Eva Heckova1, Alexandra Lipka1, Assunta Dal-Bianco2, Bernhard Strasser1, Gilbert Hangel1,3, Paulus Rommer2, Petra Hnilicová4, Ema Kantorová5, Lukas Hingerl1, Stanislav Motyka1, Fritz Leutmezer2, Stephan Gruber1, Siegfried Trattnig1,6, and Wolfgang Bogner1
1High Field MR Centre, Department of Biomedical Imaging and Image-guided Therapy, Medical University of Vienna, Vienna, Austria, 2Department of Neurology, Medical University of Vienna, Vienna, Austria, 3Department of Neurosurgery, Medical University of Vienna, Vienna, Austria, 4Biomedical Center Martin, Jessenius Faculty of Medicine in Martin, Comenius University in Bratislava, Martin, Slovakia, 5Clinic of Neurology, Jessenius Faculty of Medicine in Martin, Comenius University in Bratislava, Martin, Slovakia, 6Christian Doppler Laboratory for Clinical Molecular MR Imaging, Vienna, Austria
1High Field MR Centre, Department of Biomedical Imaging and Image-guided Therapy, Medical University of Vienna, Vienna, Austria, 2Department of Neurology, Medical University of Vienna, Vienna, Austria, 3Department of Neurosurgery, Medical University of Vienna, Vienna, Austria, 4Biomedical Center Martin, Jessenius Faculty of Medicine in Martin, Comenius University in Bratislava, Martin, Slovakia, 5Clinic of Neurology, Jessenius Faculty of Medicine in Martin, Comenius University in Bratislava, Martin, Slovakia, 6Christian Doppler Laboratory for Clinical Molecular MR Imaging, Vienna, Austria
High-resolution MRSI at 7T can visualize
MS pathology not visible on clinical MRI. Metabolic abnormalities in
normal-appearing white matter and cortical gray matter, reflecting loss of
axonal integrity and neuroinflammation-induced astrogliosis, correlate with
clinical disability.

Figure 2: Abnormal metabolic images of
mI, NAA, and mI/NAA together with clinical MRI in patients with MS. Small
subcortical/juxtacortical lesions (A), which appear inconspicuous on
high-resolution MRI (indicated with blue arrows), are well depicted on mI/NAA
maps. In (B), red arrows indicate regions in the NAWM with increased mI only, and
yellow arrows indicate regions with increased mI and decreased NAA, where no,
or only diffuse changes are visible on clinical MRI. Green arrows indicate
white matter lesions, where elevated mI appears beyond T2-visible pathology.
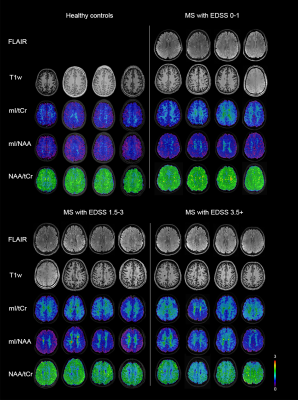
Figure 3: Examples of metabolic ratio
images and clinical MRI from healthy controls and MS patients with various
levels of clinical disability. mI/tCr and mI/NAA tended to be increased in the
NAWM of all patient subgroups, while NAA/tCr was decreased only in subgroups of
patients with mild and more severe clinical disability.
