Christopher C Conlin1, Christine H Feng2, Leonardino A Digma2, Ana E Rodriguez-Soto1, Joshua M Kuperman1, Dominic Holland3, Rebecca Rakow-Penner1, Tyler M Seibert1,2,4, Michael E Hahn1, and Anders M Dale1,3,5
1Department of Radiology, UC San Diego School of Medicine, La Jolla, CA, United States, 2Department of Radiation Medicine and Applied Sciences, UC San Diego School of Medicine, La Jolla, CA, United States, 3Department of Neurosciences, UC San Diego School of Medicine, La Jolla, CA, United States, 4Department of Bioengineering, UC San Diego Jacobs School of Engineering, La Jolla, CA, United States, 5Halıcıoğlu Data Science Institute, UC San Diego, La Jolla, CA, United States
1Department of Radiology, UC San Diego School of Medicine, La Jolla, CA, United States, 2Department of Radiation Medicine and Applied Sciences, UC San Diego School of Medicine, La Jolla, CA, United States, 3Department of Neurosciences, UC San Diego School of Medicine, La Jolla, CA, United States, 4Department of Bioengineering, UC San Diego Jacobs School of Engineering, La Jolla, CA, United States, 5Halıcıoğlu Data Science Institute, UC San Diego, La Jolla, CA, United States
An optimized 4-compartment model
better characterized whole-body diffusion than conventional DWI methods. Compartmental
signal-contributions revealed by this model may help to detect and quantify prostate-cancer
bone involvement.
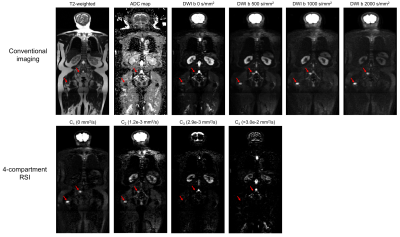
Figure 3: Coronal
whole-body images of a patient with metastatic bone lesions in the pelvis and
femur (red arrows). Conventional MR images are shown in the top row. The bottom
row shows the signal-contribution (Ci) maps for the optimized 4-compartment
RSI model. The corresponding Di
of each model compartment is listed in parentheses next to the compartment
label.
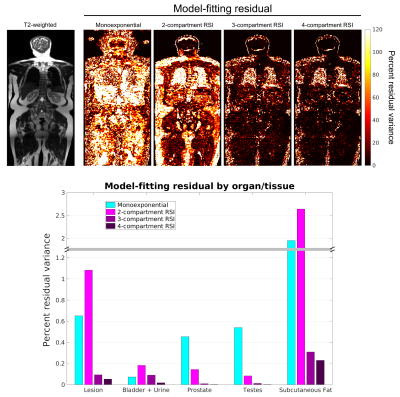
Figure 2: Model-fitting
residual at the voxel- and ROI-level. The top row shows voxel-wise maps of
fitting residual in a coronal plane of the same patient using different models.
A T2-weighted image of the same plane is included for reference. The bottom
figure graphs the fitting residual within all lesion and tissue-specific ROIs. A
better fit to the data was observed with the 4-compartment RSI model than with
the conventional monoexponential model or the lower-order RSI models.
