Andrew D Hahn1, Katie J Carey1,2, Nathan D Sandbo3, Jeff Kammermann1, Robert V Cadman3, David G Mummy4, Mark L Schiebler1,2, Amy Malik3, and Sean B Fain1,2,5
1Medical Physics, University of Wisconsin - Madison, Madison, WI, United States, 2Radiology, University of Wisconsin - Madison, Madison, WI, United States, 3Medicine, University of Wisconsin - Madison, Madison, WI, United States, 4Radiology, Duke University, Durham, NC, United States, 5Biomedical Engineering, University of Wisconsin - Madison, Madison, WI, United States
1Medical Physics, University of Wisconsin - Madison, Madison, WI, United States, 2Radiology, University of Wisconsin - Madison, Madison, WI, United States, 3Medicine, University of Wisconsin - Madison, Madison, WI, United States, 4Radiology, Duke University, Durham, NC, United States, 5Biomedical Engineering, University of Wisconsin - Madison, Madison, WI, United States
Anti-fibrotic treatment of IPF was associated with improved hyperpolarized 129Xe MRI ventilation imaging biomarkers of ventilation and gas exchange after 1 year.

Figure 1. Boxplots of HVP and RBC:Barrier measurements from the 1-year follow-up (a,b), and within-patient differences in these metrics over the 1-year monitoring period (c,d). Significant differences (P<0.05) between medication groups are indicated by asterisks. Note that no significant differences were found between groups at baseline (data not shown).
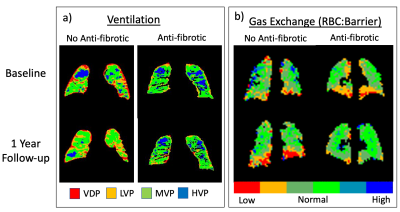
Figure 2. Example parametric maps of ventilation (a) and RBC:Barrier ratio (b) from an IPF patient not taking anti-fibrotic medication (male, age 65) and an IPF patient treated with anti-fibrotics (male, age 60) at baseline and after 1 year. Note the reduction in HVP over time in the no anti-fibrotic case (a, left), with HVP apparently maintained with anti-fibrotic medication (a, right). Similarly, RBC:Barrier appears to decrease over time in the no anti-fibrotic patient (b, left), and recover in the patient taking anti-fibrotics (b, right).
