi Hang Zhou1, Siu Ki Yu1, and Kin Yin Cheung1
1Medical Physics and Research, Hong Kong Sanatorium, Hong Kong, Hong Kong, 2Comprehensive Oncology Center, Hong Kong Sanatorium, Hong Kong, Hong Kong
A novel ITV determination technique based on the volume of positional probability distribution (PPV) generated by volumetric 4DMRI was proposed and verified on cancer patients. For large targets, both PPV and 4D-CT generated ITV were similar with relatively large DSC. For small targets, however, relatively small DSC was observed, where poor tumor visibility in 4D-CT may be the cause.
|
|||
4019.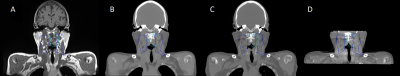 |
Promising results using synthetic CT for 2D and 3D patient positioning in head and neck radiotherapy
Emilia Palmér1, Fredrik Nordström1,2, Anna Karlsson1,2, Karin Petruson3, Maria Ljungberg1,2, and Maja Sohlin1,2
1Department of Radiation Physics, Institute of Clinical Sciences, Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden, 2Department of Medical Physics and Biomedical Engineering, Sahlgrenska University Hospital, Gothenburg, Sweden, 3Department of Oncology and Radiotherapy, Institute of Clinical Sciences, Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden
In an MRI-only radiotherapy workflow, in addition to enabling absorbed dose calculation the generated synthetic CT (sCT) must also be valid for patient positioning at treatment course. To evaluate MRI-only patient positioning for head and neck cancer patients, fourteen 3D cone beam CTs were retrospectively registered to CT and sCT. Further, original Digital Reconstructed radiographs originating from the CT and synthetic Digital Reconstructed radiographs originating from the sCT, were retrospectively registered to orthogonal projections. The small mean difference between the registrations showed that sCT could replace the CT for both 3D and 2D head and neck radiotherapy patient positioning.
|
|||
4020.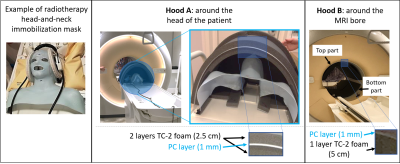 |
Damping acoustic noise for MRI in Radiotherapy Settings
Erik R Huijing1, Femke Wetzels1, Edwin Versteeg1, Koenraad Rhebergen1, Simon Woodings1, Dennis Klomp1, Marielle Philippens1, Nico van den Berg2, and Stefano Mandija3
1UMC Utrecht, Utrecht, Netherlands, 2Computational Imaging Group for MR Diagnostic & Therapy, UMC Utrecht, Utrecht, Netherlands, 3Computational Imaging Group for MR Diagnostic & Therapy, University Medical Center Utrecht, Utrecht, Netherlands
We present two hoods for acoustic noise damping for MRI in Radiotherapy. This is especially relevant for brain and head-and-neck patients who are scanned repetitively inside immobilization masks, which prevent wearing all the required earing protection devices. The hoods show good noise damping (average at least 10 dB attenuation) and minimal radiation dose attenuation (<1%), making them suitable also for MR-linac systems. Subjective results from a survey on 15 volunteers show that the hoods are well tolerated and do not increase significantly the feeling of claustrophobia.
|
|||
4021.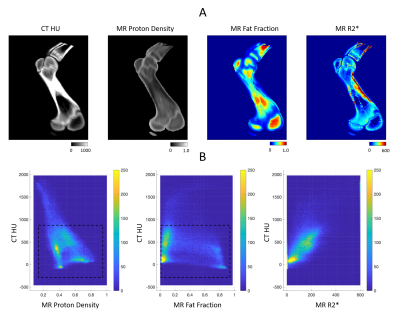 |
UTE-MRI complements CT in bone characterization for improved proton therapy dose calculation
Xin Miao1, Raanan Marants2, Thomas Benkert3, Evangelia Kaza2, Jeremy Bredfeldt2, and Atchar Sudhyadhom2
1Siemens Medical Solutions USA Inc., Boston, MA, United States, 2Department of Radiation Oncology, Dana-Farber/Brigham and Women's Cancer Center, Boston, MA, United States, 3Siemens Healthcare GmbH, Erlangen, Germany
CT-based proton therapy dose calculation suffers from significant uncertainties that critically limit clinical efficacy. Previous works demonstrated improved proton range calculation by combining quantitative MRI with CT. This study extends those works into bone, a challenging region for tissue characterization. CT and a novel UTE MRI technique were used to investigate their complimentary information for bone characterization. Both phantom and in vivo experiments showed that combining UTE-MRI and CT measurements achieved accurate classification of bone types. Understanding of bone types can have significant implications on the determination of bone tissue composition and, ultimately, accuracy of radiation delivery in proton therapy.
|
|||
 |
4022.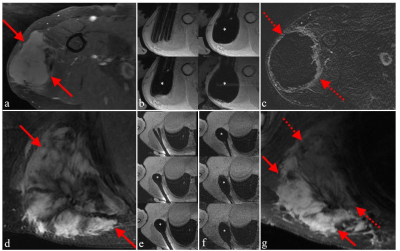 |
Magnetic Resonance Guided Percutaneous Cryoablation of Extra-abdominal Desmoid Tumors: An Institutional Experience
Ali Agely1, Vipul Sheth1, Pejman Ghanouni1, and Ryan L. Brunsing1
1Radiology, Stanford University, Palo Alto, CA, United States
Desmoid tumors are challenging to control with chemotherapy, surgery, or radiation. This retrospective review evaluated patients with extra-abdominal desmoid tumors treated with MR-guided cryoablation at our institution over two years. The primary endpoint was tumor volume change before and 3 months after cryoablation; the secondary endpoint was the change in health status assessed at the same interval. Our study demonstrates MR-guided cryoablation results in the reduction of both tumor size and improvement in health status scores. No severe adverse events occurred. We conclude that MR-guided cryoablation is an effective and safe treatment option for desmoid tumors.
|
||
4023.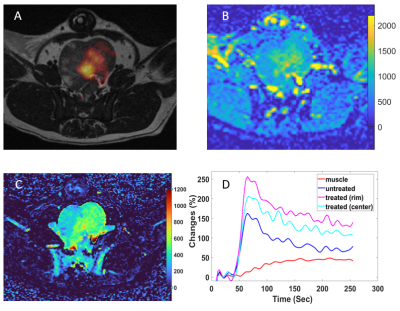 |
PET/MRI Assessment of 90Yttrium Prostate Localization and Acute Response Following Intra-arterial Radioembolization in A Canine Model
Weiguo Li1,2, Kathleen Harris1, Amrutha Mylarapu1, Malcolm Burks1, Simone Raiter1, Vanessa Louise Gates1, Andrew Gordon1, Robert Lewandowski1, Riad Salem1, and Samdeep Mouli1
1Radiology, Northwestern University, Chicago, IL, United States, 2Bioengineering, University of Illinois at Chicago, Chicago, IL, United States
Local-regional therapy of prostate cancer with 90Yttrium (90Y) radioembolization is a novel radiotherapy approach that delivers high-dose radiation therapy with minimal non-target radiation. However, currently no accurate way exists to evaluate radiation effects noninvasively following embolization. In this study, we sought to apply PET/MRI to assess biodistribution of 90Y and estimate effects of treatment following 90Y prostate artery radioembolization in a dog prostate model.
|
|||
4024.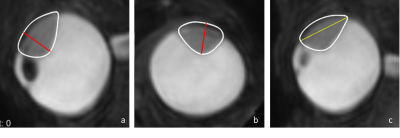 |
Improved therapy planning for eye tumours: a tumour geometry comparison between MRI and conventional ultrasound
L. Klaassen1,2, M.G. Jaarsma-Coes1,2, T.A. Ferreira2, T.H.K. Vu1, M. Marinkovic1, C.R.N. Rasch3, G.P.M. Luyten1, and J.W.M. Beenakker1,2
1Department of Ophthalmology, LUMC, Leiden, Netherlands, 2Department of Radiology, LUMC, Leiden, Netherlands, 3Department of Radiotherapy, LUMC, Leiden, Netherlands
Ocular magnetic resonance imaging, enabling 3D tumour imaging and providing better soft tissue contrast than conventional ultrasound, is increasingly used for uveal melanoma. The aim of this research was to determine the difference in geometrical tumour measurements between ultrasound and MRI. For this purpose, tumour prominence and largest basal diameter were calculated automatically based on MR imaging and compared to the US measurements. Differences >0.5mm were observed in 55% of prominence measurements and 80% of LBD measurements. Furthermore, automatically measuring tumour geometry based on 3D MR imaging lead to the discovery of inconsistencies in measurement definitions within and across disciplines.
|
The International Society for Magnetic Resonance in Medicine is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians.