Myriam Jaarsma-Coes1,2, Teresa Ferreira1, Marina Marinkovic2, Khanh Vu2, Gre Luyten2, Coen Rasch3, Berit Verbist1, and Jan-Willem Beenakker1,2
1Radiology, Leiden University Medical Center, Leiden, Netherlands, 2Ophthalmology, Leiden University Medical Center, Leiden, Netherlands, 3Radiotherapy, Leiden University Medical Center, Leiden, Netherlands
1Radiology, Leiden University Medical Center, Leiden, Netherlands, 2Ophthalmology, Leiden University Medical Center, Leiden, Netherlands, 3Radiotherapy, Leiden University Medical Center, Leiden, Netherlands
A dedicated MRI protocol helps to improve proton beam radiation planning for uveal melanoma patients, as it provides a 3D visualisation of the radiographic marker-tumor relation compared to the conventional peroperative optical measurement.
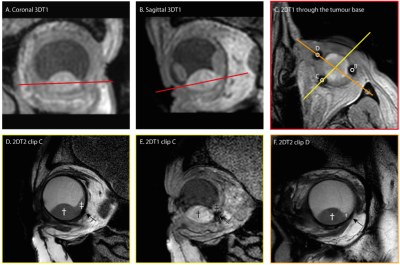
A,B). Coronal and sagittal view of the tumor are used to plan the scan to locate the clips.
C) 2DT1 scan trough the base clearly show the clips and is used to plan the subsequent scans perpendicular to the tumor base and through centre of the tumour and centre of clip C/D.
D,E). T2 spin echo sequence and T1 gradient echo showing the tumour (dagger), retinal detachment (double dagger) and clip (arrow). The clip location is better visualized on the gradient echo sequence, while a more accurate measurement can be made on the spin echo sequence.
F) T2 image of clip D.