Oral
State-of-the-Art Lung MR Imaging I
ISMRM & ISMRT Annual Meeting & Exhibition • 10-15 May 2025 • Honolulu, Hawai'i

| 16:00 |
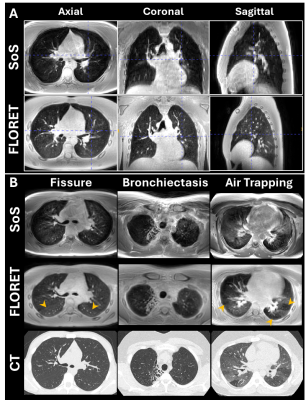 |
0303. Evaluating
Stack-of-Stars and FLORET 3D Ultrashort Echo Time MRI to Assess
Structural Pathology in Cystic Fibrosis Lung Disease

A. Bdaiwi, M. Willmering, J. Plummer, R. Hussain, Z.
Cleveland
Cincinnati Children's Hospital Medical Center, Cincinnati, United States
Impact: Compared to Stack-of-Stars, FLORET 3D-UTE,
provides isotropic sampling and better respiratory gating
and thus enabled superior lung imaging in pwCF.
Reader-scoring of lung abnormalities correlated better with
CT scores, suggesting superior clinical utility.
|
| 16:12 |
 |
0304. Comparison
of signal- and volume-based ventilation-weighted assessment
using 3D FLORET UTE MRI in patients with various pulmonary
disease

F. Klimeš, J. Plummer, A. Voskrebenzev, M. Gutberlet, M.
Wernz, M. Willmering, A. Matheson, A. Bdaiwi, F. Wacker,
J. Woods, Z. Cleveland, L. Walkup, J. Vogel-Claussen
Hannover Medical School, Hannover, Germany
Impact: Although both proton lung MRI methods
successfully identified ventilation defects, the stronger
correlation between signal-based (RVent) and 129Xe
MRI indicates that RVent may provide a more reliable
assessment of lung ventilation in clinical applications in
comparison to volume-based (JVent) parameter.
|
| 16:24 |
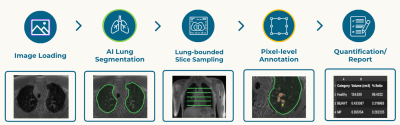 |
0305. Artificial
Intelligence-assisted Pixel-level Lung (APL) Scoring for Fast
and Accurate Quantification in Ultra-short Echo-time MRI
B. Xin, R. Hickey, T. Blake, J. Jin, C. Wainwright, T.
Benkert, A. Stemmer, P. Sly, D. Coman, J. Dowling
CSIRO, Sydney, Australia
Impact: AI-assisted
pixel-level scoring significantly improved the efficiency
and accuracy of lung MRI quantification, which has the
potential to streamline the clinical workflow of lung MRI
analysis for cystic fibrosis patients and be extended to
other lung diseases (e.g., bronchopulmonary dysplasia).
|
| 16:36 |
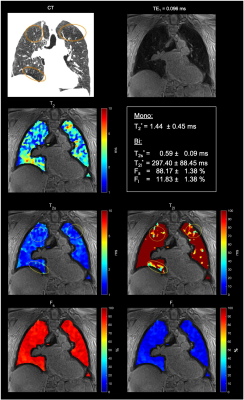 |
0306. Ultrashort
TE Imaging with Tight Intervals (δTE) for T2* Mapping in COPD:
Toward a Biomarker for Lung Structural Changes

V. Malis, Y. Kassai, Y. Kuwatsuru, A. Mesa, A. Yen, A.
Malhotra, D. Conrad, M. Miyazaki
UC San Diego, San Diego, United States
Impact: The δTE UTE technique enables safe, non-ionizing
imaging suitable for repeated exams in longitudinal
monitoring of COPD progression. By enhancing T2*
mapping sensitivity, it shows promise as a potential
biomarker for detecting subtle lung changes, complementing
current CT assessments.
|
| 16:48 |
 |
0307. Free-breathing
3D pulmonary ventilation mapping at 0.55T using Stack-of-Spiral
Out-in bSSFP

Z. Zhao, N. Lee, B. Tasdelen, X. Miao, Y. Tian, B. Li,
S. Cui, K. Nayak
University of Southern California, Los Angeles, United States
Impact: The proposed approach for 3D regional
ventilation mapping requires 5min is feasible and provides
consistent measurements and show good agreements with PREFUL
in healthy volunteers. This may improve the diagnosis and
evaluation of patients with pulmonary dysfunction.
|
| 17:00 |
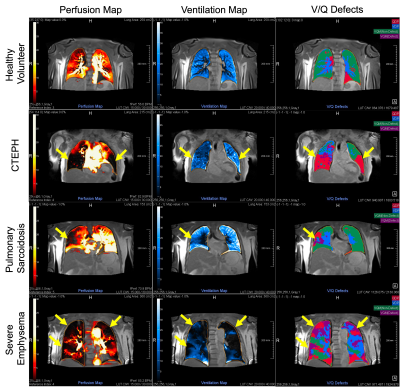 |
0308. Low-Field
(0.55T) Phase-resolved Functional Lung (PREFUL) MRI for
Evaluating Ventilation and Perfusion in Pulmonary Diseases
D. Capaldi, D. Baria, P. Deo, Y. J. Lee, P. Su, X. Miao, R.
Grimm, A. Voskrebenzev, J. Vogel-Claussen, J. Scholey, L.
Singer, Y. Yang, P. Larson, J. H. Sohn
UCSF, San Francisco, United States
Impact: Low-field PREFUL MRI enables non-invasive,
high-quality lung imaging, detecting pronounced ventilation
and perfusion defects in patients with lung disease. This
advancement underscores low-field MRI’s unique potential for
accessible, non-contrast enhanced, high-quality pulmonary
function assessment across diverse conditions.
|
| 17:12 |
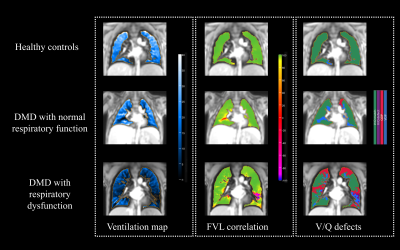 |
0309. Characterizing
respiratory dysfunction in Duchenne muscular dystrophy using
phase‐resolved functional lung (PREFUL) MRI
K. Xu, H. Xu, Y. Chen, T. Yin, R. Grimm, Y. Guo
West China Second University Hospital, Sichuan University, Chengdu, China
Impact: Our demonstration of a detectable decline in VDP
suggests that PREFUL MRI might represent a new noninvasive
tool for the functional assessment of lung even in the early
phase of respiratory compromise in children with DMD.
|
| 17:24 |
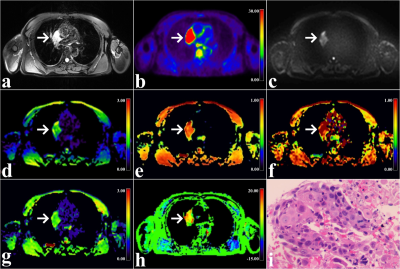 |
0310. Continuous-time
random walk and amide proton transfer-weighted imaging to
predict lymphovascular space invasion in non-small cell lung
cancer
N. Meng, Q. Chen, X. Yu, J. Pan, X. Chen, J. Yuan, Y. Yang,
Z. Wang, M. Wang
Henan Provincial People’s Hospital & Zhengzhou University People’s Hospital, Zhengzhou, China
Impact: The analysis of tumour glucose metabolism, water
molecule diffusion, temporal / spatial heterogeneities, and
mobile proteins / peptides measurement
at multiparametric 18F-FDG PET/MRI enables the prediction of
LVSI in NSCLC.
|
| 17:36 |
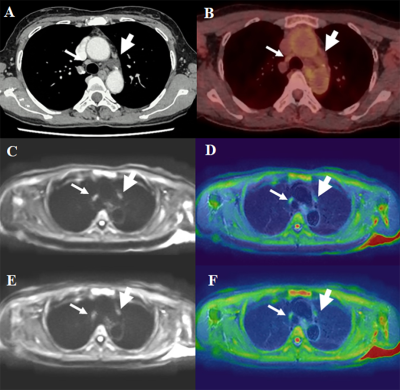 |
0311. Reverse
Encoding Distortion Correction (RDC) on DWI: Improving Image
Quality and Diagnosis of Lymph Node Metastasis in Non-Small Cell
Lung Cancer
Y. Ohno, K. Yamamoto, Y. Sano, M. Ikedo, M. Ozaki, M. Yui,
H. Nagata, T. Ueda, M. Nomura, T. Yoshikawa, D. Takenaka, Y.
Ozawa
Fujita Health University School of Medicine, Toyoake, Japan
Impact: RDC DWI has better potentials for improving
distortion, image quality and diagnosis of lymph node
metastasis as compared with cDWI and FDG-PET/CT in NSCLC
patients.
|
| 17:48 |
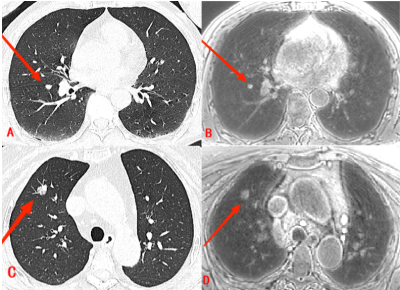 |
0312. Clinical
Application of Free-Breathing 3D Ultra-Short Echo Time Sequences
to Detect Lung Nodules
Z. Zhou, Z. Guo, Y. Ge, X. Kan, B. Thomas, J. An, M. Wang
Fuwai Henan Hospital, Chinese Academy of Medical Sciences, Zhengzhou, China
Impact: UTE, an emerging non-radiative examination
protocol, demonstrates great potential in detecting,
diagnosing, and providing short-term follow-up of lung
nodules and is poised to become an important tool for early
screening and diagnosis of lung cancer.
|
The International Society for Magnetic Resonance in Medicine is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians.