Digital Poster
Breast Cancer: Diagnosis & Imaging Treatment Response
Joint Annual Meeting ISMRM-ESMRMB & ISMRT 31st Annual Meeting • 07-12 May 2022 • London, UK

| Computer # | ||||
|---|---|---|---|---|
1588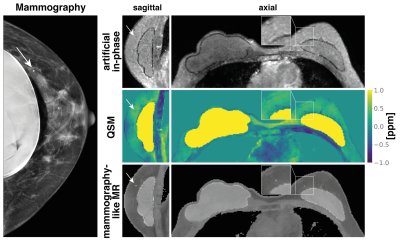 |
43 | Mammography-like MR images using a preconditioned water-fat-silicone total field inversion QSM algorithm
Christof Boehm1, Jonathan K. Stelter1, Jakob Meineke2, Stefan Ruschke1, Kilian Weiss3, Mingming Wu1, Tabea Borde1, Marcus R. Makowski1, Eva M. Fallenberg1, and Dimitrios C. Karampinos1
1Department of Diagnostic and Interventional Radiology, School of Medicine, Klinikum Rechts der Isar, Technical University of Munich, Munich, Germany, 2Philips Research, Hamburg, Germany, 3Philips GmbH Market DACH, Hamburg, Germany
Early stage malignant tumors are often accompanied by microcalcifications. X-ray-based mammography examinations are routinely used for screening and early detection due to the excellent contrast of calcified structures. However, due to the damaging nature of x-ray radiation, the use of an MR-based technique would be desirable for repeated examinations. In this work, we present initial results of quantitative-susceptibility-mapping-based (QSM) mammography-like MR-images that show robust detection of calcifications down to the resolution of the MR scan. Furthermore, the proposed method accounts for the potential presence of silicone breast implants allowing robust QSM in proximity to silicone implants for the first time.
|
||
1589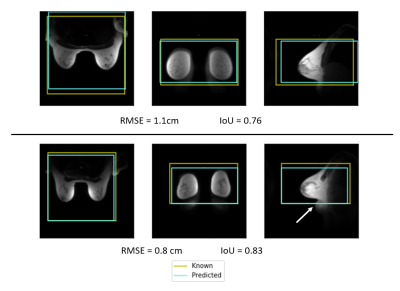 |
44 | Towards Automated Scan Volume Placement for Breast MRI Using a Deep Neural Network
Timothy J Allen1, Leah C Henze Bancroft2, Ersin Bayram3, Lloyd Estkowski4, Pingni Wang5, Ty A Cashen6, and James H Holmes7
1Medical Physics, University of Wisconsin-Madison, Madison, WI, United States, 2Radiology, University of Wisconsin-Madison, Madison, WI, United States, 3GE Healthcare, Houston, TX, United States, 4GE Healthcare, Waukesha, WI, United States, 5GE Healthcare, Menlo Park, CA, United States, 6GE Healthcare, Madison, WI, United States, 7Radiology, University of Iowa, Iowa City, IA, United States We investigate the use of a deep neural network to automatically position imaging volumes for breast MR exams. The axial localizer images and scan volume information from a variety of MR scanners were used to train a deep neural network to replicate the clinical technologists’ placement. The average intersection over union between clinical placement and neural network predicted placement was 0.46 ± 0.21. The distance between volume centers was 7.4 cm on average and as low as 1.1 cm. These results show promise for improving consistency of imaging volume placement in breast MRI. |
||
1590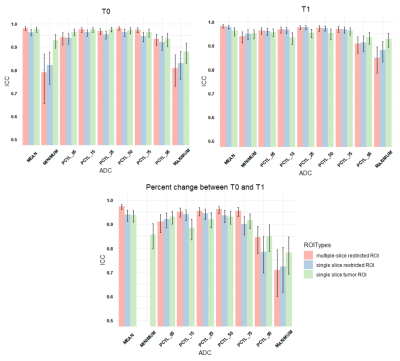 |
45 | Inter-reader variability in apparent diffusion coefficient measurements for assessment of breast cancer response to neoadjuvant therapy
Nu N. Le1, Wen Li1, Natsuko Onishi1, David Newitt1, Jessica Gibbs1, Lisa Wilmes1, John Kornak2, Savannah C. Partridge3, Elissa Price1, Bonnie N. Joe1, Laura Esserman2, and Nola M. Hylton1
1Radiology, UCSF, San Francisco, CA, United States, 2UCSF, San Francisco, CA, United States, 3University of Washington, Seattle, WA, United States
This study presents a retrospective analysis of inter-reader variability in tumor ADC measurements extracted from three types of ROIs using data from the multi-center I-SPY 2 trial. Overall, good agreement was observed between two readers. Mean ADCs measured in restricted ROIs were highly reproducible by manual delineation. Mean ADCs of multi-slice restricted ROIs showed higher ICCs than single-slice restricted ROIs.
|
||
1591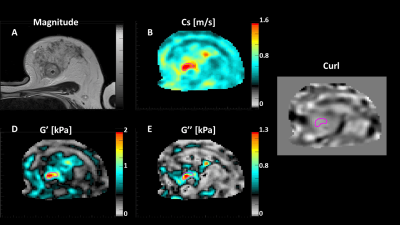 |
46 | Magnetic Resonance Elastography for Early Assessment of Response to Neoadjuvant Chemotherapy in Women with Breast Cancer Video Permission Withheld
Patriek Jurrius1,2, Omar Darwish3,4,5, Daniel Fovargue3, Belul Shifa6, Karen Welsh7, Joanna Bell7, Sarah-Jane Hamilton7, John Spence7, Giacomo Annio4, Renee Miller3, Marian Troelstra3, Ashutosh Kothari2, Hisham Hamed2, Georgina Bitsakou2, Ali Sever8, Sultana Hasso8, Yasmin Giambrone8, Isaac Daimiel Naranjo8, Katerina Ntailiani8, Keshthra Satchithananda9,
Sarah Willson8, Sarah Pinder1,10, Anne Rigg11, David Nordsletten3, Radhouene Neji3,5, Tony Ng1, Arnie Purushotham1,2, and Ralph Sinkus3,4
1School of Cancer & Pharmaceutical Sciences, King's College London, London, United Kingdom, 2Oncoplastic breast surgery, Guy's & St. Thomas' NHS Foundation Trust, London, United Kingdom, 3School of Biomedical Engineering & Imaging Sciences, King's College London, London, United Kingdom, 4Inserm U1148, LVTS, University Paris Diderot, Paris, France, 5MR Research Collaborations, Siemens Healthcare Ltd., Frimley, United Kingdom, 6Oncology and Haematology Clinical Trials, Guy's & St. Thomas' NHS Foundation Trust, London, United Kingdom, 7MRI department, Guy's & St. Thomas' NHS Foundation Trust, London, United Kingdom, 8Breast Radiology, Guy's & St. Thomas' NHS Foundation Trust, London, United Kingdom, 9Breast Radiology, King's College Hospital NHS Foundation, London, United Kingdom, 10Histopathology, Guy's & St. Thomas' NHS Foundation Trust, London, United Kingdom, 11Medical Oncology, Guy's & St. Thomas' NHS Foundation Trust, London, United Kingdom Approximately one-third of women with breast cancer undergoing neoadjuvant chemotherapy (NACT) have no discernible disease response to their treatment yet are subjected to the potential side-effects of their treatment. Currently, response to NACT is assessed by determining tumour size, contrast avidity, and lymph node involvement on MRI pre-, mid- and post-treatment. As a result, women undergo 3-4 cycles of NACT with unknown efficacy. Changes in a tumour’s biomechanics as assessed by magnetic resonance elastography (MRE) after only one cycle of NACT correlate with response to treatment, allowing for early assessment of a patient’s response to NACT. |
||
1592 |
47 | Monitoring the response of breast tumors to neoadjuvant chemotherapy using multimodal magnetic resonance and optical imaging – a case study
Bin Deng1,2,3, Ailis Muldoon1,2, Pedro Itriago4, Wei-Ching Lo5, Mansi Saksena2,3, Samuel Patz3,6, Ralph Sinkus7, Steven J. Isakoff3,8, and Stefan A. Carp1,2,3
1Athinoula A. Martinos Center for Biomedical Imaging, Massachusetts General Hospital, Charlestown, MA, United States, 2Department of Radiology, Massachusetts General Hospital, Boston, MA, United States, 3Harvard Medical School, Boston, MA, United States, 4Siemens Medical Solutions, Houston, TX, United States, 5Siemens Medical Solutions, Boston, MA, United States, 6Department of Radiology, Brigham and Women’s Hospital, Boston, MA, United States, 7Laboratory for Vascular Translational Science (LVTS), Institut National de la Santé et de la Recherche Médicale (INSERM), Paris, France, 8Cancer Center, Massachusetts General Hospital, Boston, MA, United States
Functional imaging is advantageous in monitoring neoadjuvant chemotherapy (NACT) since changes in tumor physiology manifest earlier than actual tumor shrinkage. We leveraged a custom breast coil for multimodal T1, DWI, MRE, and near-infrared optical imaging to evaluate the response of breast tumors to NACT. In this case study of a patient who achieved pathologic complete response, concordant changes in tumor size, ADC, stiffness and total hemoglobin concentration have been observed. This multiparametric approach could help us gain a comprehensive understanding of the multitude of simultaneous physiological changes in tumors related to microenvironment, angiogenesis, and metabolism as a result of NACT.
|
||
1593 |
48 | Predicting response to neoadjuvant therapy using tumor morphologic features on breast MRI
Wen Li1, Rohan Nadkarni1, David C Newitt1, Natsuko Onishi1, Jessica Gibbs1, Lisa J Wilmes1, Bonnie N Joe1, Efstathios D Gennates2, John Kornak2, Mark Magbanua3, Laura van't Veer3, Barbara LeStage4, I-SPY 2 Consortium5, Laura J Esserman6, and Nola M Hylton1
1Radiology & Biomedical Imaging, University of California, San Francisco, San Francisco, CA, United States, 2Epidemiology & Biostatistics, University of California, San Francisco, San Francisco, CA, United States, 3Laboratory Medicine, University of California, San Francisco, San Francisco, CA, United States, 4I-SPY 2 Advocacy Group, San Francisco, CA, United States, 5Quantum Leap Healthcare Collaborative, San Francisco, CA, United States, 6Surgery, University of California, San Francisco, San Francisco, CA, United States
Functional tumor volume (FTV) has been used to longitudinally assess tumor response to neoadjuvant therapy longitudinally in I-SPY trials. Previously, we found that a single 3D shape feature, sphericity, is associated with pathologic complete response (pCR). In this study, we expanded the analysis by including all radiomic shape features in an elastic net model and evaluated their role in prediction of pCR in the multi-center I-SPY 2 trial. Our results showed that the model with shape features outperformed the models with FTV or sphericity alone.
|
||
1594 |
49 | How much earlier did MRI detect breast cancer than mammography in the DENSE trial?
Keith S Cover1
1., Amsterdam, Netherlands
The current analysis found MRI screening in the DENSE trial detected invasive breast cancers about 6 years earlier than mammography. The calculation is based on first and second round invasive cancer detection rates. The 6 years is also consistent with the trial’s high false positive rate in the second round that used “prior” first round exams to estimate lesion growth over the 2 years between rounds. The “how much earlier” measure provides an additional means for comparing the relative performance of breast cancer screening modalities.
|
||
1595 |
50 | Assessment of the Diagnosis Value of Diffusion Tensor Imaging and Fractional Anisotropy Value in Peripheral Prostate Cancer based on PI-RADS v2 Video Not Available
Zhiqiang Chen1, Na Song1, Dan Zhang1, Zhuo Wang1, Shaoru Zhang1, Yuhui Xiong2, Aijun Wang1, Bing Chen1, and Lei Cai1
1Radiology, The Department of Radiology, General Hospital of Ningxia Medical University, Yinchuan, China, 2GE Healthcare, MR Research China, Beijing, Beijing, China In this retrospective study, we aim to explore the diagnostic values of diffusion tensor imaging (DTI) in peripheral prostate cancer, and compare DTI with diffusion weighted imaging (DWI) based on prostate imaging reporting and data system version 2 (PI-RADS v2) in peripheral prostate cancer (PCa). It was concluded that both DWI and DTI have high values in the diagnosis and differentiation of PCa, and DWI& dynamic contrast enhanced (DCE) MRI has higher diagnostic efficiency than DTI&DCE-MRI according to PI-RADS v2. |
||
The International Society for Magnetic Resonance in Medicine is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians.