Traditional Poster
Parkinson’s Disease: Imaging, Biomarkers, & Beyond
ISMRM & ISMRT Annual Meeting & Exhibition • 10-15 May 2025 • Honolulu, Hawai'i

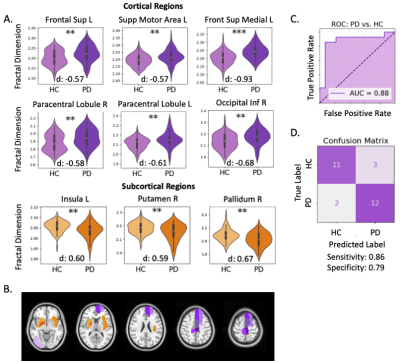 |
4894. Cortical
Boundary Complexity on Structural MRI Distinguishes Parkinson’s
Disease from Healthy Controls and Correlates with Symptom
Severity
D. Schoen, S. Deutsch, J. Mehta, S. Wang, I. Bledsoe, J.
Ostrem, P. Starr, D. Wang, M. Morrison
UCSF, San Francisco, United States
Impact: This study confirms regional fractal dimension
(FD)—a measure of sub-(cortical) boundary complexity—as a
biomarker of Parkinson’s disease diagnosis and severity. FD
could be used to improve clinical decision-making including
patient-specific treatment planning.
|
|
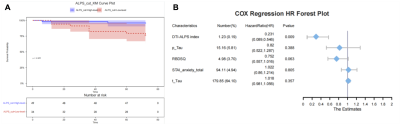 |
4895. Neuroimaging-Based
Glymphatic Function Predicts Conversion from Prodromal to
Manifest Parkinson's Disease
A. Chen, Y. Xu, X. Wei
Guangzhou First People's Hospital Affiliated to Guangzhou Medical University,the Second Affiliated Hospital of South China University of Technology, Guangzhou, China
Impact: The DTI-ALPS index indicates glymphatic
dysfunction in pPD and predicts conversion to PD, aiding
early risk assessment and intervention.
|
|
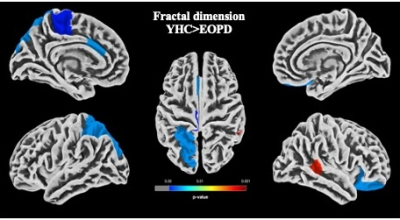 |
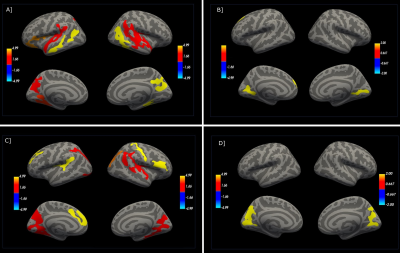
4896. A
comparative study of volume and surface changes in early onset
Parkinson’s Disease compared to age related controls
S. Kumari, S. Arora, S. Chaudhary, P. Bhat, A. Jaiswal, R.
Rajan, S. S. Kumaran, L. Devarajan, A. Srivastava
All India Institute of Medical Sciences, New Delhi, India
Impact: Distinct patterns of brain atrophy and cortical
alterations in EOPD, suggest disruption of folding
architecture of the cortex in patients with PD and reduced
cortical complexity with LEDD, and could guide more accurate
monitoring of treatments.
|
|
 |
4897. Brain
age gap estimated from MRI based deep learning model was
associated with cognitive impairment in Parkinson’s disease
W. Xie, J. Dai, F. Zhou
The First Affiliated Hospital, Jiangxi Medical College, Nanchang University, Nanchang, China
Impact: BAG can be used to objectively estimate
cognitive impairment in PD patients. The application of deep
learning model to accurately and robustly predict brain age
would be helpful for the management of PD patients.
|
|
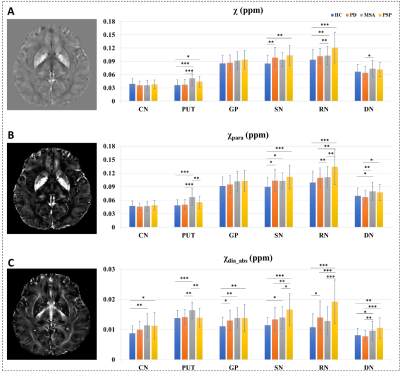 |
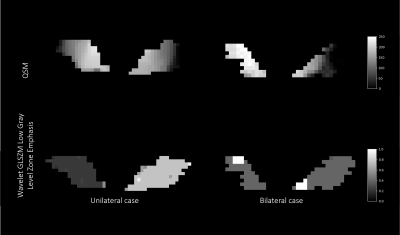
4898. Susceptibility
separation technique for assessing differences in the deep gray
matter nuclei among parkinsonian disorders
G. Li, H. Zhou, C. Xu, H. Zhong, W. Chen, G. Wang, J. Li
East China Normal University, Shanghai, China
Impact: The susceptibility separation method on QSM
images delivers valuable and comprehensive insights into the
iron deposition and myelin density among PD, MSA, and PSP.
This may expand our understanding of susceptibility
alternation in parkinsonian disorders.
|
|
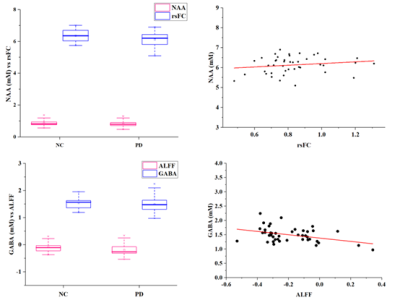 |
4899. Altered
Functional Connectivity and Metabolism of the Anterior Cingulate
Cortex in Parkinson’s Disease
W. Su, Q. Cheng, J. Xin, Y. Gao, Q. Zhang, X. Li, S. Zhao,
F. Xue, K. Zhang
School of Psychology, Shandong Normal University, Jinan, China
Impact: Integrating rs-fMRI and MRS in PD research could
uncover the bidirectional relationship between functional
connectivity and metabolism, enhancing our understanding of
future brain dynamics changes.
|
|
 |
4900. Morphometric
Brain Changes in Young-Onset and Late-Onset Parkinson’s Disease:
A Comparative Study
S. S. Kumaran, P. Bhat, P. ., S. Kumari, S. Arora, V. Goyal,
A. K. Srivastava, R. Rajan, D. Radhakrishnan
All India Institute of Medical Science, New Delhi, India
Impact: Deformation-morphometric analyses identified
unique structural brain changes in PD and YoPD, especially
critical subcortical alterations. Duration and onset
specific atrophy in the view of clinical similarity,
reinforces the utility of DBM as a sensitive method for
capturing PD-associated neurodegeneration.
|
|
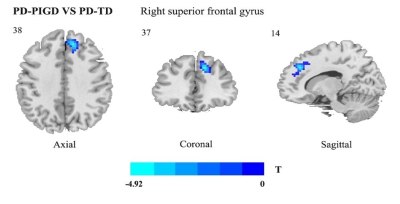 |
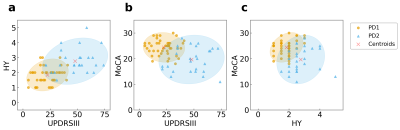
4901. Changes
to voxel-wise spontaneous activity and linked brain functional
networks in PD patients with distinct motor subtypes.
M. Guo, Y. Jiang, G. Fan
The First Affiliated Hospital of China Medical University., Shenyang, China
Impact: These findings suggest that PD-PIGD represents a
more severe PD subtype, offering new insights into clinical
differences between PD motor subtypes.
|
|
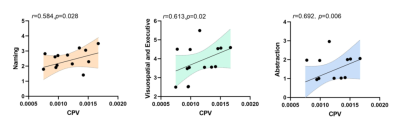 |
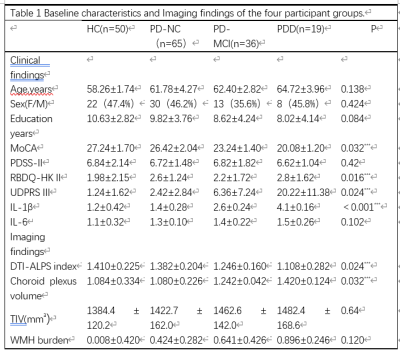
4902. Relationship
Among ALPS, Choroid Plexus Volume and Cognitive Subdomains in
Parkinson’s Disease
H. Li, X. ZHAO, Y. Liu, Z. Wang, J. ZHANG, K. AI
Department of Magnetic Resonance, the Second Hospital of Lanzhou University, Lanzhou, China, LANZHOU, China
Impact: The correlation between CPV and the cognitive
functions of visuospatial executive ability, naming, and
abstraction provides a more granular perspective to
understand the relationship between changes in various
cognitive domains of PD patients and the glymphatic system.
|
|
 |
4903. Glymphatic
System Impairment in Different Stages of Parkinson's Disease:
Evidence from DTI-ALPS Imaging
C. Lai, S. Zhou, Z. Zhen, Z. Zuo, W. Chen
Institute of Biophysics, Chinese Academy of Sciences, Beijing, China
Impact: Alps-index changes intensify in advanced PD
stages, indicating potential as a progression marker. This
emphasizes the need for longitudinal studies to validate it
as a tool for monitoring PD progression and assessing
therapeutic interventions.
|
|
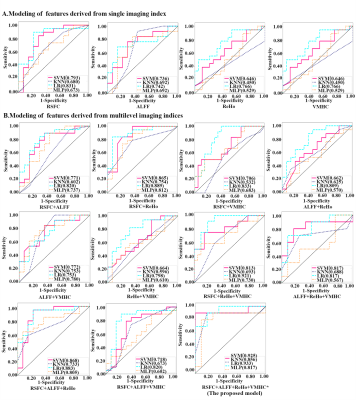 |
4904. Machine
learning approach effectively discriminates PD from progressive
supranuclear palsy: multi-level indices of rs-fMRI
W. Cheng, J. Dai, F. Zhou
Nanchang University, Nanchang, China
Impact: PD and PSP have similar clinical syndrome but
were treated differently. Our finding suggested LR and SVM
based on multi-level indices of rs-fMRI can effectively
differentiate PD from PSP. It would help the treatment
selection for PD and PSP patients.
|
|
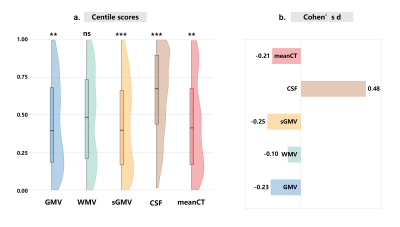 |
4905. Normative
Modeling of Brain Structure Deviations in Parkinson’s Disease
Patients without Dementia
L. Chai, Z. Zhuo, Y. Duan, Y-s Wang, J. Weng, T. Hua, Y. Liu
Beijing Tiantan Hospital, Capital Medical University, Beijing, China
Impact: PD patients without dementia exhibit
heterogeneous cortical changes, with nearly half showing
negative deviations. Global alterations include reduced gray
matter, increased cerebrospinal fluid (CSF), and stable
white matter volume (WMV). Thinner cortical thickness
correlates with more severe gait freezing.
|
|
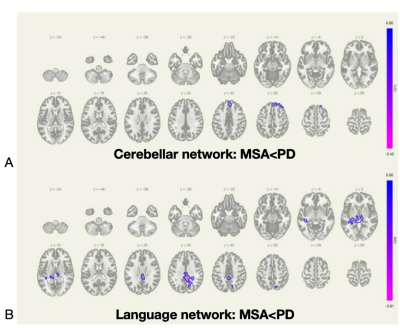 |
4906. Iron
deposition is associated with motor and non-motor network
breakdown in Parkinsonism
y. zhang, f. leng, y. gao, J. Lian, j. qiu
Peking University First Hospital, Beijing, China
Impact: This study is one of the first to report the
association between iron deposition and network dysfunction
in Parkinsonian disorders. The findings placed emphasis on
language network disruption in movement disorders, which may
serve as initial clue for further investigations.
|
|
|
4907. GABAergic
Imbalance in REM sleep behavior disorder in patients with
Parkinson’s disease
Y. Zhang, N. He, P. Wu, J. Weng, Q. Yu, F. Yan
Ruijin Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, China, Shanghai, China
Impact: GABA+ level imbalance in PD patients with and
without RBD might bring forward new layered diagnoses or
therapeutic options.
|
||
| 4908. WITHDRAWN | ||
 |
4909. The
relationship between sleep disorder,neuroinflammation,glymphatic
dysfunction, and cognition: a study based on Parkinson’s disease
continuum participants
维. 张, 祺. 田
重庆, 重庆, China
Impact: Our study provided evidence that both sleep
disorder and neuroinflammation were associated with
glymphatic dysfunction, which is further related to
cognitive impairment. These results may provide a
theoretical basis for new targets for treating PD.
|
|
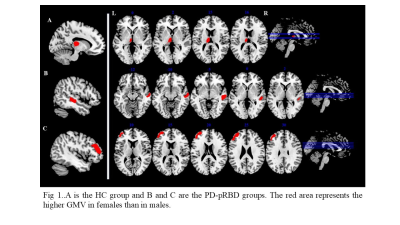 |
4910. Sex-Specific
Brain Morphological and Network Differences in Parkinson's
Disease Parkinson’s with Rapid Eye Movement Sleep Behavior
Disorder
Y. Liu, L. Zhou, J. Zhang
The Second Hospital of Lanzhou University, lanzhou, China
Impact: By examining the distinct stages of disease
progression in PD patients alongside sex-specific
differences, this research aims to identify resultant
variations as potential targets for non-pharmacological
interventions, such as transcranial magnetic stimulation
(TMS), to support individualized treatment strategies.
|
|
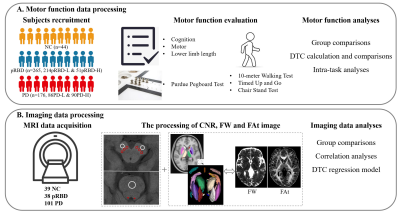 |
4911. The
clinical manifestation and preliminary mechanism exploration of
cognitive-motor interference in Parkinson's disease
J. Wu, J. Chen, M. Zhang
The Second Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou, China
Impact: Education provokes a positive effect for PD
motor during early parkinsonian period. The cognitive-motor
interference in PD was modulated by not only dopaminergic
nigra, but cerebellar lobule and basal forebrain, which
further found to be differed under different disease
conditions.
|
|
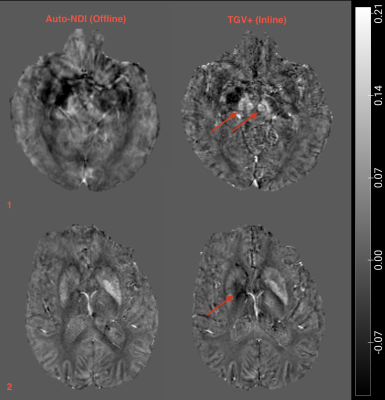 |
4912. QSM
in Patients with Movement Disorders: Neuroradiological
Evaluation of Offline and Inline Pipelines for Clinical Use
M. Elgwely, P. Sha, A. Papadaki, S. Wastling, J. Pfeuffer,
I. Dragonu, C. Triantafyllou, O. Kiersnowski, K. Shmueli, J.
Thornton, A. K. Yamamoto, D. Thomas, T. Yousry
Lysholm Department of Neuroradiology, National Hospital for Neurology and Neurosurgery, London, United Kingdom
Impact: Clinically robust QSM can be achieved using
multi-echo 3D-GRE sequence within a clinically acceptable
scan time using offline and inline pipelines. This confirms
the feasibility of using inline QSM for potential routine
clinical neuroradiological evaluation of patients with
movement disorders.
|
|
 |
4913. Lateral
Deep Brain Stimulation Prediction using Quantitative
Susceptibility Mapping (QSM) and Unsupervised Gaussian Mixture
Models
A. Roberts, S. Akkus, D. Romano, P. Spincemaille, B. Kopell,
Y. Wang
Cornell University, New York, United States
Impact: Preoperative QSM as a potential predictive tool
for deep brain stimulation candidate selection is
introduced. Findings suggest that imaging features
complement clinical assessment in surgical planning. Future
studies should examine additional targets to validate this
approach.
|
The International Society for Magnetic Resonance in Medicine is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians.