Christopher C Conlin1, Christine H Feng2, Leonardino A Digma2, Ana E Rodriguez-Soto1, Joshua M Kuperman1, Dominic Holland3, Rebecca Rakow-Penner1, Tyler M Seibert1,2,4, Anders M Dale1,3,5, and Michael E Hahn1
1Department of Radiology, UC San Diego School of Medicine, La Jolla, CA, United States, 2Department of Radiation Medicine and Applied Sciences, UC San Diego School of Medicine, La Jolla, CA, United States, 3Department of Neurosciences, UC San Diego School of Medicine, La Jolla, CA, United States, 4Department of Bioengineering, UC San Diego Jacobs School of Engineering, La Jolla, CA, United States, 5Halıcıoğlu Data Science Institute, UC San Diego, La Jolla, CA, United States
1Department of Radiology, UC San Diego School of Medicine, La Jolla, CA, United States, 2Department of Radiation Medicine and Applied Sciences, UC San Diego School of Medicine, La Jolla, CA, United States, 3Department of Neurosciences, UC San Diego School of Medicine, La Jolla, CA, United States, 4Department of Bioengineering, UC San Diego Jacobs School of Engineering, La Jolla, CA, United States, 5Halıcıoğlu Data Science Institute, UC San Diego, La Jolla, CA, United States
Multicompartmental modeling
was applied to develop an empirical tissue classifier for identifying bone
lesions in whole-body DWI. This classifier considerably
outperformed one based on conventional ADC values.
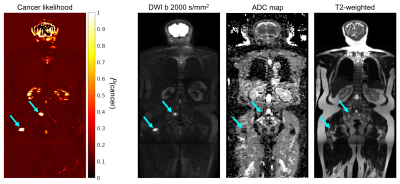
Figure 3: RSI cancer-likelihood map of a patient with
prostate-cancer metastases in the pelvis and femur (cyan arrows), compared against
conventional MR images. Bone lesions show a very high likelihood value [probability
of being cancerous; P(cancer)] compared to surrounding normal tissue.
Normal tissue is generally less pronounced on the likelihood map than on
conventional MR images. False positive signal remains, however, in organs with dense
cellular arrangement like the kidneys and brain.
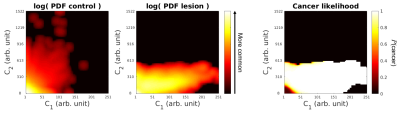
Figure 2: RSI signal distributions for normal tissue and bone
lesions. The joint C1,C2 probability density functions (PDFs) are shown for
normal control tissue (left) and bone lesions (middle). Both PDFs are shown after
log transformation to better show less frequent combinations of C1
and C2. The posterior probability distribution on the right is
derived from the PDFs and shows the likelihood of cancer [P(cancer)]
given particular C1 and C2 values. High C1
signal in particular is indicative of cancer.
