Digital Poster
Cancer Therapy: MRI-Guided Interventions
Joint Annual Meeting ISMRM-ESMRMB & ISMRT 31st Annual Meeting • 07-12 May 2022 • London, UK

| Computer # | ||||
|---|---|---|---|---|
2139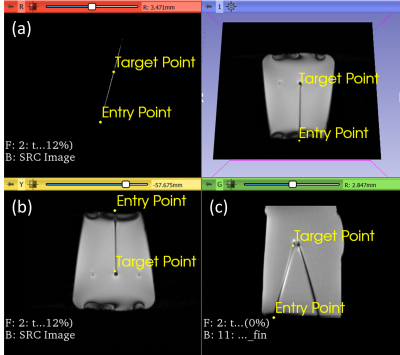 |
41 | Interactive Real-Time MRI-Guided Needle Tracking using Scanner Remote Control
Amanda Aleong1, Junichi Tokuda2, Pedro Moreira2, Ravi Seethamraju3, Gerald Moran4, Himanshu Bhat5, and Robert Weersink6
1Biomedical Engineering, University of Toronto, Toronto, ON, Canada, 2Radiology, Brigham and Women’s Hospital and Harvard Medical School, Boston, MA, United States, 3Siemens Medical Solutions USA Inc., Boston, MA, United States, 4Siemens Healthcare Ltd, Vineland, ON, Canada, 5Siemens Medical Solutions USA Inc., Newton, MA, United States, 6University of Toronto, Toronto, ON, Canada
MRI offers the gold standard for delineating cancerous lesions in soft tissue. Minimally invasive needle-based interventions require the accurate placement of multiple long, flexible needles at the target site. The manual tracking of needles in MR images is a time-consuming task that is further challenged by needle deflection. Automated needle segmentation offers the means to evaluate the alignment of the needle to the scan plane. This work demonstrates automatic needle tracking using remote scan control to dynamically update the scan plane of a real-time MR sequence. Automatic scan plane alignment is validated, and the feasibility of needle tracking is assessed.
|
||
2140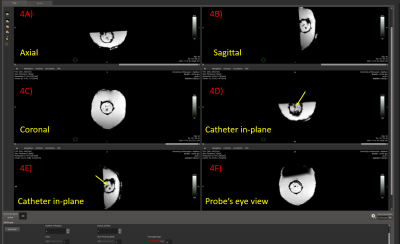 |
42 | Vendor Independent Visualization Platform for Neuro Device Guidance and Therapeutic Monitoring Based on Stereotactic OR Workstations
Robert Moskwa1, Eugene Ozhinsky2, Thomas Lilieholm1, Azam Ahmed3, and Walter F Block1
1Medical Physics, University of Wisconsin-Madison, Madison, WI, United States, 2Radiology, University of California, San Francisco, San Francisco, CA, United States, 3Neurological Surgery, University of Wisconsin-Madison, Madison, WI, United States
The NIH-sponsored international Phase III MISTIE Trial showed that that patients whose residual clot volume was reduced below 15 ml exhibited a statistically higher degree of functional independence. However, CT-image guidance has trouble visualizing clot, brain tissue, and intermediate levels of evacuation. MRI-guidance of ICH evacuations would support far better visualization of clots during attempts at suction or administration of lysing drugs. We present a six panel display whose viewpoints are patterned directly from the Medtronic Stealth workstation. This interface allows for acquisition and display of MR-images in real-time. Viewing planes and image parameters can be changed in real-time.
|
||
2141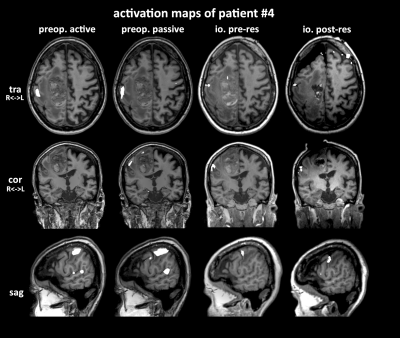 |
43 | Establishing a passive motor fMRI protocol for intraoperative 3T MRI: Preliminary results
Gilbert Hangel1, Jonathan Wais2, Matthias Tomschik2, Gudrun Mayr-Geisl2, Philip Pruckner3, Pedro Cardoso4, Christian Dorfer2, Gregor Kasprian3, and Karl Rössler2
1Department of Neurosurgery & High Field MR Centre, Medical University of Vienna, Wien, Austria, 2Department of Neurosurgery, Medical University of Vienna, Vienna, Austria, 3Division of Neuroradiology and Musculoskeletal Radiology, Department of Biomedical Imaging and Image-guided Therapy, Medical University of Vienna, Vienna, Austria, 4Medical University of Vienna, Vienna, Austria Using a 3T ioMRI system with an 8-channel intraoperative coil, we developed passive sensorimotor intraoperative fMRI protocol under anaesthesia at our site. We successfully applied it to passive fMRI of hand and foot in an exploratory cohort of four patients, confirming correspondence of activation to preoperative fMRI scans. This is the first reported implementation of intraoperative 3T passive fMRI. |
||
2142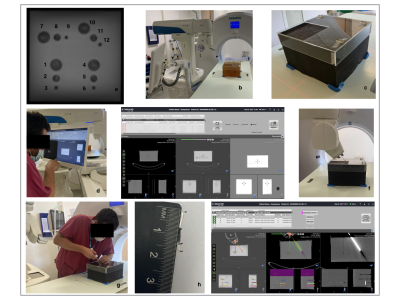 |
44 | Developing and testing robotic MRI/CT fusion biopsy using a novel home-made interventional phantom
Edward W Johnston1,2, Nicos Fotiadis1,2, Craig Cummings2, Toby Tyne 2, Jodie Basso1, Christina Messiou1,2, Dow-Mu Koh1,2, and Jessica M Winfield2,3
1Radiology, Royal Marsden Hospital, London, United Kingdom, 2Institute of Cancer Research, London, United Kingdom, 3MRI Unit, Royal Marsden Hospital, London, United Kingdom MRI/CT fusion may enable MRI-guided biopsy without the requirement for dedicated interventional MRI facilities. Assessment and training in MRI/CT-fusion biopsy requires phantoms containing targets that can be seen on MRI but not on CT and can be biopsied. These requirements are not met using commercially available phantoms. We produced a phantom containing targets that can be appreciated on MRI but not CT, which is reproducible, can be biopsied and assessed for core adequacy. We successfully biopsied targets (1-3cm diameter) using a commercially available interventional robot equipped with work-in-progress MRI/CT-fusion software, including targets with steep out-of-plane angulations, within clinically reasonable timeframes. |
||
2143 |
45 | Acquiring and Reconstructing UTE-Dixon Fat and Water Images for Generation of Synthetic CT in Thorax on an MR-Linac
Rosie Goodburn1, Wajiha Bano1, Uwe Oelfke1, and Andreas Wetscherek1
1Radiotherapy and Imaging, Institute of Cancer Research, London, United Kingdom
Generation of synthetic CT (synCT) for adaptive MR-guided radiotherapy is particularly challenging in the thorax due to the impact of respiratory motion, short-T2* tissues in lung, and a complex tissue-density structure. To address these challenges and provide data suitable for generating thoracic synCTs, we developed a UTE-Dixon sequence with a golden-angle stack-of-stars trajectory. We have demonstrated successful online acquisition and offline reconstruction of UTE, fat, water and B0 images as well as retrospective respiratory gating. Work is ongoing to optimize processing of respiratory-resolution of UTE and Dixon images that will form the input to synCT in thorax on an MR-Linac.
|
||
2144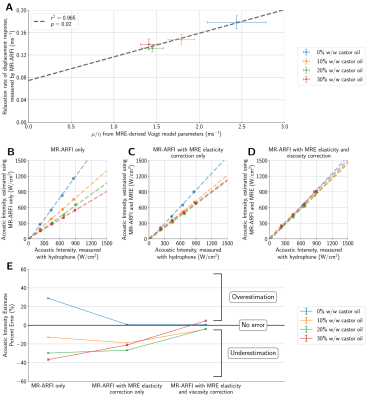 |
46 | Estimating acoustic intensity in viscoelastic media using MR acoustic radiation force imaging and multifrequency MR elastography
Ningrui Li1, Pooja Gaur2, Kristin Quah1, and Kim Butts Pauly2
1Electrical Engineering, Stanford University, Stanford, CA, United States, 2Radiology, Stanford University, Stanford, CA, United States
In addition to focal spot localization for non-ablative transcranial ultrasound therapies, MR acoustic radiation force imaging (MR-ARFI) has the potential to estimate the acoustic intensity delivered to the target. However, variability in tissue stiffness and viscosity precludes accurate estimates of acoustic intensity from MR-ARFI displacements alone. We demonstrate that multifrequency MRE can be used to characterize a medium’s viscoelastic response to focused ultrasound, improving estimates of acoustic intensity and enabling safer, more effective treatments.
|
||
2145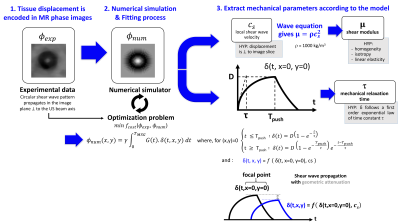 |
47 | MAGNETIC RESONANCE ACOUSTIC RADIATION FORCE IMAGING (MR-ARFI) FOR THE MONITORING OF MR-GUIDED HIFU THERAPY
Karine Choquet1, Jonathan Vappou1, Ounay Ishak1, Afshin Gangi1,2, and Elodie Breton1
1Université de Strasbourg, CNRS, ICube, UMR 7357, Strasbourg, France, 2Department of interventional imaging, Hôpitaux Universitaires de Strasbourg, Strasbourg, France Tissue biomechanical properties are highly promising biomarkers for HIFU ablation monitoring. A quantitative, MR-acoustic radiation force imaging (ARFI)-based method is proposed for measuring both tissue elasticity and viscosity, together with PRFS-derived temperature. This method is based on the identification of the MR-ARFI focal spot pattern. The method was first validated in a phantom with known properties. The method was then evaluated during HIFU heating in a gelatin phantom. Both elastic modulus and viscosity were found to decrease as temperature increased. These results highlight the ability of this method to provide new, quantitative biomarkers of tissue thermal damage in real time. |
||
2146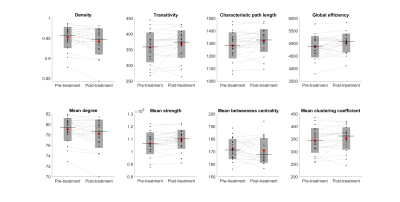 |
48 | Immediate changes in graph metrics following MRgFUS - an investigation using state-of-the-art diffusion image analysis
Arkiev D'Souza1, Fernando Calamante 1,2,3, Kain Kyle1,4, Stephen Tisch5, Ben Jonker5, Yael Barnett5, Joel Maamary5, Jerome Maller6, Justin Garber1, Michael Barnett1,4,7, and Chenyu Wang1,4
1Brain and Mind Centre, The University of Sydney, Camperdown, Australia, 2Sydney Imaging, The University of Sydney, Camperdown, Australia, 3School of Biomedical Engineering, The University of Sydney, Camperdown, Australia, 4Sydney Neuroimaging Analysis Centre, Camperdown, Australia, 5St Vincent's Hospital Sydney, Sydney, Australia, 6GE Healthcare Australia, Melbourne, Australia, 7Department of Neurology, Royal Prince Alfred Hospital, Camperdown, Australia
MRgFUS (Magnetic Resonance guided focused ultrasound) is an emerging treatment for tremor. The neuroadaptations that accompany desirable clinical outcomes following treatment are not well understood. Diffusion imaging can non-invasively quantify the structural connectivity between brain regions and may help explain tremor suppression mechanisms. Here, advanced diffusion analysis techniques were used to construct structural connectomes before and immediately after MRgFUS treatment in 27 patients with tremor. Graph theory metrics were measured on baseline and follow-up connectomes and differences between sessions were investigated using paired t-tests. Network density, characteristic path length, global efficiency, degree and strength changed following surgery (p<0.05).
|
||
2147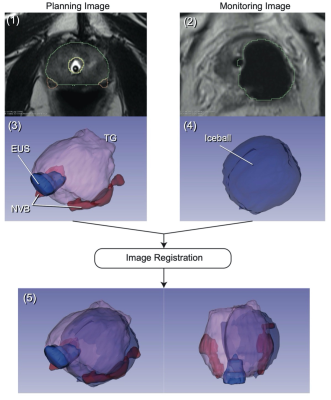 |
49 | AI-Assisted Analysis of Iceball Coverage on Patient Outcomes Following MR-guided Focal Cryoablation for Prostate Cancer: A Retrospective Study
Nicholas Fordham1,2, Junichi Tokuda1, Pedro Moreira1, Clare M Tempany1, and Kemal Tuncali1
1Department of Radiology, Brigham and Women's Hospital, Boston, MA, United States, 2Boston University School of Medicine, Boston, MA, United States
We conducted a retrospective study of 44 MRI-guided focal cryoablation cases for prostate cancer. Our goal was to evaluate AI-assisted MRI-based assessment of inadvertent cryoinjuries in the surrounding structures as predictors of post-procedural morbidities. Specifically, we estimated the iceball involvement with the external urethral sphincter (EUS) and the neurovascular bundle (NVB) using intraprocedural T2-weighted MRI and correlated with acute postoperative urinary incontinence and erectile dysfunction. The study demonstrated a correlation between incontinence and MRI-estimated iceball involvement with the EUS. However, no correlation was found between erectile dysfunction and the iceball involvement with the NVB.
|
||
2148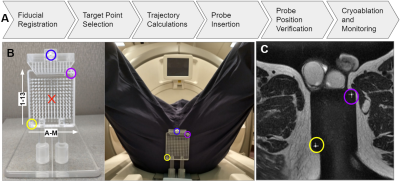 |
50 | Platform for Real-Time Multiplane Targeting and Monitoring of Minimally-Invasive Image-Guided Prostate Cryoablation Procedures
Thomas Lilieholm1, Robert Moskwa1, Eugene Ozhinsky2, David A Woodrum3, Walter F Block1,4,5, and Erica M Knavel Koepsel6
1Medical Physics, University of Wisconsin - Madison, Madison, WI, United States, 2Radiology, University of California - San Francisco, San Francisco, CA, United States, 3Radiology, Mayo Clinic, Rochester, MN, United States, 4Radiology, University of Wisconsin - Madison, Madison, WI, United States, 5Biomedical Engineering, University of Wisconsin - Madison, Madison, WI, United States, 6Interventional Radiology, University of Wisconsin - Madison, Madison, WI, United States
Minimally invasive cryoablation is an effective and safe treatment option for localized low- and intermediate-risk prostate cancers. Precisely placed cryoprobes in cancerous regions of the prostate kill malignant cells by freezing local tissues while being less invasive than prostatectomy, and having a shorter treatment cycle than most radiotherapies. For accurate probe placement, MR-image guidance is often employed, coupled with external probe-guiding apparati. We developed a platform that enables a cohesive workflow to register the probe-guiding apparati, facilitate target selection, select and verify probe trajectory, and monitor the prostate in real-time using multiple planes during probe insertion and cryoablation freeze cycles.
|
||
2149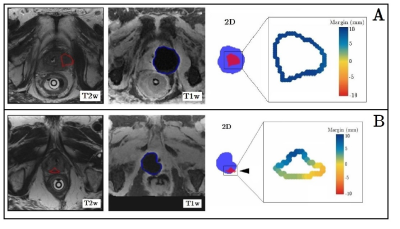 |
51 | Deep learning-assisted ablative margin analysis for MR-guided prostate focal cryoablation: feasibility and initial retrospective validation
Daan N. Schouten1, Cees H. Slump2, Jurgen J. Fütterer1,2, Joyce G.R. Bomers1, and Christiaan G. Overduin1
1Medical Imaging, Radboudumc, Nijmegen, Netherlands, 2Robotics and Mechatronics, University of Twente, Enschede, Netherlands
MR-guided focal cryoablation is an emerging treatment option for localized prostate cancer, however local recurrence due to incomplete ablation is not uncommon. Ablation completeness is typically assessed on intraprocedural imaging by side-by-side comparison, but a volumetric approach is lacking. We present a deep learning-assisted algorithm for near real-time ablative margin monitoring during cryoablation procedures. Retrospective validation in 27 patients after MR-guided prostate cryoablation demonstrated significantly smaller minimal ablative margin and percentual tumour coverage for patients with versus without local recurrence. Prospective use may aid physicians in reducing the risk of local recurrence during prostate cryoablation procedures.
|
||
2150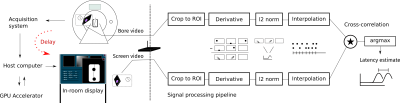 |
52 | Measurement of End-to-End latency in real-time MRI
Philip Schaten1, Mueed Azhar2, Ansgar Adler3, Michael Steinmetz2,4,5, and Martin Uecker1,3,4
1Institute for Diagnostic and Interventional Radiology of the University Medical Center Göttingen, Göttingen, Germany, 2Department of Pediatric Cardiology of the University Medical Center Göttingen, Göttingen, Germany, 3Institute of Medical Engineering, Graz University of Technology, Graz, Austria, 4DZHK (German Centre for Cardiovascular Research), Partner Site Göttingen, Göttingen, Germany, 5Goettingen Heart Center, University Medical Center Göttingen, Göttingen, Germany
For interventional MRI-guided applications image reconstruction should be without delay to avoid unwanted failure. Since latency is unavoidable it is very important to know it beforehand. For this reason, we present a new method to measure the latency of real-time MRI systems.
The main components are two inexpensive optical cameras. No modification of the scanner system is required. Different validations show that our method works reliably. Results from our RT MRI system provide insight into the latency of different protocols. We believe that we have found an inexpensive, easy, and robust way of determining RT MRI latency. |
||
2151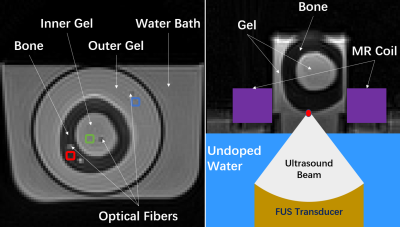 |
53 | Combining Proton Resonance Frequency Shift and T1-mapping Thermometry with a 3D Spiral Ultra-Short Echo Time Sequence
Sheng Chen1, Yekaterina K. Gilbo1, Helen L. Sporkin1, Samuel W. Fielden2, Steven P. Allen1,3, John P. Mugler III4, G. Wilson Miller4, and Craig H. Meyer1,4
1Biomedical Engineering, University of Virginia, Charlottesville, VA, United States, 2Department of Imaging Sciences & Innovation, Geisenger, Danville, PA, United States, 3Electrical and Computer Engineering, Brigham Young University, Provo, UT, United States, 4Radiology and Medical Imaging, University of Virginia, Charlottesville, VA, United States Temperature monitoring plays an essential role in transcranial MR-guided focused ultrasound (tcMRgFUS) surgery for measuring thermal dose at the target. Unintended heating of the skull and nearby brain tissue is not currently monitored. By using a two-echo 3D spiral ultra-short echo time (UTE) sequence, we demonstrate a method that combines T1-mapping and proton resonance frequency (PRF) shift thermometry to simultaneously monitor skull and brain heating and validate it in an in vitro model. |
||
2152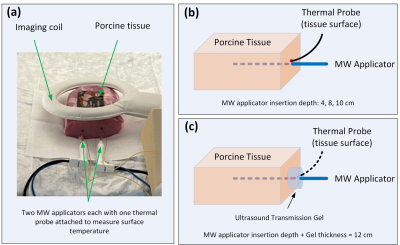 |
54 | Investigation of heating risks during MR-guided microwave ablation using applicators without active shaft cooling
Liqiang Ren1, David A Woodrum1, Krzysztof R Gorny1, Joel P Felmlee1, Scott M Thompson1, and Aiming Lu1
1Radiology, Mayo Clinic, Rochester, MN, United States
Execution of MR sequences (RF-heating) and/or microwave energy during MRgMWA may lead to harmful heating at tissue surface with non-cooled MR-conditional applicators. MR imaging was performed using a high SAR sequence and several geometric orientations of phantom/applicators to assess RF-heating impact. Applicator insertion depth (with/without ultrasound gel) and spacing of two applicators on shaft heating were evaluated. Negligible temperature changes due to RF-heating were observed. Significant temperature increases were measured during MWA due to action of MWA system/applicator, which can be mitigated by increasing the applicator insertion depth. Further reduction in temperature change can be achieved by using ultrasound gel.
|
||
2153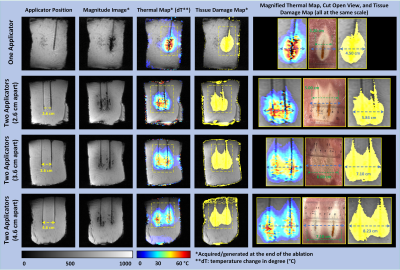 |
55 | Feasibility of microwave ablation using two applicators with real-time MR thermometry
Liqiang Ren1, David A Woodrum1, Krzysztof R Gorny1, Joel P Felmlee1, Christopher P Favazza1, Scott M Thompson1, and Aiming Lu1
1Radiology, Mayo Clinic, Rochester, MN, United States
Simultaneous use of multiple applicators is desirable in MRgMWA when treating large tumors and its feasibility is investigated in phantom experiments to evaluate the impact of MW system on MR image quality and in ex-vivo experiments with porcine tissue to compare MWA procedures with one and two applicators. Relative SNR was dropped from 88.1% with one applicator activated to 54.6% with both activated, yet temperature and tissue damage maps with acceptable image quality were obtained. Simultaneous use of two MW applicators could significantly increase the treatment efficiency with a larger ablation zone when both applicators are properly selected and configured.
|
||
The International Society for Magnetic Resonance in Medicine is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians.