Digital Poster
Cancer Therapy: Radiation Therapy & Surgery
Joint Annual Meeting ISMRM-ESMRMB & ISMRT 31st Annual Meeting • 07-12 May 2022 • London, UK

| Computer # | ||||
|---|---|---|---|---|
2214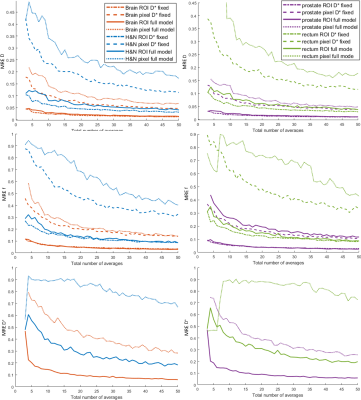 |
27 | Data-driven optimization of intravoxel incoherent motion imaging for clinical endpoints in radiotherapy on a 1.5 T MR-Linac
Andreas Wetscherek1, Brigid A McDonald2, Ernst S Kooreman3, Angus Z Lau4,5, Ramesh Paudyal6, Amita Shukla-Dave6,7, Liam SP Lawrence4,5, Petra J van Houdt3, and Uulke A van der Heide3
1Joint Department of Physics, The Institute of Cancer Research and The Royal Marsden NHS Foundation Trust, London, United Kingdom, 2Department of Radiation Oncology, The University of Texas MD Anderson Cancer Center, Houston, TX, United States, 3Department of Radiation Oncology, The Netherlands Cancer Institute, Amsterdam, Netherlands, 4Physical Sciences Platform, Sunnybrook Research Institute, Toronto, ON, Canada, 5Department of Medical Biophysics, University of Toronto, Toronto, ON, Canada, 6Department of Medical Physics, Memorial Sloan Kettering Cancer Center, New York, NY, United States, 7Department of Radiology, Memorial Sloan Kettering Cancer Center, New York, NY, United States
Measuring the detectable effect size is crucial for setting up clinical trials involving quantitative MRI for treatment adaptation, response assessment and outcome prediction in MR-guided radiotherapy. For four different tumor sites (brain, head and neck, prostate and rectum) diffusion-weighted MRI protocols were optimized for intravoxel incoherent motion imaging based on minimizing the mean relative error of the IVIM parameters. For full IVIM model fits, 4-5 b-values were found optimal, while a fit with fixed D* was best performed with 3 b-values. MR-Linac systems currently have limitations regarding gradient performance and number of coil channels and qMRI techniques require careful optimization.
|
||
2215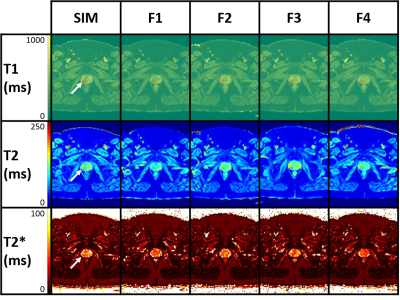 |
28 | Multi-parametric MRI on a 0.35 T MR-LINAC: application to prostate radiotherapy treatment follow-up
Louis Marage1, Igor Bessières1, Magali Quivrin2, Aubignac Léone1, Karine Peignaux-Casanovas2, Gilles Truc2, Paul-Michael Walker1, and Stanislas Rapacchi3
1Medical Physics, Centre Georges-François Leclerc, Dijon, France, 2Radiotherapy, Centre Georges-François Leclerc, Dijon, France, 3Aix-Marseille Univ, CNRS, CRMBM, Marseille, France - The proposed method allows a comprehensive relaxation times estimation (T1, T2, T2*) on MRgRT systems. - The methodology was validated on phantom and volunteer for accuracy and reproducibility. - For T1 and T2, less than 5 % coefficient of variation was observed and less than 10 % for the T2*. - Trends on 5 patients show a slight decrease and a recovery for the T1 and T2 values in both the boost and whole prostate during their treatment. - The dispersion of T1 and T2 decreased for all patients for the whole prostate whereas it was stable for the boost. |
||
2216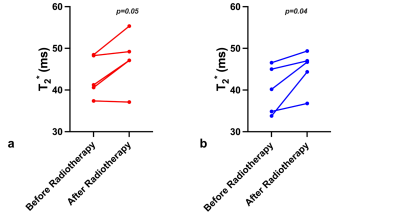 |
29 | Integration of T2* mapping in daily prostate MR-Linac workflow for hypoxia characterisation
Wajiha Bano1, Kobika Sritharan2, Uwe Oelfke1, Alison Tree2, and Andreas Wetscherek1
1Joint Department of Physics, The Institute of Cancer Research and The Royal Marsden NHS Foundation Trust, London, United Kingdom, 2Department of Radiotherapy, The Royal Marsden NHS Foundation Trust, London, United Kingdom
T2* mapping can be a potential biomarker to characterise hypoxia and monitor treatment response throughout the course of MR-guided radiotherapy on an MR-Linac. This study explores the feasibility of integrating T2* mapping in daily prostate MR-Linac workflow using a cohort of patients with prostate cancer. We compared mean T2* values within the prostate with repeated measures acquired twice weekly during radiotherapy. T2* values at the end of treatment were higher than at the first fraction but didn’t show a consistent trend throughout treatment. Integrating T2* mapping with other functional measurements can aid in response based treatment adaptation.
|
||
2217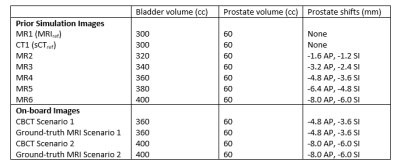 |
30 | On-board pseudo-MRI guidance for prostate radiotherapy on a conventional X-ray guided LINAC
Wendy Harris1, Ergys Subashi1, Victoria Yu1, Eric Aliotta1, Ricardo Otazo1, and Laura Cervino1
1Medical Physics, Memorial Sloan Kettering Cancer Center, New York, NY, United States
Current target localization for prostate radiotherapy on a conventional LINAC consists of acquiring a cone-bean CT (CBCT) image and matching it to implanted fiducial markers inside the prostate due to poor soft-tissue contrast of CBCT. MRI provides better soft tissue contrast and no ionization radiation, but there are very few MR-LINACs, and conventional LINACs with x-ray imaging capabilities are much more ubiquitous. This study proposes to use prior MRI acquisitions, PCA motion modeling, and on-board CBCT from a conventional LINAC to obtain on-board pseudo-MRI for target localization in prostate radiotherapy.
|
||
2218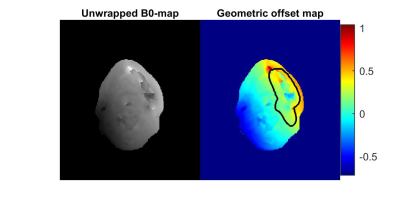 |
31 | Estimation and visualization of geometric fidelity using geometric offset maps for improved guidance in H&N radiation therapy
Emilia Palmér1, Maria Ljungberg1,2, Anna Karlsson1,2, Fredrik Nordström1,2, Karin Petruson3, and Maja Sohlin1,2
1Department of Radiation Physics, Institute of Clinical Sciences, University of Gothenburg, Gothenburg, Sweden, 2Department of Medical Physics and Biomedical Engineering, Sahlgrenska University Hospital, Gothenburg, Sweden, 3Department of Oncology and Radiotherapy, Institute of Clinical Sciences, University of Gothenburg, Gothenburg, Sweden
In an MRI-only workflow, high geometric fidelity of the MRI data is required. Head and neck (H&N) cancer patients, however, frequently have implants, e.g., dental restorations, causing distortions of the MRI data. Geometric offset maps were computed using B0-map calculated from the Dixon-sequence included in the standard clinical protocol. Even though the implants included in this pre-study did not contribute with a significant geometric offset in the delineated target volume, visualization of the geometric offset maps as such bring additional important information when delineating structures in an MRI-only H&N workflow and could thereby become a promising tool in clinical practice.
|
||
2219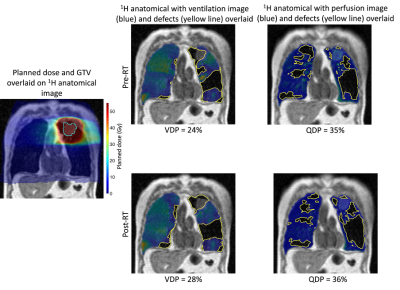 |
32 | Multi-modal assessment of dose-related changes in regional lung function in non-small cell lung cancer patients receiving radiotherapy
Bilal A Tahir1,2,3, Paul JC Hughes2, Jack Atkinson2,3, Isaac Jadav1, Joshua R Astley1,2, Stephen D Robinson1,4, Alberto Biancardi2, Helen Marshall2, Kerry A Hart1,5, James A Swinscoe1, Rob H Ireland1,2, Matthew Q Hatton1,4, and Jim M Wild2,3
1Department of Oncology and Metabolism, The University of Sheffield, Sheffield, United Kingdom, 2POLARIS, Department of Infection, Immunity and Cardiovascular Disease, The University of Sheffield, Sheffield, United Kingdom, 3Insigneo Institute for in silico medicine, The University of Sheffield, Sheffield, United Kingdom, 4Clinical Oncology, Weston Park Cancer Centre, Sheffield, United Kingdom, 5Radiotherapy Physics, Weston Park Cancer Centre, Sheffield, United Kingdom
Radiotherapy plays a central role in the management of lung cancer. However, despite advances, survival of lung cancer patients undergoing radiotherapy remains poor, partly attributable to the incidence of radiation-induced lung injury, which is exacerbated in patients with poor pulmonary function. Both ventilation and perfusion information are vital to providing a complete picture of pulmonary function, ideally in a regional fashion. Here, we develop and apply an image acquisition and analysis pipeline to assess dose-related changes in regional lung function as derived from hyperpolarized gas ventilation and dynamic contrast-enhanced perfusion MRI in lung cancer patients receiving a course of radiotherapy.
|
||
2220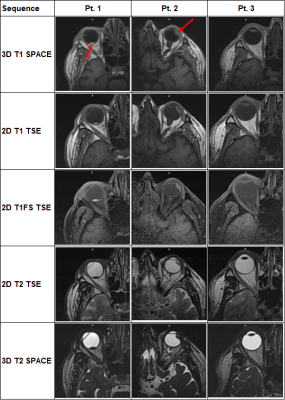 |
33 | MR Protocol Optimization for Treatment Planning Simulation of Ocular Melanoma Proton Therapy
Matthew John Goette1,2, Roelf Slopsema3, Anees Dhabaan3, and Hui-Kuo Shu3
1Radiology and Imaging Sciences, Emory Healthcare, Atlanta, GA, United States, 2Radiation Oncology, Emory Healthcare, Atlanta, GA, United States, 3Radiation Oncology, Emory University, Atlanta, GA, United States
An MR treatment planning simulation protocol for proton therapy in patients with ocular melanoma was optimized using a 70-mm loop coil.
|
||
2221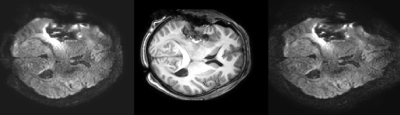 |
34 | Exploring the use of Echo Planar Image Correction (EPIC) for intra operative Diffusion Tensore Imaging. – Initial results
Svein Are Sirirud Vatnehol1,2, Einar Vik-Mo3, and Ragnhild Marie Undseth1
1The Intervention Centre, Oslo University Hospital, Oslo, Norway, 2Department of Optometry, Radiography and Lighting Design, University of South-Eastern Norway, Drammen, Norway, 3Department of Neurosurgery, Oslo University Hospital, Oslo, Norway
Intra operative MRI with Diffusion Tensor Imaging allows identification of white mater tracks during surgery allowing for a more aggressive approach by the surgeon while preserving eloquent structures. However DTI is prone to artefacts from B0 inhomogeneity. In this abstract we present our initial experiences on the effect of a commercially available Echo Planar Imaging Correction in the intraoperative setting. While overall image quality is increased, further studies on a larger number of patients are required before the clinical effect can be assessed.
|
||
2222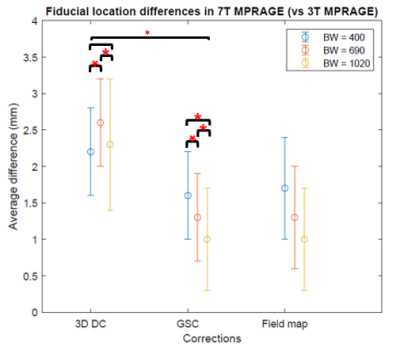 |
35 | Use of 7 Tesla MRI for frameless pre-surgical planning with skin-adhesive fiducials
Andrew J Fagan1, Krystal Kirby1, Emily Koons1, and Kirk M Welker1
1Radiology, Mayo Clinic, Rochester, MN, United States
This study aimed to investigate the use of 7 Tesla MRI for frameless pre-surgical planning for tumor resection applications. Image geometric distortions at the locations of 10 skin-adhered fiducials were minimized in 7 Tesla images, and compared to in vivo results from a current 3 Tesla frameless imaging protocol. Geometric accuracy of < 1 mm was obtained in 7 Tesla images at the surface of a head-shaped phantom.
|
||
The International Society for Magnetic Resonance in Medicine is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians.