Online Gather.town Pitches
Ocular & Neurological Disorders
Joint Annual Meeting ISMRM-ESMRMB & ISMRT 31st Annual Meeting • 07-12 May 2022 • London, UK

| Booth # | ||||
|---|---|---|---|---|
3886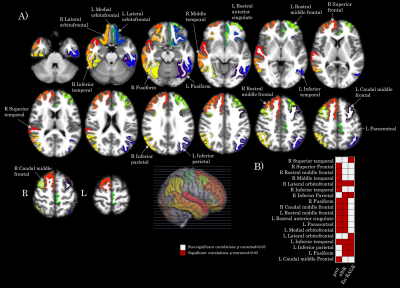 |
1 | Brain cortical changes are related to SARS-CoV-2 inflammatory biomarkers in hospitalized patients with neurological manifestations
Gretel Sanabria-Diaz1, Manina Maja Etter 2,3, Lester Melie-Garcia1,4, Johanna Maria Lieb5, Marios-Nikos Psychogios5, Gregor Hutter2,3, and Cristina Granziera1,4
1Department of Medicine and Biomedical Engineering, Translational Imaging in Neurology (ThINK), University Hospital Basel and University of Basel, Basel, Switzerland, 2Department of Biomedicine, University Hospital Basel and University of Basel, Basel, Switzerland, 3Division of Neurosurgery, University Hospital Basel, Basel, Switzerland, 4Neurologic Clinic and Policlinic, MS Center and Research Center for Clinical Neuroimmunology and Neuroscience Basel (RC2NB), University Hospital Basel and University of Basel, Basel, Switzerland, 5Department of Neuroradiology, Clinic of Radiology and Nuclear Medicine, University Hospital Basel, Basel, Switzerland
A quantitative imaging study is critical to detect cortical brain macrostructural alterations associated with an inflammatory response in hospitalized SARS-CoV-2 patients. Using automated processing of the 3D high-resolution T1-weighted anatomical images, we found a decrease of cortical gray matter volume and thickness, but not in the surface area related to increased levels in CSF protein, CSF blood/albumin ratio, and CSF EN-RAGE. The anatomical localization of these regions may be the in vivo hallmarks of the virus effect on the brain cortex due to a hyperinflammatory response and associated with neurological deficits presented in acute and post-Covid phases.
|
||
3887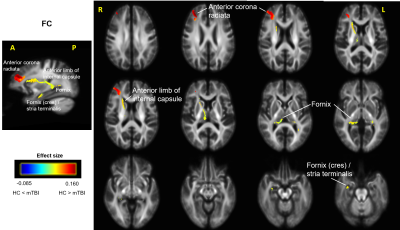 |
2 | A fixel-based analysis of white matter alterations in patients with acute mild traumatic brain injury
Li Jiang1,2, Jiachen Zhuo1,2, Steven Roys1,2, Rosy Linda Njonkou Tchoquessi1,2, and Rao Gullapalli1,2
1Center for Advanced Imaging Research, University of Maryland Baltimore, Baltimore, MD, United States, 2Department of Diagnostic Radiology & Nuclear Medicine, University of Maryland Baltimore, Baltimore, MD, United States
Mild traumatic brain injury (mTBI) accounts for the majority of head injuries and is often associated with physical, cognitive, and effective deficits. We used fixel-based analysis (FBA) to investigate the white matter (WM) structural alterations in acute mTBI patients. Three fixel-based metrics were used: fibre density (FD), fibre-bundle cross-section area (FC) and a combination of FD and FC (FDC). We found out that mTBI patients demonstrated reduced FC and FDC in multiple WM tracts and it may suggest that FBA can be used to detect subtle WM changes following mild injuries.
|
||
3888 |
3 | Genetic susceptibility to myelin and axonal injury as measured by myelin water imaging and multi-shell diffusion in multiple sclerosis
Reza Rahmanzadeh1,2, Stefan Herms3, Bettina Burger3, Po-Jui Lu1,2, Muhamed Barakovic1,2, Matthias Weigel1,2, Thanh D. Nguyen4, Yi Wang4, Francesco La Rosa 5,6, Meritxell Bach Cuadra 5,6, Ernst-Wilhelm Radue1, Jens Kuhle2, Ludwig Kappos2,
Sven Cichon3,7, and Cristina Granziera1,2
1Translational Imaging in Neurology Basel, Department of Medicine and Biomedical Engineering, University Hospital Basel and University of Basel, Basel, Switzerland, 2Neurologic Clinic and Policlinic, Switzerland, Departments of Medicine, Clinical Research and Biomedical Engineering, University Hospital Basel and University of Basel, Basel, Switzerland, 3Human Genomics Research Group, Department of Biomedicine, University Hospital and University of Basel, Basel, Switzerland, 4Department of Radiology, Weill Cornell Medical College, New York, NY, United States, 5Signal Processing Laboratory (LTS5), Ecole Polytechnique Fédérale de Lausanne (EPFL), Lausanne, Switzerland, 6Radiology Department, Center for Biomedical Imaging (CIBM), Lausanne University and University Hospital, Lausanne, Switzerland, 7Institute of Medical Genetics and Pathology, University Hospital Basel, Basel, Switzerland
Despite several large-scale genome-wide association studies (GWAS) have been performed in MS, to date no study explored the relationship between genetic risk factors for MS and the extent of myelin and axon damage in the brain of MS patients, as measured by advanced MRI techniques. Our results identify novel genetic loci that might be associated with myelin and axonal pathology in MS Patients.
|
||
3889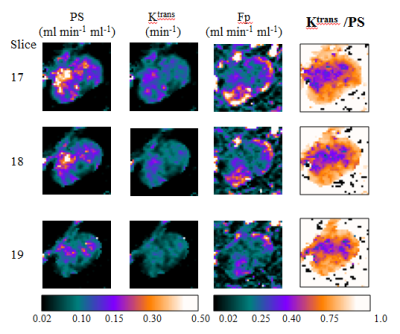 |
4 | High-spatial resolution mapping of microvascular permeability-surface area product using dual temporal resolution DCE-MRI techniques
Ka-Loh Li1, Daniel Lewis2, Xiaoping Zhu1, Alan Jackson1, and Timothy Cootes1
1Division of Informatics, Imaging and Data Sciences, University of Manchester, Manchester, United Kingdom, 2Department of Neurosurgery, Salford Royal NHS Foundation Trust,, Manchester, United Kingdom A limitation of the extended Tofts model (ETM) is that estimates of Ktrans, transfer constant, reflect both capillary plasma flow (Fp) and the capillary permeability-surface area product (PS). Other DCE-MRI models can separate out these physiological effects, but such models mandate high-temporal resolution data, compromising spatial resolution and volume coverage. In this in vivo brain tumor study, we demonstrate that incorporating the ETM and an early-timepoints absolute CBF (ET-CBF) method with a dual-temporal resolution, DCE-MRI approach, termed LEGATOS, permits generation of high-spatial resolution maps of Ktrans, Fp and PS, allowing high-spatial resolution interrogation of flow and permeability effects. |
||
 |
3890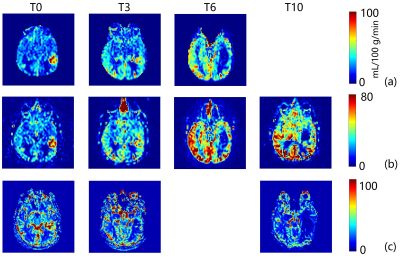 |
5 | Longitudinal Assessment of Tumor Perfusion in Glioblastoma using Arterial Spin Labeled MRI: Preliminary Findings
Yiming Wang1, Marco C. Pinho1,2, Limin Zhou1, Michael N. Youssef3,4, Joseph A. Maldjian1,2, and Ananth J. Madhuranthakam1,2
1Department of Radiology, UT Southwestern Medical Center, Dallas, TX, United States, 2Advanced Imaging Research Center, UT Southwestern Medical Center, Dallas, TX, United States, 3Department of Neurology, UT Southwestern Medical Center, Dallas, TX, United States, 4Harold C. Simmons Cancer Center, UT Southwestern Medical Center, Dallas, TX, United States
In Glioblastoma (GBM) patients undergoing chemoradiation, decreased tumor perfusion can be observed in treatment-responding patients and earlier than changes in tumor volume measured by conventional MRI. Such perfusion changes can be measured by non-contrast Arterial Spin Labeled (ASL) MRI, which is particularly suitable for longitudinal assessment of tumor perfusion. In this study, we performed longitudinal perfusion measurements using ASL MRI in patients with glioblastoma undergoing chemoradiation. Progressive perfusion reduction was observed in a representative patient's enhancing tumor ROIs along with increased ADC values, indicating reduced tumor cellularity, which likely results from treatment responses.
|
|
3891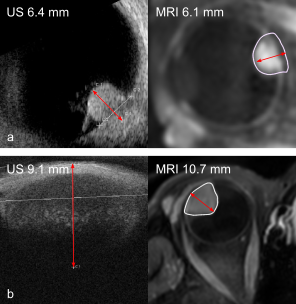 |
6 | 3D MRI versus conventional ultrasound tumour measurements for treatment planning of eye tumours
L. Klaassen1,2,3, M.G. Jaarsma-Coes1,2, T.A. Ferreira2, T.H.K. Vu1, M. Marinkovic1, G.P.M. Luyten1, C.R.N. Rasch3, and J.W.M. Beenakker1,2,3
1Ophthalmology, Leiden University Medical Center, Leiden, Netherlands, 2Radiology, Leiden University Medical Center, Leiden, Netherlands, 3Radiation Oncology, Leiden University Medical Center, Leiden, Netherlands
The aim of this study was to compare ultrasound and MRI dimension measurements for eye tumours and to determine the most suitable measurement modality. MRI and ultrasound yield similar prominence measurements (median absolute difference 0.3 mm) when tumour extent is visible on both modalities. However, in anteriorly located tumours, MRI measurements are more accurate, and using US for these tumours might lead to an underestimation of tumour diameter. MRI provided insight in 3D tumour geometry, even when tumour extent was difficult to visualize on US, enabling more accurate therapy planning and selection for uveal melanoma patients.
|
||
3892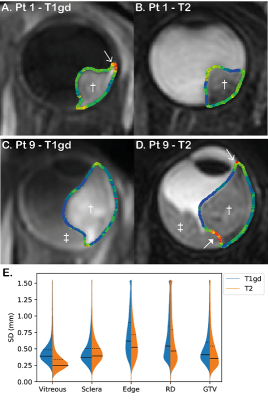 |
7 | Inter-observer variability in MR-based target volume delineation of uveal melanoma
L. Klaassen1,2,3, M.G. Jaarsma-Coes1,2, B.M. Verbist2, T.H.K. Vu1, Y.L.B. Klaver3,4, M.F. Rodrigues3,4, T.A. Ferreira2, C. Nabarro2, G.P.M. Luyten1, C.R.N. Rasch3,4, M. van Herk5, and J.W.M. Beenakker1,2,3
1Ophthalmology, Leiden University Medical Center, Leiden, Netherlands, 2Radiology, Leiden University Medical Center, Leiden, Netherlands, 3Radiation Oncology, Leiden University Medical Center, Leiden, Netherlands, 4Radiation Oncology, HollandPTC, Delft, Netherlands, 5Division of Cancer Sciences, University of Manchester, Manchester, United Kingdom
The aim of this study was to assess the inter-observer variation in gross target volume (GTV) delineation of uveal melanoma on MRI. Six observers delineated the GTV in ten different patients on T2-weighted and contrast-enhanced T1-weighted scans. The average interobserver variation appeared slightly higher on T1gd (0.41 mm) compared to T2 (0.35 mm), although the difference was not significant (p=0.12). We recommend to delineate based on the T1gd-weighted scans, as parts of the tumour might be missed on T2.
|
||
3893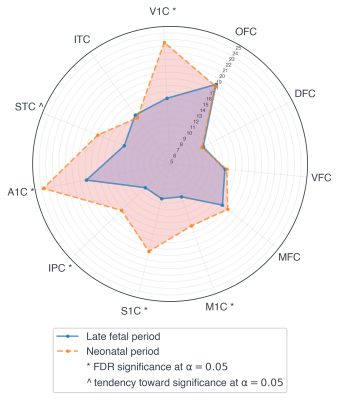 |
8 | Neural excitability through BOLD variability in the preterm brain: A longitudinal resting-state fMRI study
Serafeim Loukas1,2, Joana Sa de Almeida1, Djalel Eddine Meskaldji1,3, Dimitri Van De Ville2,4, and Petra Susan Hüppi1
1Division of Development and Growth, Department of Pediatrics, University of Geneva, Geneva, Switzerland, 2Institute of Bioengineering, École Polytechnique Fédérale de Lausanne (EPFL), Lausanne, Switzerland, 3Institute of Mathematics, École Polytechnique Fédérale de Lausanne (EPFL), Lausanne, Switzerland, 4Department of Radiology and Medical Informatics, University of Geneva, Geneva, Switzerland
Resting-state functional connectivity based on simultaneous BOLD oscillations has been described both in preterm infants and fullterm newborns. During this period of rapid cerebral cortex development, different brain activity patterns (networks) have been previously described. Regional changes in spontaneous BOLD signal variability on the other hand reflect local intravoxel BOLD changes related to neural excitability/flexibility. In the present study, we aimed to explore the longitudinal evolution of the BOLD variability between birth and term-equivalent-age (TEA), a period of rapid brain development, in preterm-born infants. Our findings suggest increased variability at TEA as compared to birth in important primary cortices.
|
||
3894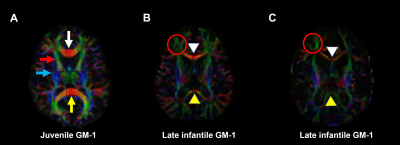 |
9 | Diffusion tensor imaging quantification of white matter tracts in internal capsule and corpus callosum of type II GM1 gangliosidosis patients
Mohammed Salman Shazeeb1, Zeynep Vardar1, Ahmet Peker1, Anna Kuhn1, Jean Johnston2, Precilla D'Souza2, Maria T. Acosta2, and Cynthia J. Tifft2
1University of Massachusetts Medical School, Worcester, MA, United States, 2National Institutes of Health, Bethesda, MD, United States
GM1-gangliosidosis is a rare heritable lysosomal storage disorder caused by accumulation of GM1-ganglioside due to deficiency of the lysosomal enzyme b-galactosidase required for sphingolipid degradation. Progressive accumulation of GM1-ganglioside in the central nervous system induces hypomyelination that results in progressive neurodegeneration. This study used quantitative diffusion tensor imaging (DTI) in 20 type II GM1 patients to assess white matter tract changes in the internal capsule and corpus callosum of juvenile and late infantile patients. Several DTI parameters showed significant differences between the patient groups and compared to healthy subjects that may be important to track the progression of the disease.
|
||
3895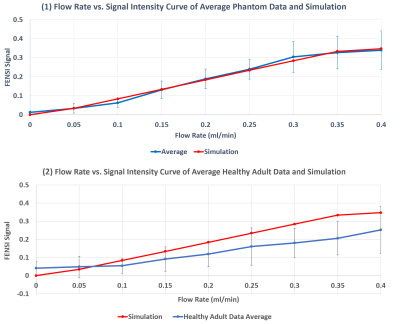 |
10 | Phase-Sweep Method and Fitting Analysis in Slow CSF Shunt Flow Measurement with PS-FENSI
Mingxiao Zhang1, Aaron Anderson2,3, Paul Arnold3, Jason Huston3, William C. Olivero2, and Bradley P. Sutton1,2
1Department of Bioengineering, University of Illinois, Urbana, IL, United States, 2Beckman Institute, Urbana, IL, United States, 3Carle Foundation Hospital, Urbana, IL, United States
Pediatric patients with hydrocephalus rely on ventriculo-peritoneal shunts to drain cerebrospinal fluid (CSF) from the brain. Quick, safe detection of shunt failure is crucial to preventing neurologic injury. Previously, a non-invasive MRI-based monitoring technique, Shunt Flow Enhancement of Signal Intensity (Shunt-FENSI), was proposed for accurate and quantitative CSF flow measurement in the slow flowing shunt. We are introducing a more advanced version, Phase-Sweep FENSI (PS-FENSI) to deal with magnetic field inhomogeneity which can cause changes to the tag effectiveness. This new method is accompanied by new fitting methods to more reliably measure FENSI signals.
|
||
3896 |
11 | Dynamic contrast-enhanced MRI reveals decreased pulmonary perfusion in COVID-19 Survivors
Iris Y. Zhou1,2, Michael C. Magaletta1, Molly Mascia2,3, George A. Alba2,3, Peter Caravan1,2, and Sydney B. Montesi2,3
1Athinoula A. Martinos Center for Biomedical Imaging, Institute for Innovation in Imaging, Department of Radiology, Massachusetts General Hospital, Boston, MA, United States, 2Harvard Medical School, Boston, MA, United States, 3Division of Pulmonary and Critical Care Medicine, Massachusetts General Hospital, Boston, MA, United States
Coronavirus disease 2019 (COVID-19) has been shown to cause pathologic aberrancies in the vascular endothelium. We performed dynamic contrast-enhanced (DCE) MRI on participants with prior COVID-19 to assess differences in pulmonary microvascular perfusion compared with healthy volunteers. Significantly reduced peak enhancement, slower rate of contrast arrival, and longer mean transit time were found in COVID-19 survivors compared to healthy controls, indicating reduced microvascular perfusion months after initial SARS-CoV-2 infection. The DCE MRI readouts can potentially be used as quantitative imaging biomarkers of pulmonary vascular change and may provide important insights into COVID-19 microvascular pathobiology and outcome.
|
||
3897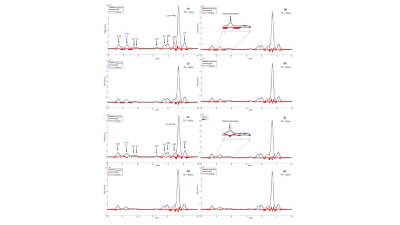 |
12 | Subcutaneous adipose tissue water fraction increases with weight loss in persons with obesity Video Permission Withheld
Jessie Han1, Mingming Wu1, Selina Rupp1, Daniela Junker1, Anna Reik2, Meike Wiechert2, Hans Hauner2,3, Marcus R. Makowski1, Christina Holzapfel2, Stefan Ruschke1, and Dimitrios C. Karampinos1
1Department of Diagnostic and Interventional Radiology, School of Medicine, Technical University of Munich, Munich, Germany, 2Institute for Nutritional Medicine, School of Medicine, Technical University of Munich, Munich, Germany, 3Else Kroener-Fresenius-Center of Nutritional Medicine, School of Life Sciences, Technical University of Munich, Freising, Germany
Subcutaneous adipose tissue (SAT) dysfunction is key in defining high-risk individuals in obesity. A change in adipose tissue water fraction with weight loss may reflect improvement in blood flow or changes in microstructure of adipose tissue. Single-voxel STEAM Magnetic Resonance Spectroscopy (MRS) and chemical shift encoded-based water-fat separation are non-invasive methods to assess the water fraction and proton density fat fraction (PDFF) of adipose tissue. The present work aims to investigate the feasibility of MRS and water-fat separation to quantify PDFF and evaluate the changes in SAT water fraction in persons with obesity undergoing an 8-week weight loss intervention.
|
||
The International Society for Magnetic Resonance in Medicine is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians.