Power Pitch
Frontiers in Neuro-Oncology Imaging
ISMRM & ISMRT Annual Meeting & Exhibition • 10-15 May 2025 • Honolulu, Hawai'i

| 08:15 |
 |
Screen Number: 1
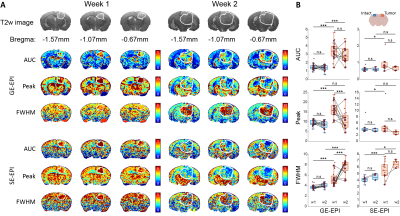
0066. Characteristics
of glioma tumor perfusion in mice with BOLD-DSC MRI
P. A. Chu Dang, S-E Ryu, J. Yei, T. T. Le, S. H. Choi, S.
Ryu, N. K. Lee, C. G. Park, M. Suh, S-G Kim
Center for Neuroscience Imaging Research (CNIR), Institute for Basic Science (IBS), Suwon, Korea, Republic of
Impact: BOLD-DSC is used as a sensitive and repeatable
tool to longitudinal investigate glioma tumor perfusion
during development, giving an insight into the vasculature
change by directly observing AUC, peak and FWHM.
|
| 08:17 |
 |
Screen Number: 2
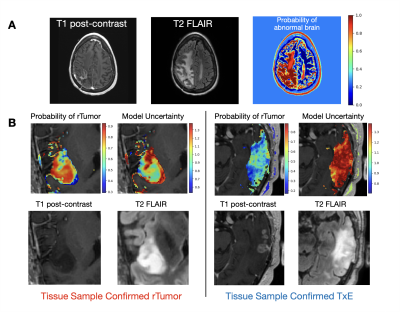
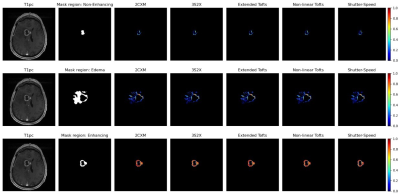
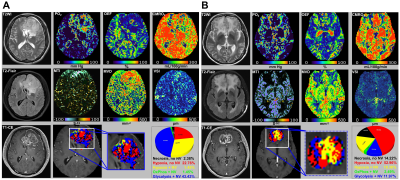
0067. Spatial
mapping of treatment-induced effects with multi-parametric MRI
correlate with survival in patients with recurrent GBM
J. Ellison, N. Tran, T. Luks, A. Jakary, J. Cluceru, J.
Phillips, A. Molinaro, V. Pedoia, A. Shai, D. Nair, J.
Villanueva-Meyer, M. Berger, S. Hervey-Jumper, M. Aghi, S.
Chang, J. Lupo
UCSF, San Francisco, United States
Impact: Spatial maps of recurrent glioma and
treatment-effects that account for normal brain demonstrate
reliable performance for mapping glioma beyond the visually
identifiable lesion with anatomical MRI. Spatial prediction
features are associated with survival and may enhance
treatment decisions.
|
| 08:19 |
 |
Screen Number: 3
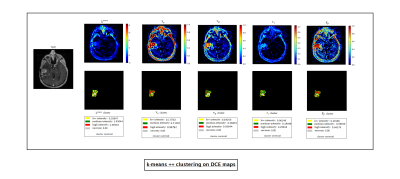
0068. Clustering-Based
Multiparametric MRI for Differentiation Between True Tumor
Progression and Pseudoprogression in Glioblastoma
S. Basak, G. W Kostrzanowska, S. Bera, A. Rajan, S. Chawla,
H. Poptani, S. Bhaduri
TCG Centres of Research and Education in Science and Technology (TCG CREST), Kolkata, India
Impact: These results demonstrate the importance of
vascular permeability in tumor assessment and establish Ktrans and
Kep along
with tumor volume as essential parameters for
differentiating true progression from treatment effects.
|
| 08:21 |
 |
Screen Number: 4
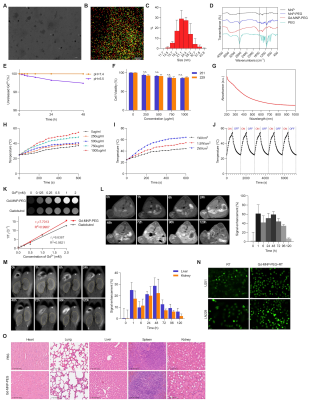
0069. MRI-guided
thermoradiotherapy of glioblastoma multiforme using Gd3+-loaded
melanin nanoparticles reverses anoikis resistance pathway
Y. Shi, J. Lian, Y. Ma, P. Liu
First Affiliated HosFirst Affiliated Hospital of Harbin Medical University, Harbin, China
Impact: This study presents biocompatible nanoplatforms
that allow MR imaging, high anti-tumor thermoradiotherapy
efficacy, and negligible side effects in the treatment of
GBM.
|
| 08:23 |
 |
Screen Number: 5
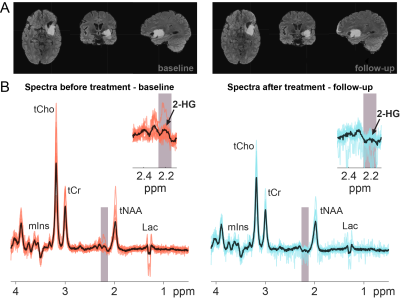
0070. Ivosidenib
and Vorasidenib decrease 2-hydroxyglutarate levels in low-grade
glioma: an in-vivo MR Spectroscopy study

D. Simicic, S. Alcicek, L. Blair, M. Saint-Germain, H.
Zöllner, C. Davies-Jenkins, M. Holdhoff, J. Laterra, C.
Bettagowda, K. Schreck, D. Lin, P. Barker, D. Kamson, G.
Oeltzschner
The Johns Hopkins University School of Medicine, Baltimore, United States
Impact: This is the first in-vivo evidence using MRS
that ivosidenib/vorasidenib reduces 2-HG suggesting that
in-vivo 2-HG estimates could serve as sensitive biomarkers
for monitoring low-grade gliomas in vivo in response to
small-molecule IDH inhibitor therapy after initiation of
treatment.
|
| 08:25 |
 |
Screen Number: 6
0071. Unsupervised
Learning to Dissect the Metabolic Heterogeneity in mutant IDH
Astrocytoma and Oligodendroglioma Using 3D MRSI
G. Ungan, P. Weiser, J. Dietrich, D. Cahill, O. Andronesi
Athinoula A. Martinos Center for Biomedical Imaging, Department of Radiology, Massachusetts General Hospital, Harvard Medical School, Boston, United States
Impact: This study demonstrates that metabolic imaging
combined with unsupervised machine learning effectively
differentiates astrocytomas and oligodendrogliomas. Insights
into tumor heterogeneity and spatial complexity advance
glioma classification and could guide more personalized,
subtype-specific treatment strategies in neuro-oncology.
|
| 08:27 |
 |
Screen Number: 7
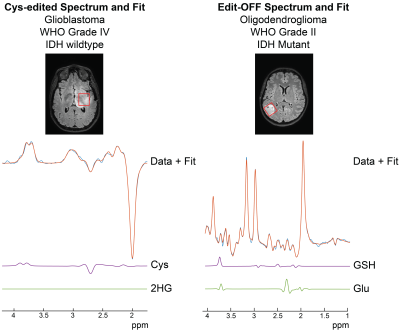
0072. In
vivo proton MR spectroscopy reveals alterations in cysteine
metabolism in human gliomas
K. Chan, E. Noch, E. Maher, T. Patel, A. Henning
The University of Texas Southwestern, Dallas, United States
Impact: The measurement of dysregulated cysteine
metabolism by 1H-MRS could provide a non-invasive biomarker
for monitoring treatments that target this pathway,
including cysteine depletion. High levels of cystathionine
in the absence of 2HG could be a marker of IDH-wildtype
glioblastoma.
|
| 08:29 |
 |
Screen Number: 8
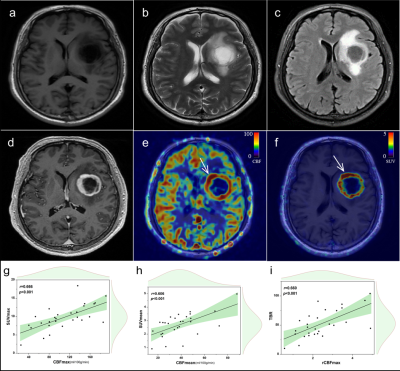
0073. Region-wise
Comparison of DCE-MRI based Pharmacokinetic Model Fitting in
Glioblastoma
S. Bera, S. Basak, S. Misra, G. W Kostrzanowska, A. Rajan,
S. Chawla, H. Poptani, S. Bhaduri
TCG Centres for Research and Education in Science and Technology (TCG CREST), KOLKATA, India
Impact: This study improves GBM assessment by optimizing
DCE-MRI PK model selection. It tailors models to specific
tumor regions, enabling more accurate quantification of
tumor characteristics, aiding diagnosis & treatment
planning. This approach can be applied to other tumors and
imaging protocols.
|
| 08:31 |
 |
Screen Number: 9
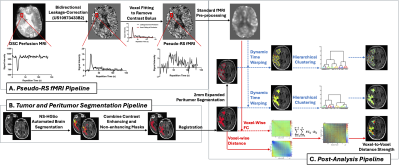
0074. Characterizing
Intra- and Peritumoral Connectivity in Human Gliomas using
Pseudo-Resting State Functional MRI Derived from DSC Perfusion
MRI
C. Wang, N. Cho, J. Yao, R. Everson, K. Patel, L. Liau, P.
Nghiemphu, N. Salamon, A. Lai, T. Cloughesy, B. Ellingson
University of California, Los Angeles, United States
Impact: “Pseudo” rs-fMRI derived from clinical DSC
perfusion MRI may be useful for monitoring brain tumor
patients. Tumor infiltration and heterogeneity associated
with different glioma molecular subtypes can be revealed by
connectivity patterns within the tumor and with adjacent,
normal-appearing tissue.
|
| 08:33 |
 |
Screen Number: 10
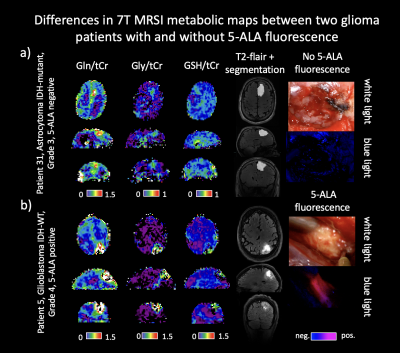
0075. 7T
MRSI ratios can predict the presence of 5-ALA fluorescence in
gliomas comparable to T1w-CE and PET
S. Huskic, P. Lazen, C. Cadrien, N. Weilguny, T.
Roetzer-Pejrimovsky, J. Furtner, J. Leitner, A.
Kloss-Brandstaetter, M. Preusser, T. Traub-Weidinger, K.
Roessler, S. Trattnig, G. Grabner, W. Bogner, G. Widhalm, G.
Hangel
Medical University of Vienna, Vienna, Austria
Impact: Our results show that 7T MRSI is a powerful tool
for predicting 5-ALA fluorescence in gliomas and can be
useful in therapy planning. It would be valuable to
investigate the spatial correlation between 7T MRSI and
areas of 5-ALA fluorescence.
|
| 08:35 |
 |
Screen Number: 11
0076. Similarity
of biological information captured by 68Ga-PSMA-11 PET and
arterial spin labeling perfusion imaging in glioblastoma
Y. Han, W. Hu, Y. Luo, X. Cao, Y. Sun, J. Zhang
Lanzhou University Second Hospital, Lanzhou, China
Impact: These findings may be valuable for further
revealing the potential mechanisms underlying PSMA tracer
uptake, and also provide support for PSMA-targeted
radiotherapy as a viable treatment option for patients with
glioblastoma.
|
| 08:37 |
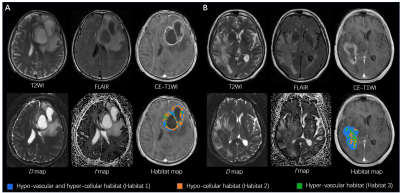 |
Screen Number: 12
0077. Preoperative
Habitat Imaging of Intratumor Heterogeneity Using Intravoxel
Incoherent Motion MRI Predicts Survival of High-Grade Gliomas
X. Wang, S. Suo, M. Cao, Y. Song, Y. Zhou
Renji Hospital, School of Medicine, Shanghai Jiao Tong University, Shanghai, China
Impact: Preoperative
perfusion and diffusion heterogeneity identified by habitat
analysis from IVIM-MRI were associated with the OS of HGG
patients. The specific tumor subregion with prognostic value
may help to refine the understanding of glioma ITH and
contribute to future treatments.
|
| 08:39 |
 |
Screen Number: 13
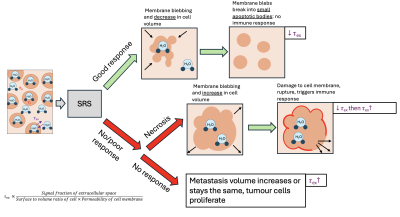
0078. Exchange
time from time-dependent diffusion-weighted MRI as a potential
biomarker for treatment response in human brain metastasis.
E. Gwyther, J. Powell, S. Iqbal, J. Golten, B. Jucker, M.
Jallais, D. Jones, C. Tax, M. Palombo
Cardiff University, Cardiff, United Kingdom
Impact: We provide evidence that estimates of exchange
time in brain metastases using diffusion time dependent
kurtosis is a potential biomarker to characterize treatment
response using endogenous water contrast.
|
| 08:41 |
 |
Screen Number: 14
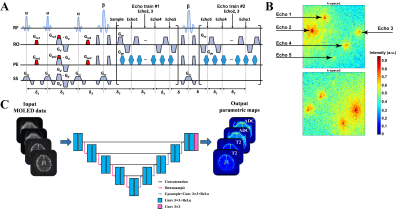
0079. Simultaneous
T2 and ADC Mapping via MQMOLED MRI for Brain Tumor
Differentiation
J. Bao, Z. Li, Q. Yang, X. Wang, Y. Zhuang, Y. Dong, L. Lin,
A. Tulupov, Y. Zhang, S. Cai, Z. Chen, C. Cai, J. Cheng
Department of Magnetic Resonance Imaging, The First Affiliated Hospital of Zhengzhou University, Zhengzhou University, zhengzhou, China
Impact: The MQMOLED's rapid, reliable tumor
differentiation capability could transform preoperative
diagnostics, enabling tailored treatment approaches and
potentially improving patient outcomes by precisely
identifying tumor types, thus guiding more effective
therapeutic interventions.
|
| 08:43 |
Screen Number: 15
0080. WITHDRAWN |
|
| 08:45 |
 |
Screen Number: 16
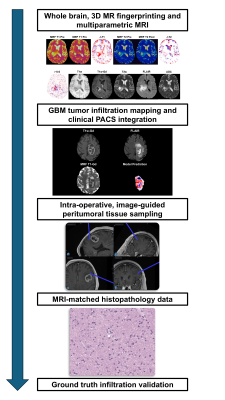
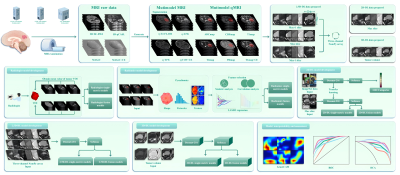
0081. Pre-Surgical
Detection of Infiltrating Glioblastoma Using a
Histopathology-Validated MR Fingerprinting Prediction Model
W. Zhao, T. Hodges, S. Gongala, P. Arjmand, X. Wang, S.
Deng, C. Tippareddy, N. Korakavi, E. Alzaga Goni, R. Adams,
R. Ghotra, P. Vempati, C. Davatzikos, M. Couce, J. Sunshine,
M. Staudt, A. Sloan, C. Badve, D. Ma
Case Western Reserve University, Cleveland, United States
Impact: Glioblastoma (GBM) peritumoral infiltration
leads to inevitable recurrence and death. We develop and
histopathologically-validate an MRF artificial intelligence
(AI) model for pre-surgical prediction of infiltrating GBM
to reduce tumor recurrence, improve patient quality of life,
and extend survival.
|
| 08:47 |
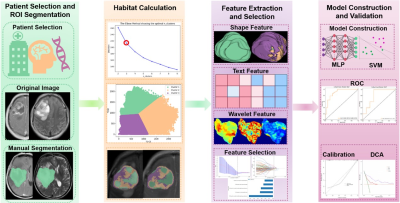 |
Screen Number: 17
0082. Presurgical
Tumor and Habitat MRI-based Radiomics Features for Predicting
Post-Surgical Recurrence of Glioma
Q. Ouyang, P. Liu, G. Jiang
The Affiliated Guangdong Second Provincial General Hospital of Jinan University, Guangzhou, China
Impact: The presurgical habitat-based radiomics model
may facilitate clinicians in deciding whether to undergo the
surgical resection of glioma, thus giving a patient-tailored
decision.
|
| 08:49 |
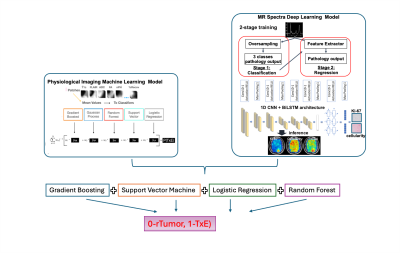 |
Screen Number: 18
0083. Integrating
AI-based models from physiologic MRI with MR spectra for
differentiating treatment-effect from glioma tumor recurrence
I. F. S. Ngnie Kamga, J. Ellison, N. Tran, J. Philips, A.
Molinaro, Y. Li, T. Luks, A. Shai, D. Nair, J.
Villanueva-Meyer, M. Berger, S. Hervey-Jumper, M. Aghi, S.
Chang, J. Lupo
UCSF, San Francisco, United States
Impact: Our integrated framework improves
differentiation of TxE from rTumor, reducing misdiagnosis
risk and guiding treatment decisions. Future work could
explore personalized treatment strategies based on imaging
biomarkers, improving patient outcomes. Researchers gain
avenues to optimize multi-modal ML approaches in
neuro-oncology.
|
| 08:51 |
 |
Screen Number: 19
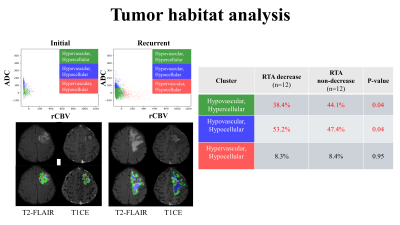
0084. Multiparametric
MRI Predicts Longitudinal Changes in Telomerase Activity in
Recurrent IDH-Wildtype Glioblastoma
K. S. Choi, S. Y. Jeong, S. H. Choi, C-K Park, I. Hwang
Seoul National University Hospital, Seoul, Korea, Republic of
Impact: Tumor habitat analysis using multiparametric MRI
for noninvasive telomerase activity prediction could inform
telomerase-targeted clinical trials in glioblastoma
treatment.
|
| 08:53 |
 |
Screen Number: 20
0085. Physio-Metabolic
MRI–derived tumor microenvironment mapping for differentiating
glioblastomas from large brain metastases
P. Liu, Q. Ouyang, R. Yang, G. Jiang
The Affiliated Guangdong Second Provincial General Hospital of Jinan University, Guangzhou, China
Impact: The physio-metabolic MRI-derived biomarkers of
oxygen metabolism and neovascularization offer valuable
insights into the heterogeneity of TME, enabling more
precise and personalized identification of solitary brain
tumors. This approach paves the way for developing novel,
tailored therapeutic strategies forthose patients.
|
| 08:55 |
 |
Screen Number: 21
0086. Optimizing
Glioma Classification: Comparative Analysis of Radiologist,
Radiomics and Multi-dimensional Deep Learning Using Quantitative
MRI
X. Ge, Y. Xiong, J. Zhang
Second Clinical School, Lanzhou University, Lanzhou, China
Impact: This study could significantly enhance glioma
diagnostics by employing advanced quantitative MRI alongside
DL models, such as 2.5D-DL fusion model, which demonstrates
superior classification accuracy. This approach enables
personalized treatment strategies based on molecular
insights, previously unattainable with traditional methods.
|
| 08:57 |
 |
Screen Number: 22
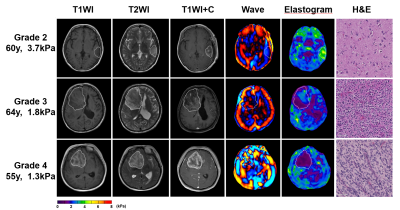
0087. Biomechanical
Study of Adult-type Diffuse Glioma: Insights from MR
Elastography on Tumor Molecular Mutations, Blood Supply and
Prognosis
Y. Zeng, S-j Bai, M. Zhou, W. Cheng, H. Guan, Y. Shi
Shengjing Hospital of China Medical University, Shenyang, Liaoning Province, China
Impact: This study demonstrates that MR
elastography-derived tumor stiffness is a valuable
noninvasive biomarker for glioma grading, molecular mutation
prediction, and prognosis assessment, potentially enhancing
early diagnosis, surgical planning, and personalized
treatment strategies for glioma patients.
|
| 08:59 |
Screen Number: 23
0088. WITHDRAWN |
|
| 09:01 |
 |
Screen Number: 24
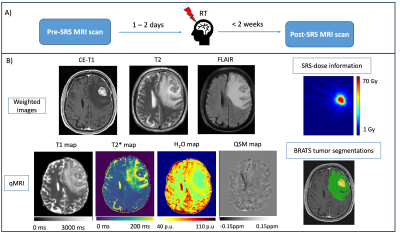
0089. Stereotactic
radiosurgery-induced changes in brain metastasis patients within
two weeks after therapy detected using multi-parametric qMRI
D. Thomas, S. Klinsing, M. Ghazouani, A-L Luger, R. Wolff,
M. Czabanka, J. Steinbach, U. Pilatus, E. Hattingen, P.
Zeiner, K. Wenger
Goethe University Frankfurt, University Hospital Frankfurt, Institute of Neuroradiology, Frankfurt am Main, Germany
Impact: Results demonstrate that qualitative and
quantitative (qMRI) changes are detectable in MR scans of BM
patients even within two weeks after SRS. The effects of SRS
are not dose dependent and may have predictive value for
treatment outcome.
|
| 09:03 |
 |
Screen Number: 25
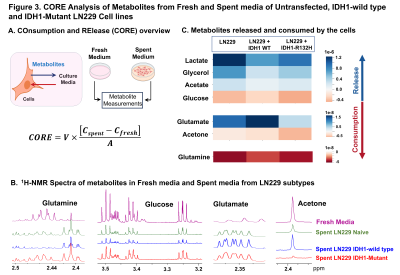
0090. IDH-Mutant
Gliomas Reprogram Glutamine Metabolism and Pyruvate Utilization:
1H NMR Spectroscopy based Consumption and Release Investigations
V. Tiwari, N. Gupta, R. Chandak, A. Panigrahi
Indian Institute of Science Education and Research Berhampur, Berhampur, India
Impact: 1H-NMR-based
investigations and transcriptomic-profiling suggests that
IDH-mutant gliomas undergo unique metabolic-adaptations,
showing increased glutamine-glutamate dependency, disrupted
pyruvate pathways, enhanced release of lactate. These
findings indicate Glutamine-addiction in IDH-mutant-gliomas,
pointing towards potential therapeutics targeted at
glutamine metabolism for management of IDH-mutant-gliomas.
|
The International Society for Magnetic Resonance in Medicine is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians.