Oral
Lung
ISMRM & SMRT Annual Meeting • 15-20 May 2021

| Concurrent 5 | 16:00 - 18:00 | Moderators: Anne Slawig & Jason Woods |
 |
0589.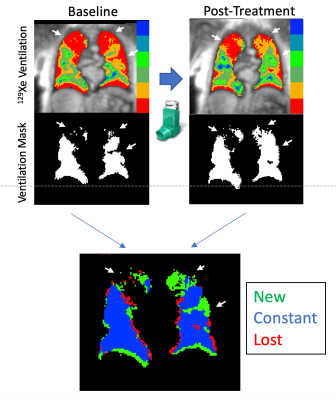 |
Regional Changes in Ventilation Following Bronchodilation in COPD Are Not Associated With Improved Gas Exchange on Xenon-129 MRI
David Mummy1, Erika Coleman2, Ziyi Wang3, Elianna Bier3, Junlan Lu4, Bastiaan Driehuys1,3,4, and Yuh-Chin Huang2
1Radiology, Duke University, Durham, NC, United States, 2Medicine, Duke University, Durham, NC, United States, 3Biomedical Engineering, Duke University, Durham, NC, United States, 4Medical Physics, Duke University, Durham, NC, United States
Hyperpolarized 129Xe MRI images acquired pre/post-bronchodilator treatment in COPD (N=17) provide a new means of evaluating gas evaluating gas exchange in regions of new, existing, and lost ventilation. Here we demonstrate via longitudinal image registration that, despite improvements in FEV1 and regional ventilation following treatment, no changes in region-based measures of 129Xe barrier or RBC signal were observed. This suggests the presence of persistent vascular abnormalities in COPD that are not addressed by bronchodilation.
|
|
0590. |
19F-MRI of inhaled perfluoropropane in patients with asthma and patients with COPD pre- and post-bronchodilator therapy
Mary A. Neal1, Benjamin J. Pippard1,2, Ian Forrest3, Rod A. Lawson4, Holly F. Fisher5, John N. S. Matthews5, Kieren G. Hollingsworth1,2, A. John Simpson1, Jim M. Wild6, and Peter E. Thelwall1,2
1Translational and Clinical Research Institute, Newcastle University, Newcastle upon Tyne, United Kingdom, 2Newcastle Magnetic Resonance Centre, Newcastle University, Newcastle upon Tyne, United Kingdom, 3Respiratory Medicine, Newcastle upon Tyne Hospitals NHS Foundation Trust, Newcastle upon Tyne, United Kingdom, 4Respiratory Medicine, Sheffield Teaching Hospitals NHS Foundation Trust, Sheffield, United Kingdom, 5Population Health Sciences Institute, Newcastle University, Newcastle upon Tyne, United Kingdom, 6POLARIS, Department of IICD, University of Sheffield, Sheffield, United Kingdom
19F-MRI of inhaled perfluoropropane can be used for assessment of pulmonary ventilation. Static breath hold 19F-MR images were acquired pre- and post-bronchodilator following inhalation of a perfluoropropane/oxygen gas mixture in patients with asthma and patients with chronic obstructive pulmonary disease (COPD). Percentage ventilated lung volume (%VV) was calculated from each of the 19F-MR images. %VV was significantly reduced in both patient groups, and between pre- and post-bronchodilator acquisitions in the asthmatic patient group. A strong positive correlation between %VV and spirometric indices was revealed. Gas inhalations were well tolerated by all participants, with no adverse events.
|
||
0591. |
Response of Hyperpolarized 129Xe MRI measures of ventilation and gas-exchange to anti-fibrotic treatment in Idiopathic Pulmonary Fibrosis
Andrew D Hahn1, Katie J Carey1,2, Nathan D Sandbo3, Jeff Kammermann1, Robert V Cadman3, David G Mummy4, Mark L Schiebler1,2, Amy Malik3, and Sean B Fain1,2,5
1Medical Physics, University of Wisconsin - Madison, Madison, WI, United States, 2Radiology, University of Wisconsin - Madison, Madison, WI, United States, 3Medicine, University of Wisconsin - Madison, Madison, WI, United States, 4Radiology, Duke University, Durham, NC, United States, 5Biomedical Engineering, University of Wisconsin - Madison, Madison, WI, United States
Predicting outcomes and monitoring longitudinal treatment response in IPF is unreliable using currently available clinical biomarkers. We investigate associations between hyperpolarized 129Xe MRI biomarkers of ventilation and gas exchange and treatment with anti-fibrotic medication in IPF patients over a 1-year period. Anti-fibrotic treatment was associated with improved ventilation and gas exchange, relative to no anti-fibrotic treatment, after 1 year. Within-patient improvements in gas exchange were significantly larger in patients treated with anti-fibrotic medications. No longitudinal associations were found between anti-fibrotic treatment and spirometry, suggesting the imaging biomarkers may be more useful for monitoring anti-fibrotic treatment response in IPF.
|
||
 |
0592.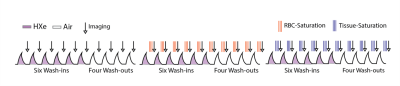 |
Monitoring Patients with Endobronchial Valve Interventions Using a Multifaceted Hyperpolarized Xenon Lung Function Assessment
Hooman Hamedani1, Stephen Kadlecek1, Faraz Amzajerdian1, Ryan Baron1, Kai Ruppert1, Ian Duncan1, Luis Loza1, Tahmina Achekzai1, Maurizio Cereda1, and Rahim R. Rizi2
1University of Pennsylvania, Philadelphia, PA, United States, 2Radiology, University of Pennsylvania, Philadelphia, PA, United States
Here, we present an approach for comprehensively assessing the lung’s response to an intervention. Using our multi-breath approach during tidal breathing, we evaluated whether after a Treatment with Zephyr Endobronchial Valves, ventilation is successfully redistributed to the healthier lung, and whether this shift in ventilation can effectively improve gas exchange in non-targeted lobes. We showed gas exchange was more than doubled in the upper left lobe, exceeding the modest ventilation increase observed after occlusion of the LL lobe, likely indicating dramatically improved Q. Notably, right lung function was also improved, perhaps due to normalized breathing mechanics.
|
|
 |
0593.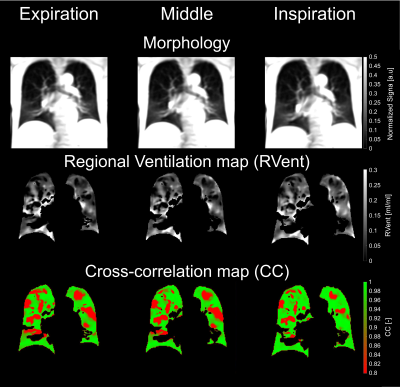 |
Registration on different lung volumes and its influence on ventilation and perfusion parameters derived by phase-resolved functional lung MRI
Filip Klimeš1,2, Andreas Voskrebenzev1,2, Lea Behrendt1,2, Marcel Gutberlet1,2, Gesa Helen Pöhler1,2, Till Frederik Kaireit1,2, Cristian Crisosto1,2, Frank Wacker1,2, and Jens Vogel-Claussen1,2
1Institute of Diagnostic and Interventional Radiology, Hannover Medical School, Hannover, Germany, 2Biomedical Research in Endstage and Obstructive Lung Disease Hannover (BREATH), German Centre for Lung Research (DZL), Hannover, Germany
Correction of lung motion is a mandatory step for the voxel-wise signal analysis of Fourier Decomposion (FD) based methods, such as phase-resolved functional lung (PREFUL) MRI. Usually, all images are registered towards one fixed image in intermediate lung position. In this work, a group oriented registration approach with three different target images (expiration, middle, inspiration) was tested and the influence on functional parameters derived by PREFUL was evaluated in 41 study participants. While small significant differences were observed, high absolute agreement of all functional ventilation and perfusion parameters was found indenpedent on the chosen target volume.
|
|
0594.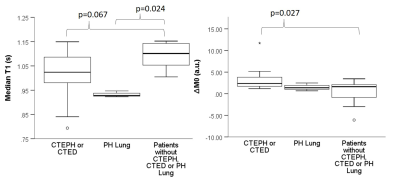 |
M0 and T1 mapping for differentiation of perfusion defects in patients with CTEPH and CTED.
Laura Saunders1, Paul J. C. Hughes1, Dave Capener1, David G Kiely1,2, Jim M Wild1, and Andy J Swift1
1Infection Immunity and Cardiovascular Disease, University of Sheffield, Sheffield, United Kingdom, 2Sheffield Pulmonary Vascular Disease Unit, Sheffield, United Kingdom
Identifying the cause of lung perfusion defects is vital for chronic thromboembolic pulmonary hypertension (CTEPH) or chronic thromboembolic disease (CTED) diagnosis. 30 patients with suspected CTEPH underwent Look-Locker M0 and T1 mapping, 16/30 were diagnosed with CTEPH or CTED. Co-registered peak perfusion maps were used to identify perfusion defects. T1 was significantly lower in perfusion defects in all patients. Patients with CTEPH or CTED had significantly lower M0 in non-perfused lung, whereas control patients did not have significantly differences between perfused and non-perfused lung. Lung M0 maps may allow differentiation of perfusion defects in patients with CTEPH/CTED from other patients.
|
||
0595.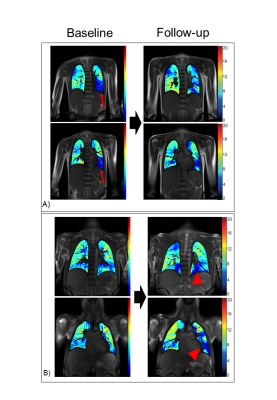 |
One-year follow-up of functional lung MRI in children with cystic fibrosis
Corin Willers1, Lukas Maager1, Bettina S. Frauchiger1, Kathryn Ramsey1, Grzegorz Bauman2,3, Orso Pusterla2,3, Oliver Bieri2,3, and Philipp Latzin1
1Division of Pediatric Respiratory Medicine, Department of Pediatrics,, Inselspital, Bern University Hospital, University of Bern, Switzerland, Bern, Switzerland, 2Division of Radiological Physics, Department of Radiology, University of Basel Hospital Basel, Basel, Switzerland, Basel, Switzerland, 3Department of Biomedical Engineering, University of Basel, Basel, Switzerland, Basel, Switzerland
Matrix Pencil MRI in cystic fibrosis is a sensitive and promising technique to monitor progression of lung disease, and is especially well-suited for children. In this work, we investigate the agreement between changes in functional lung MRI and in lung function tests during a 1-year follow-up period. We demonstrate the benefit of imaging to interpret changes in lung function correctly.
|
||
0596.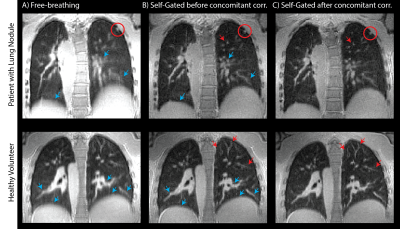 |
Optimized 3D spiral ultra-short echo time free-breathing pulmonary imaging on a high-performance low-field 0.55T scanner
Ahsan Javed1, Rajiv Ramasawmy1, Joel Moss2, Waqas Majeed3, Pan Su3, Thomas Benkert4, Himanshu Bhat3, and Adrienne E Campbell-Washburn5
1Cardiovascular Branch, Division of Intramural Research, National Heart, Lung, and Blood Institute, National Institutes of Health, Bethesda, MD, United States, 2Pulmonary Branch, Division of Intramural Research, National Heart, Lung, and Blood Institute, National Institutes of Health, Bethesda, MD, United States, 3Siemens Medical Solutions USA Inc., Malvern, PA, United States, 4Siemens Healthcare GmbH, Erlangen, Germany, 5Cardiovascular Branch, Division of Intramural Research, National Heart, Lung, and Blood Institute, National Institute of Health, Bethesda, MD, United States
Low signal in the lung parenchyma, and reduced signal-to-noise at 0.55T makes high resolution lung imaging challenging. SNR can be improved by using longer spiral readouts. However, these readouts are susceptible to artifacts from trajectory errors, and blurring from concomitant fields which are amplified at lower field strengths. Here we present an optimized self-gated, ultra-short echo time, stack-of-spirals acquisition which leverages inline corrections for trajectory imperfections, measurement drift, and concomitant fields to enable robust high resolution lung imaging on low field scanners. We also demonstrate the improvement in image quality in patients with lung nodules and Lymphangioleiomyomatosis (LAM).
|
||
0597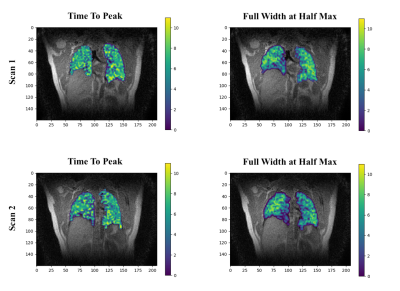 |
Intensity Based Visualization of Pulmonary Function Using Time to Peak and Full Width at Half Max Biomarkers on Ultrashort Echo Time (UTE) MRI Video Permission Withheld
Darren Hsu1, Fei Tan2, Michael Lustig3, and Peder E. Z. Larson4
1Department of Computer Science, University of California, Berkeley, Berkeley, CA, United States, 2Department of Bioengineering, University of California, Berkeley - University of California, San Francisco, San Francisco, CA, United States, 3Department of Electrical Engineering and Computer Sciences, University of California, Berkeley, Berkeley, CA, United States, 4Department of Radiology and Biomedical Imaging, University of California, San Francisco, San Francisco, CA, United States
The visualization of respiratory inhalation-exhalation cycles are applied to pulmonary MR images. Using 3D UTE phase resolved MR Images, respiratory phases were reconstructed from free breathing images. Applying signal intensity based methods, biomarker metrics such as time to signal intensity peak (TTP) or full width at half maximum (FWHM) intensity are extracted from the image. The resulting visualizations depict localized respiratory function to help clinicians understand the rate and velocity at which lung tissue expands from full inspiration to full expiration.
|
||
0598 |
CEST Imaging vs. Diffusion-Weighted Imaging vs. FDG-PET/CT vs. Combined Method: Prediction Capability for Recurrence in NSCLC Patients Video Permission Withheld
Yoshiharu Ohno1,2,3, Masao Yui4, Takeshi Yoshikawa3,5, Yoshimori Kassai4, Kaori Yamamoto4, Kazuhiro Murayama2, and Hiroshi Toyama1
1Radiology, Fujita Health University School of Medicine, Toyoake, Japan, 2Joint Research Laboratory of Advanced Medical Imaging, Fujita Health University School of Medicine, Toyoake, Japan, 3Division of Functional and Diagnostic Imaging Research, Department of Radiology, Kobe University Graduate School of Medicine, Kobe, Japan, 4Canon Medical Systems Corporation, Otawara, Japan, 5Diagnostic Radiology, Hyogo Cancer Center, Akashi, Japan
No major reports have been reported the comparison of capability for differentiating recurrence from non-recurrence groups in candidates for surgical resection due to lung cancer among CEST imaging, DWI and PET/CT. We hypothesized that CEST imaging, which was determined as APT-weighted (APTw) imaging at 3.5 ppm, had equal or better potential for prediction of postoperative recurrence prediction in postoperative lung cancer patients, when compared with DWI and FDG-PET/CT. The purpose of this study was to compare the prediction capability of among single- and multi-parametric approaches by APTw imaging, DWI, and FDG-PET/CT in NSCLC patients.
|
The International Society for Magnetic Resonance in Medicine is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians.