Mary A. Neal1, Benjamin J. Pippard1,2, Ian Forrest3, Rod A. Lawson4, Holly F. Fisher5, John N. S. Matthews5, Kieren G. Hollingsworth1,2, A. John Simpson1, Jim M. Wild6, and Peter E. Thelwall1,2
1Translational and Clinical Research Institute, Newcastle University, Newcastle upon Tyne, United Kingdom, 2Newcastle Magnetic Resonance Centre, Newcastle University, Newcastle upon Tyne, United Kingdom, 3Respiratory Medicine, Newcastle upon Tyne Hospitals NHS Foundation Trust, Newcastle upon Tyne, United Kingdom, 4Respiratory Medicine, Sheffield Teaching Hospitals NHS Foundation Trust, Sheffield, United Kingdom, 5Population Health Sciences Institute, Newcastle University, Newcastle upon Tyne, United Kingdom, 6POLARIS, Department of IICD, University of Sheffield, Sheffield, United Kingdom
1Translational and Clinical Research Institute, Newcastle University, Newcastle upon Tyne, United Kingdom, 2Newcastle Magnetic Resonance Centre, Newcastle University, Newcastle upon Tyne, United Kingdom, 3Respiratory Medicine, Newcastle upon Tyne Hospitals NHS Foundation Trust, Newcastle upon Tyne, United Kingdom, 4Respiratory Medicine, Sheffield Teaching Hospitals NHS Foundation Trust, Sheffield, United Kingdom, 5Population Health Sciences Institute, Newcastle University, Newcastle upon Tyne, United Kingdom, 6POLARIS, Department of IICD, University of Sheffield, Sheffield, United Kingdom
19F-MRI of inhaled perfluoropropane was performed on patients with asthma (n=16) and COPD (n=13), pre and post bronchodilator. Ventilation defects with correlation to spirometry were observed. Defect volume reduced in patients with asthma after bronchodilator.

Figure 2: Central slices from 3D SPGR 19F-MR images of inhaled PFP in twelve representative participants. Equivalent slices pre- and post-bronchodilator from the 3D datasets are displayed. The original magnitude images are displayed, where no image processing has been applied other than selection of an appropriate lower windowing threshold to minimise visibility of background noise.
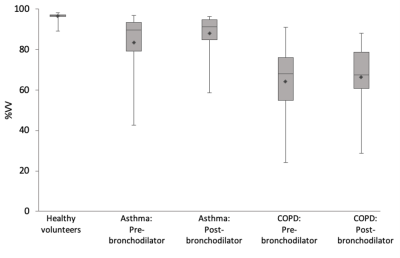
Figure 3: The distribution of %VV measurements from 19F-MRI images of inhaled perfluoropropane in patients with asthma (N = 14) and patients with COPD (N = 12), displayed beside %VV measurements of 38 healthy volunteers measured during an earlier phase of this study.7 Diamonds label the group means, with the 25th percentile, median, and 75th percentiles marked by the three horizonal lines in each box plot. A significant change in %VV was measured between pre- and post-bronchodilator measurements within the asthma cohort, though not for patients with COPD.
