Digital Poster
COVID-19: Latest MRI Findings & Applications
Joint Annual Meeting ISMRM-ESMRMB & ISMRT 31st Annual Meeting • 07-12 May 2022 • London, UK

| Computer # | ||||
|---|---|---|---|---|
2201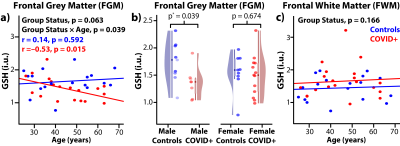 |
14 | Brain GABA and glutathione measurements in convalescent COVID-19 subjects Video Permission Withheld
Muhammad G. Saleh1, Linda Chang1,2,3, Huajun Liang1, Meghann C Ryan1, Eric Cunningham1, Eleanor Wilson4, Andrea R Levine5, Shyamasundaran Kottilil5, and Thomas Ernst1
1Department of Diagnostic Radiology and Nuclear Medicine, University of Maryland School of Medicine, Baltimore, MD, United States, 2Department of Neurology, University of Maryland School of Medicine, Baltimore, MD, United States, 3Department of Neurology, Johns Hopkins University School of Medicine, Baltimore, MD, United States, 4Institute of Human Virology, University of Maryland School of Medicine, Baltimore, MD, United States, 5Department of Medicine, University of Maryland School of Medicine, Baltimore, MD, United States
COVID-19 infection was associated with lower plasma levels of glutathione (GSH), provoking oxidative stress; however, whether GSH levels are also lower in the brain is unknown. COVID-19 survivors (COVID+) also have higher prevalence of psychiatric disorders, possibly due to altered brain GABA. However, brain GABA and GSH levels have not been assessed in convalescent COVID-19 (COVID+) individuals. Using edited MRS, frontal grey matter (FGM) GSH were lower in male COVID+, and COVID+ individuals had greater age-related decline in FGM GSH, compared to uninfected controls. These findings suggest that male COVID+ individuals, especially the older subjects, are susceptible to oxidative stress.
|
||
2202 |
15 | Global network disruption in focal to bilateral tonic-clonic seizures. Video Permission Withheld
Christina Maher1,2, Arkiev D'Souza1, Michael Barnett1,3,4, Omid Kavehei2,5, Armin Nikpour4, and Chenyu Wang1,3
1Brain and Mind Centre, The University of Sydney, Sydney, Australia, 2School of Biomedical Engineering, Faculty of Engineering, University of Sydney, Sydney, Australia, 3Sydney Neuroimaging and Analysis Centre, Sydney, Australia, 4Department of Neurology, Royal Prince Alfred Hospital, Sydney, Australia, 5ARC Centre for Innovative Bioengineering, The University of Sydney, Sydney, Australia
Focal to bilateral tonic-clonic seizures (FBTCS) are a feature of focal epilepsy, characterised by seizures that spread contralaterally to the origin of ictal discharge. Widespread global network disruption has been shown in patients with FBTCS compared to those with focal epilepsy. A structure-function relationship has been proposed, suggesting the role of the underlying subcortical structures in network alterations. Disease duration has been associated with whole-brain network disruption. Global network disruption may be a subtle marker in differentiating the likelihood of developing FBTCS, allowing treatment to be tailored.
|
||
2203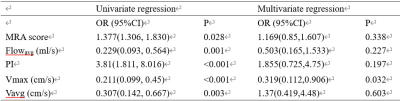 |
16 | Relationship between internal carotid artery hemodynamics and cerebrovascular events in moyamoya angiopathy based on 4D Flow MRI
Maoxue Wang1, Jilei Zhang2, and Bing Zhang3
1The Affiliated Drum Tower Hospital of Nanjing University Medical School, nanjing, China, 2Philips Healthcare, Shanghai, China, 3The Affiliated Drum Tower Hospital of Nanjing University Medical School, Nanjing, China
Little is known of distal internal carotid artery (ICA) hemodynamics in patients with moyamoya angiopathy (MMA) and its relationship with cerebrovascular events. In this study, distal ICA hemodynamics were analyzed using 4D Flow MRI in 70 MMA patients (61 infarct hemispheres and 63 non-infarct hemipheres). Vmax was found to be associated with cerebrovascular event in MMA patients.
|
||
2204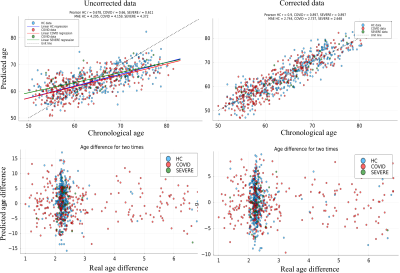 |
17 | Longitudinal brain imaging reveals brain white matter changes after COVID-19 in the UK Biobank
Ivan I. Maximov1,2, Dennis van der Meer2,3,4, Ann-Marie de Lange2,3,5, and Lars T Westlye2,3
1Western Norway University of Applied Sciences, Bergen, Norway, 2NORMENT, Oslo University Hospital, Oslo, Norway, 3University of Oslo, Oslo, Norway, 4Maastricht University, Maastricht, Netherlands, 5Lausanne University Hospital, Lausanne, Switzerland
The COVID-19 pandemic has caused a global health crisis. There are a few indications that this disease has harmful consequences on neurological functioning, besides brain changes following COVID-19 infection have not yet been fully understood. Here, we used UK Biobank (UKB) longitudinal diffusion MRI data acquired before and after COVID-19 tests along the ongoing UKB study. We evaluated brain age gap metrics for the participants with positive and negative test results in order to evaluate COVID-19 consequences on the brain.
|
||
2205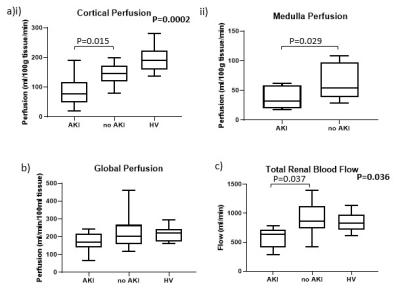 |
18 | Inflammation and reduced cortical perfusion assessed by renal MRI during acute kidney injury in critically ill COVID-19 patients
Eleanor F Cox1, Tomas Luther2, Per Eckerbom3, Jan Weis4, Fredrik Palm5, Robert Frithiof2, Per Liss3, and Susan T Francis1
1Sir Peter Mansfield Imaging Centre, University of Nottingham, Nottingham, United Kingdom, 2Section of Anesthesiology, Dept of Surgical Sciences, Uppsala University Hospital, Uppsala, Sweden, 3Section of Radiology, Dept of Surgical Sciences, Uppsala University Hospital, Uppsala, Sweden, 4Department of Medical Physics, Uppsala University Hospital, Uppsala, Sweden, 5Department of Medical Cell Biology, Uppsala University, Uppsala, Sweden Acute kidney injury (AKI) is associated with increased mortality in COVID-19 patients. Multiparametric MRI was performed to study renal perfusion, oxygenation and tissue structure in nineteen COVID-19 intensive care patients. Results are compared between patients with and without COVID-19 associated AKI, and with healthy volunteers (HV). Cortical perfusion was lower in COVID-19 compared to HVs (P=0.0002) with cortex and medullary perfusion lower in AKI compared to non-AKI (P<0.03). Correlations between cortex measures in COVID-19 showed T1 was positively correlated with T2 and ADC, and T2 was positively correlated with ADC and T2* suggesting interstitial oedema resulting from inflammation. |
||
2206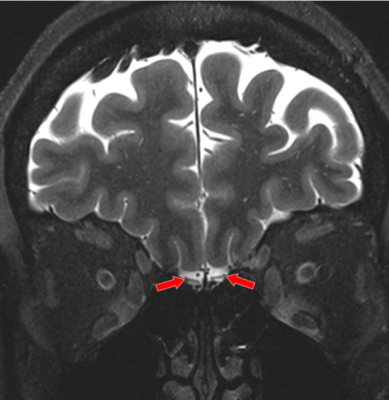 |
19 | Ultrahigh-Field 7T MRI of the Brain of COVID-19 Patients with Neurological Symptoms: An Initial Study
Shams Rashid1,2, Oleksandr Khegai1, Nathalie Jette3, Puneet Belani1, Puneet Pawha1, Sera Saju1, Allison Navis3, Brian Mathew3, Jonathan Goldstein3, Kapil Gururangan3, Qing Hao3, Anuradha Singh3, Jacqueline Becker4, Bradley Delman1, and Priti Balchandani1,2
1Diagnostic, Molecular and Interventional Radiology, Icahn School of Medicine at Mount Sinai, New York, NY, United States, 2BioMedical Engineering and Imaging Institute, Icahn School of Medicine at Mount Sinai, New York, NY, United States, 3Neurology, Icahn School of Medicine at Mount Sinai, New York, NY, United States, 4General Internal Medicine, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Since late 2019, COVID-19 has emerged as a global pandemic that has infected 200 million and killed 5 million. A significant proportion of COVID-19 patients continue to have persistent neurological sequelae after recovery, which are not well understood. In this study, we report our preliminary neuroradiological findings from ultrahigh field MRI at 7T in patients with post-COVID neurological symptoms. We show that numerous heterogeneous abnormalities are present in 7T MR brain images. We expect that these findings may pave the way to explain neurological symptoms in post-COVID patients.
|
||
2207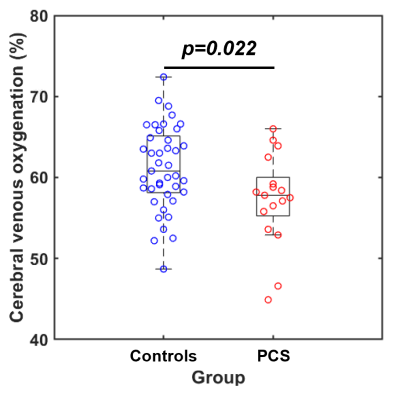 |
20 | Lower Cerebral Venous Oxygenation in Post-acute Sequelae of COVID-19
Peiying Liu1, Thomas Ernst1, Huajun Liang1, Dengrong Jiang2, Eric Cunningham1, Zixuan Lin2, Meghann C. Ryan1,3, Hanzhang Lu2, Eleanor Wilson4, Andrea Levine4, and Linda Chang1
1Department of Diagnostic Radiology & Nuclear Medicine, University of Maryland School of Medicine, Baltimore, MD, United States, 2Department of Radiology, Johns Hopkins University School of Medicine, Baltimore, MD, United States, 3Program in Neuroscience, University of Maryland School of Medicine, Baltimore, MD, United States, 4Department of Medicine, University of Maryland School of Medicine, Baltimore, MD, United States
Post-COVID Syndrome (PCS) is highly prevalent amongst COVID-19 survivors. Neuropsychiatric symptoms are often reported in patients with PCS, suggesting brain involvement in the early stages of COVID-19. One potential etiology is the cerebral microcirculation dysfunction due to SARS-CoV-2 infection, which may affect oxygen delivery and consumption in the brain. In the present study, we investigated the changes in cerebral venous oxygenation, which reflects the balance between oxygen supply and consumption, in convalescent COVID-19 participants with PCS. Our results showed that participants with PCS had altered venous oxygenation in their brain, which was also associated with slower locomotion.
|
||
2208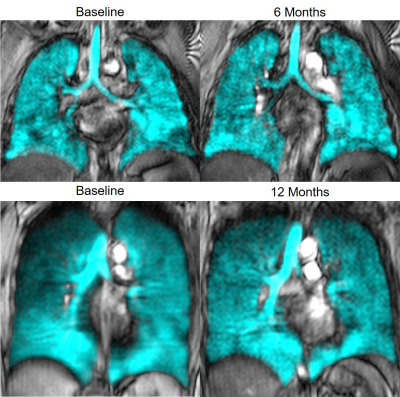 |
21 | Post-Acute COVID-19 Syndrome: Longitudinal 129Xe MRI Ventilation Heterogeneity Measurements
Harkiran K Kooner1,2, Marrissa J McIntosh1,2, Maksym Sharma1,2, Gaurav V Singh3, Neha Nasir3, Emily Blake3, Inderdeep Dhaliwal4, Michael Nicholson4, Miranda Kirby3, and Grace Parraga1,2,4
1Robarts Research Institute, London, ON, Canada, 2Department of Medical Biophysics, Western University, London, ON, Canada, 3Department of Physics, Ryerson University, Toronto, ON, Canada, 4Division of Respirology, Department of Medicine, Western University, London, ON, Canada
Post-acute COVID-19 syndrome (PACS) is an umbrella term for the long-term symptoms and poor quality-of-life that follow acute SARS-CoV-2 viral-infection in up to 7/10 COVID-19 survivors. The mechanistic understanding of PACS remains poorly understood, which stymies treatment decision-making. In a PACS pilot study, we evaluated hyperpolarized 129Xe MRI ventilation defect percent and texture features to measure potential longitudinal changes. There were no significant differences in 129Xe MRI ventilation texture measurements six-months and 12-months after a baseline visit (12 weeks post-infection). PACS participants exhibited abnormal second-order 129Xe MRI ventilation textures and patchy ventilation, relative to healthy controls, 6-12 months post-infection.
|
||
2209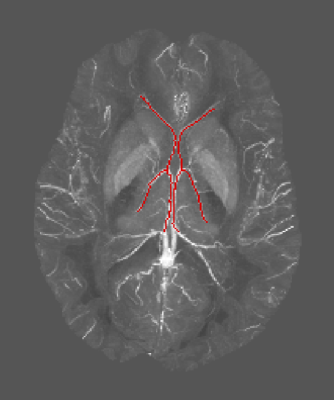 |
22 | The Impact of 3-ply and KN95 Facemasks on Cerebral Blood Flow and Oxygenation
Aisling Fothergill1,2,3, Christoph Birkl1,4, Christian Kames1,2, Alexander Weber1, and Alexander Rauscher1,2,5
1UBC MRI Research Centre, University of British Columbia, Vancouver, BC, Canada, 2Department of Physics and Astronomy, University of British Columbia, Vancouver, BC, Canada, 3Geoffrey Jefferson Brain Research Centre, Division of Neuroscience and Experimental Psychology, Faculty of Biology, Medicine and Health, University of Manchester, Manchester, United Kingdom, 4Department of Neuroradiology, Medical University of Innsbruck, Innsbruck, Austria, 5Department of Pediatrics, Division of Neurology, University of British Columbia, Vancouver, BC, Canada
Given the increased use of facemasks in everyday life, the impacts of these masks on cerebral blood flow (CBF) and oxygenation needs to be investigated. This study used pseudo-continuous arterial spin labeling (pCASL) and quantitative susceptibility mapping (QSM) to determine changes to grey matter CBF and oxygenation respectively. This was done by comparing facemask and no facemask scans for both 3-ply and KN95 masks. The average percent change between the facemask and no facemask oxygenation/susceptibility were insignificant for both mask types, and only the 3-ply facemask showed a statistically significant increase of 5.5% in CBF when wearing the facemask.
|
||
2210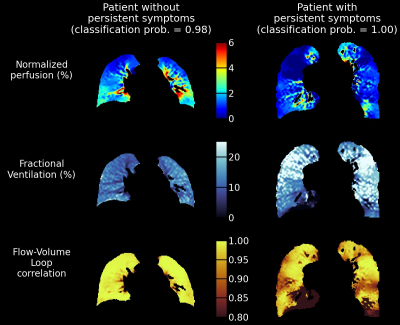 |
23 | Free-breathing low-field MRI of the lung exhibits functional damages associated with persistent symptoms in Covid-19 patients
Simon Lévy1, Rafael Heiss1, Robert Grimm2, David Grodzki2, Andreas Voskrebenzev3,4, Jens Vogel-Claussen3,4, Florian Fuchs5, Richard Strauss5, Susanne Achenbach6, Daniel Klett5, Jonas Schmid5, Andreas E. Kremer5,7, Michael Uder1, Armin M. Nagel1, and Sebastian Bickelhaupt1
1Institute of Radiology, University Hospital Erlangen, Friedrich-Alexander-Universität Erlangen-Nürnberg (FAU), Erlangen, Germany, 2MR Application Predevelopment, Siemens Healthcare, Erlangen, Germany, 3Institute of Diagnostic and Interventional Radiology, Hannover Medical School, Hannover, Germany, 4Biomedical Research in Endstage and Obstructive Lung Disease Hannover (BREATH), German Center for Lung Research (DZL), Hannover, Germany, 5Department of Medicine 1, University Hospital Erlangen, Friedrich-Alexander-Universität Erlangen-Nürnberg (FAU), Erlangen, Germany, 6Department of Transfusion Medicine and Haemostaseology, University Hospital Erlangen, Friedrich-Alexander-Universität Erlangen-Nürnberg (FAU), Erlangen, Germany, 7Department of Gastroenterology and Hepatology, University Hospital Zürich, Zürich, Switzerland
Free-breathing lung images were acquired at 0.55T in 73 Covid-19 patients, on average 5.4 months after the symptoms onset. Perfusion, fractional ventilation and Flow-Volume Loop correlation (FVLc) maps were extracted with the Phase-Resolved Functional Lung analysis technique, and percentages of defect areas were calculated. The most relevant predictors of the presence of persistent symptoms were the areas with concurrent perfusion and FVLc defects, and the areas without defects. Patients could be classified as symptomatic or asymptomatic with an accuracy of 71% when fitting a regression model with these predictors on the entire dataset and their combined score was significantly different.
|
||
2211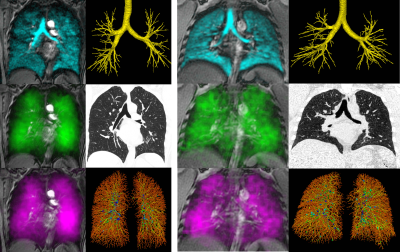 |
24 | 129Xe Gas-Transfer MRI RBC-to-Barrier Ratio in Post-Acute COVID19 Syndrome: Clinically-relevant?
Alexander M Matheson1, Harkiran K Kooner1, Elianna Bier2, Junlan Lu2, Bastiaan Driehuys2, Miranda Kirby3, Giles Santyr4,5, Mitchell S Albert6, Yurii Shepelytskyi6, Vira Grynko6, Sarah Svenningsen7,8, Alexei Ouriadov9, Inderdeep Dhaliwal10, J Michael Nicholson10, and Grace Parraga1,10
1Department of Medical Biophysics, Robarts Research Institute, Western University, London, ON, Canada, 2Center for In Vivo Microscopy, Duke University Medical Center, Durham, NC, United States, 3Department of Physics, Ryerson University, Toronto, ON, Canada, 4Hospital for Sick Children, Toronto, ON, Canada, 5Department of Medical Biophysics, University of Toronto, Toronto, ON, Canada, 6Thunder Bay Regional Health Research Institute, Lakehead University, Thunder Bay, ON, Canada, 7Division of Respirology, Department of Medicine, McMaster University, Hamilton, ON, Canada, 8St. Joseph's Healthcare, Hamilton, ON, Canada, 9Department of Physics and Astronomy, Western University, London, ON, Canada, 10Division of Respirology, Department of Medicine, Western University, London, ON, Canada
Post-acute COVID19 syndrome (PACS) is an umbrella term for a syndrome of symptoms persisting at least 12 weeks post COVID19 infection. Preliminary studies in PACS patients post-hospitalization revealed abnormally low 129Xe RBC-to-barrier ratios, but the clinical relevance of this is not well-understood. We acquired 129Xe gas-transfer MRI, spirometry, diffusing-capacity-of-the-lung for carbon-monoxide (DLCO) and same-day CT in 39 participants including 30 PACS and 9 never-COVID19 controls. The 129Xe MRI RBC-to-barrier ratio was significantly related to DLCO and significantly lower in both never-hospitalized and ever-hospitalized PACS patients compared to never-COVID19 controls.
|
||
2212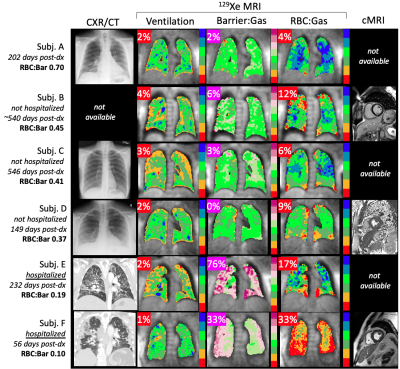 |
25 | Hyperpolarized 129Xe MRI is sensitive to variations in gas exchange impairment in patients with long haul COVID-19
David Mummy1, Elianna Bier2, Junlan Lu3, Suphachart Leewiwatwong2, Aryil Bechtel4, Isabelle Dummer5, Sakib Kabir1, Jennifer Korzekwinski1, Katherine Williford 6, Shelby Martindale6, Coral Giovacchini6, David Shaz6, Joseph Mammarappallil1, Fawaz Alenezi6, Raymond Kim6, Bastiaan Driehuys1, and Loretta Que6
1Radiology, Duke University, Durham, NC, United States, 2Biomedical Engineering, Duke University, Durham, NC, United States, 3Medical Physics, Duke University, Durham, NC, United States, 4Physics, Duke University, Durham, NC, United States, 5Bioengineering, McGill University, Montreal, QC, Canada, 6Medicine, Duke University, Durham, NC, United States
Many patients who recover from COVID-19 have symptoms that persist long after the acute phase of the disease has subsided, including fatigue and dyspnea on exertion. There is an unmet need for understanding the diverse cardiac and pulmonary causes of these symptoms and to monitor patients longitudinally. We imaged N=6 subjects with long-haul COVID using both cardiac MRI and hyperpolarized 129Xe MRI and spectroscopy. While cardiac imaging did not reveal structural or functional abnormalities, we observed a wide variety of findings on 129Xe MRI, with subjects who had been hospitalized exhibiting the most pronounced gas exchange impairment.
|
||
2213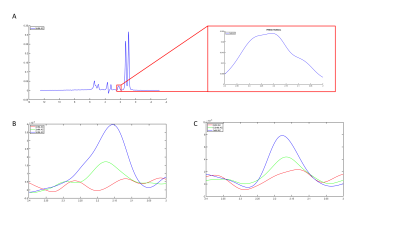 |
26 | Single-shot 3T 1H MRS with dual water/lipid VAPOR suppression for intrahepatic acetylcarnitine detection
Mijke Buitinga1,2, Julian Mevenkamp1, Florian Haans1, Kim Brouwers1, Patrick Schrauwen2, Lucas Lindeboom1,2, Joachim E Wildberger1, and Vera B Schrauwen-Hinderling1,2
1Department of Radiology & Nuclear Medicine, Maastricht University Medical Center, Maastricht, Netherlands, 2Department of Nutrition & Movement Sciences, University of Maastricht, Maastricht, Netherlands
We have developed a novel 3T 1H-MRS sequence to detect acetylcarnitine. Acetylcarnitine has been investigated by 1H-MRS in the muscle and is thought to play an important role in maintaining metabolic flexibility and insulin sensitivity. As these are hallmarks of metabolic disease, techniques to study acetylcarnitine levels non-invasively are of great interest. The advantage of our approach is the absence of a subtraction scheme and high signal intensity, while both water and lipid resonances are sufficiently suppressed to uncover the acetylcarnitine resonance. This makes our sequence suitable also for detection in tissues susceptible to respiratory motion, such as the liver.
|
||
The International Society for Magnetic Resonance in Medicine is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians.