Digital Poster
Pulmonary Imaging II: Applications
Joint Annual Meeting ISMRM-ESMRMB & ISMRT 31st Annual Meeting • 07-12 May 2022 • London, UK

| Computer # | ||||
|---|---|---|---|---|
1474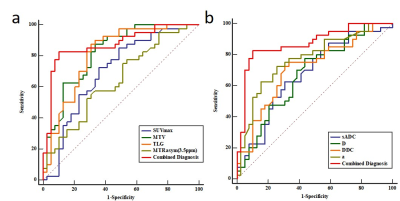 |
24 | Multi-parametric 18-FDG PET/MRI in predicting lung cancer lymphatic metastasis
Fangfang Fu1, Meng Nan2, Yaping Wu1, Zhun Huang3, Yan Bai1, Pengyang Feng3, Ting Fang2, Jianmin Yuan4, Yang Yang5, Haiyan Gao1, and Meiyun Wang1
1Henan Provincial People's Hospital & People's Hospital of Zhengzhou University, Zhengzhou, China, 2Zhengzhou University People's Hospital & Henan Provincial People’s Hospital, Zhengzhou, China, 3Henan University People's Hospital & Henan Provincial People’s Hospital, Zhengzhou, China, 4Central Research Institute, Beijing, China, 5Beijing United Imaging Research Institute of Intelligent Imaging, Beijing, China It is meaningful to predict lymph node status of lung cancer before surgery. In the study, 18F-FDG PET/MRI were used to obtain PET metabolic parameters, multi-model DWI and APTWI parameters for predicting LNM of lung cancer. Our results showed that multiparametric PET/MRI is helpful in predicting lymph node status before surgery. 18F-FDG hybrid PET/MRI enables a robust diagnosis ability of LNM of lung cancer when several multi-model DWI parameters, PET metabolic parameters and APT parameter are combined. Thus, integrated PET/MRI can help to characterize LNM before surgery. |
||
1475 |
25 | TNM and VALSG Stage Assessments in SCLC: Diagnostic Capability Comparison among PET/MRI, PET/CT, Whole-Body MRI and Conventional Examination Video Permission Withheld
Yoshiharu Ohno1,2, Masao Yui3, Kaori Yamamoto3, Daisuke Takenaka4, Takeshi Yoshikawa4, Saki Takeda5, Akiyoshi Iwase5, Yuka Oshima1, Nayu Hamabuchi1, Satomu Hanamatsu1, Yuki Obama1, Hiroyuki Nagata1, Takahiro Ueda1, Hirotaka Ikeda1, Kazuhiro Murayama2, and Hiroshi Toyama1
1Radiology, Fujita Health University School of Medicine, Toyoake, Japan, 2Joint Research Laboratory of Advanced Medical Imaging, Fujita Health University School of Medicine, Toyoake, Japan, 3Canon Medical Systems Corporation, Otawara, Japan, 4Diagnostic Radiology, Hyogo Cancer Center, Akashi, Japan, 5Radiology, Fujita Health University Hospital, Toyoake, Japan
Whole-body MRI and co-registered or integrated PET combined with MRI (PET/MRI) using 1.5 T or 3T MR systems has been suggested as equal to or more accurate than PET/CT or conventional staging or recurrence surveillance methods in thoracic oncologic patients. We hypothesize that whole-body MRI and co-registered PET/MRI for SCLC patients have equal to or superior potential for VALSG and TNM stage assessments than PET/CT and conventional staging method. The purpose of this study was to prospectively compare the capabilities for assessing VALSG and TNM stages among whole-body MRI, PET/MRI, PET/CT and conventional staging method in SCLC patients.
|
||
1476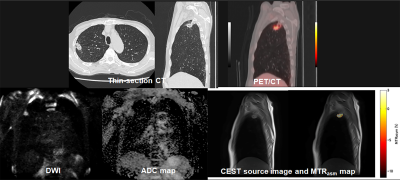 |
26 | CEST Imaging vs. DWI vs. FDG-PET/CT: Therapeutic Effect Prediction for Chemoradiotherapy in Non-Small Cell Lung Cancer Patients Video Permission Withheld
Yoshiharu Ohno1,2, Masao Yui3, Daisuke Takenaka4, Takeshi Yoshikawa4, Kaori Yamamoto3, Masato Ikedo3, Saki Takeda5, Akiyoshi Iwase5, Satomu Hanamatsu1, Yuki Obama1, Hiroyuki Nagata1, Takahiro Ueda1, Hirotaka Ikeda1, Kazuhiro Murayama2, and Hiroshi Toyama1
1Radiology, Fujita Health University School of Medicine, Toyoake, Japan, 2Joint Research Laboratory of Advanced Medical Imaging, Fujita Health University School of Medicine, Toyoake, Japan, 3Canon Medical Systems Corporation, Otawara, Japan, 4Diagnostic Radiology, Hyogo Cancer Center, Akashi, Japan, 5Radiology, Fujita Health University Hospital, Toyoake, Japan
We hypothesize that CEST imaging has a potential for therapeutic effect prediction in NSCLC patients treated with chemoradiotherapy and may be at least as valuable as DWI and FDG-PET/CT. Moreover, combined predictors may improve therapeutic effect prediction capability, when compared with single predictor from MRI or PET/CT. The purpose of this study was to compare the capability of therapeutic effect prediction for chemoradiotherapy among CEST imaging, DWI, FDG-PET/CT and combined predictors from MRI and PET/CT in NSCLC patients.
|
||
1477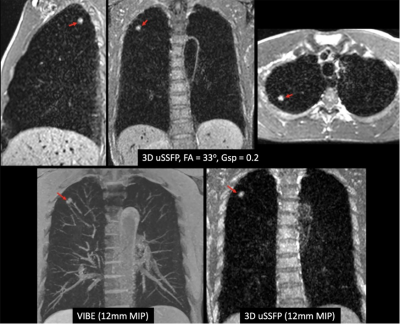 |
27 | Dark Blood, Susceptibility-Insensitive 3D Unbalanced Steady-State Free Precession: A Potential New Approach for Lung Cancer Screening
Robert R Edelman1,2, Bradley Allen2, Nondas Leloudas1, Jianing Pang3, and Ioannis Koktzoglou1,4
1Radiology, NorthShore University HealthSystem, Evanston, IL, United States, 2Radiology, Feinberg School of Medicine, Northwestern University, Chicago, IL, United States, 3Siemens Medical Solutions USA, Chicago, IL, United States, 4Radiology, Pritzker School of Medicine, University of Chicago, Chicago, IL, United States
We recently described the feasibility of using a prototype 3D unbalanced steady-state free precession (3D uSSFP) pulse sequence for dark blood imaging. We sought to determine whether this technique could be adapted for dark blood, susceptibility-insensitive imaging of the lungs. A breath-hold, ECG-gated version of 3D uSSFP was implemented for a pilot study of healthy volunteers and patients. Initial results suggest that 3D uSSFP allows efficient volumetric imaging of the lungs and can demonstrate even small lung nodules without artifacts. With further development, the technique could provide a radiation-free alternative to low-dose CT for lung cancer screening.
|
||
1478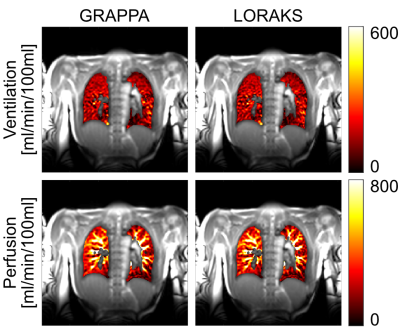 |
28 | Improving reconstruction quality in non-contrast-enhanced functional lung imaging via LORAKS
Efe Ilicak1, Safa Ozdemir1, Lothar R. Schad1, Jascha Zapp1, and Frank G. Zöllner1,2
1Computer Assisted Clinical Medicine, Heidelberg University, Mannheim, Germany, 2Mannheim Institute for Intelligent Systems in Medicine, Heidelberg University, Mannheim, Germany
Functional lung imaging is of great importance for diagnosis and follow-up of prevalent lung diseases. To this end, novel pulse sequences and post-processing techniques have been previously proposed to assess pulmonary functions. However, one overlooked aspect has been the parallel imaging reconstruction. Here, we propose the use of an advanced reconstruction scheme based on Low-Rank Modeling of Local k-Space Neighborhoods (LORAKS). In vivo results are provided to demonstrate the performance of LORAKS compared to commonly used GRAPPA reconstructions. Preliminary results indicate that LORAKS can be a viable option for improving reconstruction quality in pulmonary functional imaging.
|
||
1479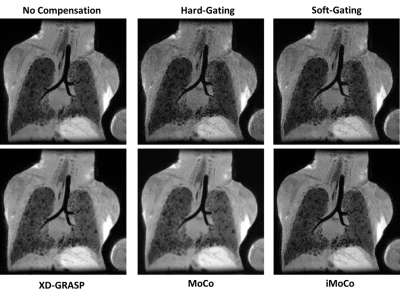 |
29 | Motion Compensation in Pulmonary Ultra-short Echo Time MRI: Preliminary Results in Neonatal Bronchopulmonary Dysplasia
Luis A. Torres1, Nara S. Higano2,3,4, Deep Gandhi4, Chamindu Gunatilaka2, Jason C. Woods2,3,4, and Sean B. Fain5
1Medical Physics, University of Wisconsin-Madison, Madison, WI, United States, 2Division of Pulmonary Medicine, Cincinnati Children’s Medical Center, Cincinnati, OH, United States, 3Department of Pediatrics, University of Cincinnati College of Medicine, Cincinnati, OH, United States, 4Department of Radiology, Cincinnati Children’s Medical Center, Cincinnati, OH, United States, 5Department of Radiology, University of Iowa, Iowa City, IA, United States
Self-gating of free breathing pulmonary MR images remains challenging due to inconsistent tidal breathing and bulk motion especially in neonatal patients. We evaluate several conventional and advanced retrospective motion compensation techniques in neonatal subjects with lung disease of prematurity. Registration-based techniques show a significant improvement in signal to noise ratio and contrast to noise ratio relative to other motion compensation methods. There were no significant changes in sharpness across the cohort. We conclude that registration-based techniques could be used to improve image quality without loss of sharpness.
|
||
1480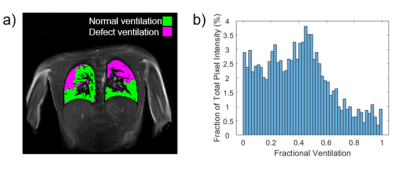 |
30 | Use of Phase Resolved Functional Lung Imaging (PREFUL) to Assess Response to Kaftrio® Therapy in Cystic Fibrosis
Zachary Peggs1, Jonathan Brooke2, Shahidehalsadat Safavi3,4, Andrew Prayle5,6, Christabella Ng5,6, Jan Alappadan1, Christopher Bradley1, Andrew Cooper1, Samal Munidasa7,8, Brandon Zanette8, Giles Santyr7,8, Helen Barr9, Alan R Smyth5,6, Ian Hall2, Susan Francis1, and Penny Gowland1
1Sir Peter Mansfield Imaging Centre, University of Nottingham, Nottingham, United Kingdom, 2The Nottingham Biomedical Research Centre (BRC), Respiratory Medicine Dept, School of Medicine, University of Nottingham, Nottingham, United Kingdom, 3The Toronto Lung Transplant Program, University Hospital Network, Toronto, ON, Canada, 4Respirology Medicine Dept, University of Toronto, Toronto, ON, Canada, 5School of Medicine, University of Nottingham, Nottingham, United Kingdom, 6Nottingham NIHR Biomedical Research Centre, Nottingham, United Kingdom, 7The Hospital for Sick Children, Toronto, ON, Canada; Dept. of Medical Biophysics, University of Toronto, Toronto, ON, Canada, 8The Hospital for Sick Children, Toronto, ON, Canada, University of Toronto, Toronto, ON, Canada, 9The Wolfson Centre for Adult Cystic Fibrosis, Nottingham City Hospital, Nottingham University Hospitals NHS Trust, Nottingham, United Kingdom
Phase resolved functional lung imaging (PREFUL) was carried out before and 12 weeks after commencement of Kaftrio® therapy in a small Cystic Fibrosis (CF) group, and in healthy controls (HC). No significant differences were found in measures characterising the PREFUL signal between HC and CF, or before and after Kaftrio® therapy. This could be explained by the small sample size or lack of age matching. It was found that fractional ventilation measures with PREFUL can be sensitive to subjective thresholding and the method of image registration. Also, the impact of irregular breathing patterns, especially in patients, should be further explored.
|
||
1481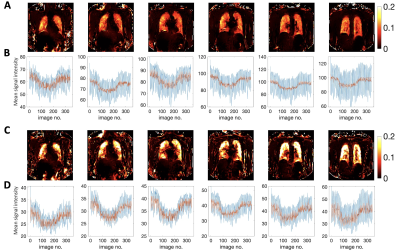 |
31 | Oxygen-enhanced MRI of the lung at 3 tesla: R2* contrast in smokers and non-smokers Video Permission Withheld
Mina Kim1, Josephine H. Naish2,3, Marta Tibiletti2, Sarah H. Needleman1, Adam Szmul1, David M. Higgins4, James P. B. O’Connor5,6, and Geoff J. M. Parker1,2
1Centre for Medical Image Computing (CMIC), University College London, London, United Kingdom, 2Bioxydyn Limited, Manchester, United Kingdom, 3BHF Manchester Centre for Heart and Lung Magnetic Resonance Research (MCMR), Manchester University NHS Foundation Trust, Manchester, United Kingdom, 4Philips, Farnborough, United Kingdom, 5Division of Cancer Sciences, University of Manchester, Manchester, United Kingdom, 6Division of Radiotherapy and Imaging, Institute of Cancer Research, London, United Kingdom T1-weighted dynamic lung OE-MRI is challenging at 3 T using gradient echo acquisitions due to decreased T1 relaxivity of oxygen and substantial ∆R2* contribution. We implemented a dual echo T1-FFE-based method at 3 T and evaluated signal enhancement behaviour and ∆R2*. The proposed method is shown to produce negative contrast on oxygen enhancement signal due to dominance of ∆R2* at TE larger than 0.4 ms. We also demonstrated that the contrast property of the percentage signal enhancement (PSE) is TE dependent. Longer TE enables differentiation on PSE values between non-smokers and smokers. |
||
1482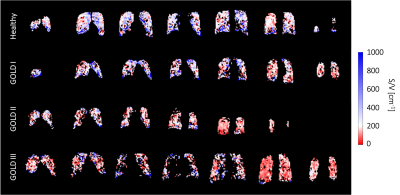 |
32 | Examining lung microstructure using 19F MR diffusion imaging in COPD patients
Arnd Jonathan Obert1,2, Marcel Gutberlet1,2, Agilo Luitger Kern1,2, Till Frederik Kaireit1,2, Julian Glandorf1,2, Tawfik Moher Alsady1,2, Frank Wacker1,2, Jens M. Hohlfeld2,3,4, and Jens Vogel-Claussen1,2
1Institute for Diagnostic and Interventional Radiology, Hannover Medical School, Hannover, Germany, 2Biomedical Research in Endstage and Obstructive Lung Disease Hannover (BREATH), German Center for Lung Research (DZL), Hannover, Germany, 3Department of Respiratory Medicine, Hannover Medical School, Hannover, Germany, 4Department of Clinical Airway Research, Fraunhofer Institute for Toxicology and Experimental Medicine, Hannover, Germany
Diffusion of fluorinated gas in the short-time regime was measured using multiple gradient echo sequences with a single pair of trapezoidal gradient pulses. Pulmonary alveolar surface-to-volume ratio (S/V) was calculated using a first-order approximation of the time-dependent diffusion in a study with 20 healthy volunteers and 22 patients with chronic obstructive pulmonary disease (COPD). Median surface-to-volume ratio is significantly decreased in COPD patients compared to healthy volunteers (P<.0001). No significant difference was found between measurements within 7 days. Linear correlations were found with S/V from hyperpolarized 129Xe MRI (r=0.85, P=.001) and the forced expiratory volume in one second (r=0.68, P<.0001).
|
||
1483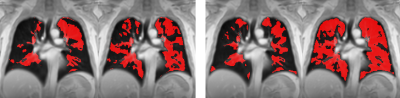 |
33 | PREFUL-MRI evaluation of dynamic hyperinflation induced by metronome-paced tachypnea in COPD patients
Robin A. Müller1,2, Filip Klimeš1,2, Andreas Voskrebenzev1,2, Lea Behrendt1,2, Till F. Kaireit1,2, Cristian Crisosto1,2, Maximilian Zubke1,2, Martin R. Prince3,4, Christopher C. Cooper5, R. Graham Barr6, Jens M. Hohlfeld7,8, and Jens Vogel-Claussen1,2
1Institute of Diagnostic and Interventional Radiology, Hannover Medical School, Hannover, Germany, 2Biomedical Research in Endstage and Obstructive Lung Disease Hannover (BREATH), German Center for Lung Research (DZL), Hannover, Germany, 3Department of Radiology, Weill Cornell Medical College, New York, NY, United States, 4Department of Radiology, Columbia College of Physicians and Surgeons, New York, NY, United States, 5Exercise Physiology Research Laboratory, Departments of Medicine and Physiology, David Geffen School of Medicine, UCLA, Los Angeles, CA, United States, 6Division of General Medicine, Department of Medicine, New York-Presbyterian/Columbia University Irving Medical Center, New York, NY, United States, 7Department of Respiratory Medicine, Hannover Medical School, Hannover, Germany, 8Fraunhofer Institute of Toxicology and Experimental Medicine, Hannover, Germany
Metronome-paced tachypnea (MPT) is a technique where a patient breathes with a fixed frequency (40 breaths / minute). MPT induces dynamic hyperinflation and allows investigation of potential stress-driven effects on ventilation parameters. Fourteen patients with chronic obstructive pulmonary disease (COPD) underwent phase-resolved functional lung (PREFUL) MRI with 2D coronal lung MR images acquired during normal tidal breathing (NTB) and MPT. Compared to NTB, ventilation defect percentages increased in COPD patients during MPT. Thus, MPT in conjunction with PREFUL-MRI will be further investigated as a possible sensible ventilation test for COPD patients.
|
||
1484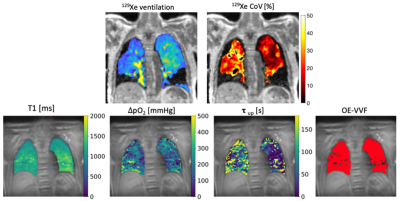 |
34 | Imaging biomarkers of ventilation in Interstitial Lung Disease from 129Xe and Oxygen Enhanced 1H MRI
Marta Tibiletti1, James A Eaden2, Jo Naish1,3, Paul JC Hughes2, John C Waterton1,4, Matthew J Heaton1, Nazia Chaudhuri5, Sarah Skeoch6, Ian N Bruce7,8, Stephen A Bianchi9, Jim M Wild2,10, and Geoff JM Parker1,11
1Bioxydyn Ltd, Manchester, United Kingdom, 2POLARIS, University of Sheffield MRI unit, The University of Sheffield, Sheffield, United Kingdom, 3MCMR, Manchester University NHS Foundation Trust, Manchester, United Kingdom, 4Centre for Imaging Sciences, University of Manchester, Manchester, United Kingdom, 5North West Lung Centre, Manchester University NHS Foundation Trust, Manchester, United Kingdom, 6Royal National Hospital for Rheumatic Diseases, Royal United Hospitals Bath NHS Foundation Trust, Bath, United Kingdom, 7NIHR Manchester Biomedical Research Centre, Manchester University NHS Foundation Trust, Manchester, United Kingdom, 8Centre for Musculoskeletal Research, University of Manchester, Manchester, United Kingdom, 9Academic Directorate of Respiratory Medicine, Sheffield Teaching Hospitals NHS Foundation Trust, Sheffield, United Kingdom, 10nsigneo Institute for in silico Medicine, Sheffield, United Kingdom, 11Centre for Medical Image Computing, Department of Medical Physics and Biomedical Engineering, University College London, London, United Kingdom
Interstitial lung diseases (ILD) are a heterogeneous group of conditions exhibiting inflammation and scarring of the lung parenchyma. Here, we compare imaging biomarkers from hyperpolarised 129Xe ventilation MRI and oxygen-enhanced MRI (OE-MRI) with standard pulmonary function tests in cohorts of ILD patients with mixed origins. We also evaluated whether disease resolution or progression could be detected over two visits. None of the imaging biomarkers considered completely differentiated ILD subtypes. OE-MRI biomarkers are feasible in ILD patients and do not correlate strongly with PFT. Both OE-MRI and 129Xe MRI revealed spatially heterogeneous ventilation in patients with DI-ILD and IPF.
|
||
1485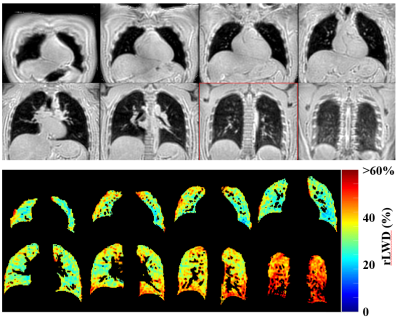 |
35 | Dynamic Changes in Lung Water Density and Volume with Changes in Body Position
David Thomas Goodhart1, Justin Grenier1, Rob Stobbe1, Peter Seres1, and Richard Thompson1
1The Department of Biomedical Engineering, University of Alberta, Edmonton, AB, Canada
We aim to describe the dynamic response of the distribution of lung water to the change in position from standing to supine. An efficient UTE MRI trajectory (Yarnball) provided 3D images (free-breathing, 74 seconds acquisition) in 3 volunteers, with 10 repeated scans over ~14 minutes. Lung water density (LWD) increased over time but total lung water content remained constant, consistent with a measured decrease in lung volume over time. LWD increased by a larger extent towards the back, suggesting a larger lung volume reduction in gravity dependent regions (the back) over time. Steady-state LWD was not achieved in 14 minutes.
|
||
The International Society for Magnetic Resonance in Medicine is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians.