Oral Session
Pulmonary: Inhale the Present, Exhale the Past
Joint Annual Meeting ISMRM-ESMRMB & ISMRT 31st Annual Meeting • 07-12 May 2022 • London, UK

14:45 |
0658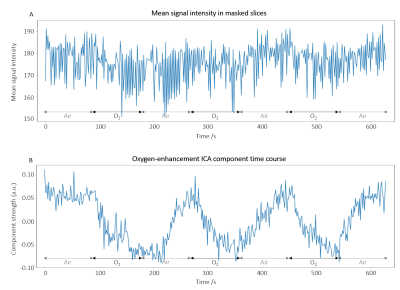 |
Functional Lung MRI at 3.0 T using Oxygen-Enhanced MRI (OE-MRI) and Independent Component Analysis (ICA)
Sarah H. Needleman1, Mina Kim1, Jamie R. McClelland1, Marta Tibiletti2, Josephine H. Naish2,3, James P. B. O'Connor4, and Geoff J. M. Parker1,2
1Centre for Medical Image Computing (CMIC), University College London, London, United Kingdom, 2Bioxydyn Limited, Manchester, United Kingdom, 3MCMR, Manchester University NHS Foundation Trust, Manchester, United Kingdom, 4Division of Radiotherapy and Imaging, Institute of Cancer Research, London, United Kingdom Analysis of dynamic lung OE-MRI is challenging due to the presence of substantial artefacts and poor SNR, particularly at 3 T. We propose a cyclical oxygen delivery scheme and ICA to separate the oxygen-enhancement signal from these confounding factors at 3 T. The proposed method extracts a well-defined oxygen-enhancement signal that removes confounds due to proton density changes, blood flow and motion. We also demonstrate the ability to resolve the opposite enhancement effects of the parenchymal and vascular OE-MRI signals to provide information on pulmonary vasculature and gas distribution. The method is shown to be sensitive to smoking status. |
|
| 14:57 | 0659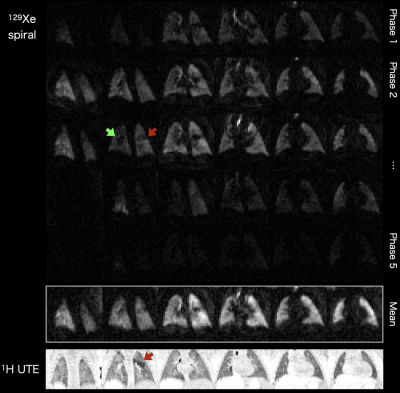 |
Hyperpolarized 129Xe MR Imaging in Neonates with Bronchopulmonary Dysplasia: Feasibility and Challenges
Neil J Stewart1,2, Nara Higano2,3,4,5, Shanmukha Sai Mukthapuram3,6, Matthew M Willmering2,3, Anita Arnsperger7, Ronald Pratt4, Wolfgang Loew4, Madhwesha R Rao1, Rolf F Schulte8, Jim M Wild1, and Jason C Woods2,3,4,5
1POLARIS, Imaging Sciences, Department of Infection, Immunity & Cardiovascular Disease, The University of Sheffield, Sheffield, United Kingdom, 2Center for Pulmonary Imaging Research, Cincinnati Children’s Hospital Medical Center, Cincinnati, OH, United States, 3Division of Pulmonary Medicine, Cincinnati Children’s Hospital Medical Center, Cincinnati, OH, United States, 4Department of Radiology, Cincinnati Children’s Hospital Medical Center, Cincinnati, OH, United States, 5Department of Pediatrics, College of Medicine, University of Cincinnati, Cincinnati, OH, United States, 6The Perinatal Institute, Section of Neonatology, Perinatal and Pulmonary Biology, Cincinnati Children’s Hospital Medical Center, Cincinnati, OH, United States, 7Division of Respiratory Care, Cincinnati Children’s Hospital Medical Center, Cincinnati, OH, United States, 8GE Healthcare, Munich, Germany We report the first-ever experience in performing HP 129Xe MRI in neonates. The neonates had prematurity-related lung disease (bronchopulmonary dysplasia), a major cause of morbidity/mortality that remains poorly characterised. The feasibility of imaging during a short (<3s) breath-hold apnea was demonstrated. Spiral-based 129Xe ventilation imaging showed good image quality (SNR>20) and sufficient sensitivity to detect mild ventilation abnormalities. Dynamic 129Xe spectroscopy revealed the existence of resonances near the conventional tissue/plasma and red blood cells resonances observed in children and adults. With further data, our work may impact on the management of infant lung diseases in the neonatal period and beyond. |
|
| 15:09 | 0660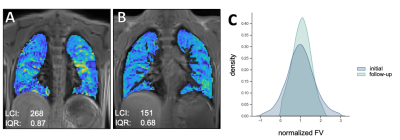 |
Functional 3D-UTE MRI of the Lungs for Monitoring Ventilation Inhomogeneity in Patients with Cystic Fibrosis on Treatment with CFTR Modulators
Julius Heidenreich1, Philipp Josef Kuhl1, Corona Metz1, Andreas Max Weng1, Jan-Peter Grunz1, Thomas Benkert2, Helge Hebestreit3, Thorsten Alexander Bley1, Herbert Köstler1, and Simon Veldhoen1
1Department of Diagnostic and Interventional Radiology, University Hospital Würzburg, Würzburg, Germany, 2Siemens Healthineers GmbH, Erlangen, Germany, 3Department of Pediatrics, University Hospital Würzburg, Würzburg, Germany
Single breath-hold 3D-UTE-MRI was proposed for simultaneous evaluation of lung morphology and function. Sixteen patients with cystic fibrosis (CF) underwent initial and follow-up 3D-UTE-MRI in 2019 and 2021. In line with a previous study, referenced voxelwise fractional ventilation (FV) provided a marker that correlates strongly with the lung clearance index (LCI), reflecting ventilation inhomogeneity. Seven patients received a new drug-combination (ivacaftor/elexacaftor/tezacaftor) with significantly improved lung function during clinical follow-up. Similarly, significantly decreased ventilation inhomogeneity was derived from functional MRI. Thus, single breath-hold 3D-UTE MRI is a valuable tool for monitoring ventilation inhomogeneity in patients with CF during drug treatment.
|
|
| 15:21 | 0661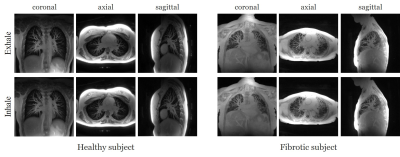 |
High-resolution dynamic 3D UTE Lung MRI using motion-compensated manifold learning
Qing Zou1, Luis A. Torres2, Sean B. Fain1, and Mathews Jacob1
1University of Iowa, Iowa City, IA, United States, 2University of Wisconsin–Madison, Madison, WI, United States
UTE radial MRI methods are powerful tools for probing lung structure and function. However, the challenge in directly using this scheme for high-resolution lung imaging applications is the long breath-hold needed. While self-gating approaches that bin the data to different respiratory phases are promising, they do not allow the functional imaging of the lung and are often sensitive to bulk motion. The main focus of this work is to introduce a novel motion compensated manifold learning framework for functional and structural lung imaging. The proposed scheme is robust to bulk motion and enables high-resolution lung imaging in around 4 minutes.
|
|
| 15:33 | 0662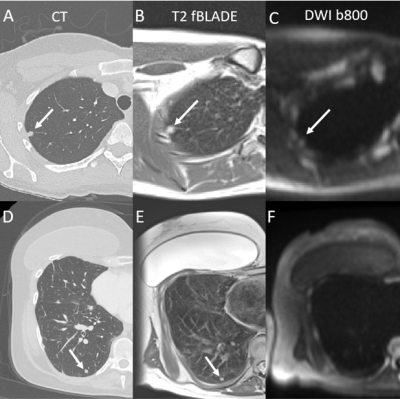 |
Lung nodule imaging using high-performance 0.55T MRI
Björn Wieslander1, Ahsan Javed2, Rajiv Ramasawmy2, Ashkan A Malayeri3, Scott Baute2, Kendall J O'Brien2, Christine Mancini2, Amanda Potersnak2, Cheryl Warga4, Joel Moss1, Marcus Y Chen2, and Adrienne E Campbell-Washburn2
1Pulmonary Branch, Division of Intramural Research, National Heart, Lung and Blood Institute, National Institutes of Health, Bethesda, MD, United States, 2Cardiovascular Branch, Division of Intramural Research, National Heart, Lung, and Blood Institute, National Institutes of Health, Bethesda, MD, United States, 3Radiology and Imaging Sciences, Clinical Center, National Institutes of Health, Bethesda, MD, United States, 4National Cancer Institute, National Institutes of Health, Bethesda, MD, United States
Lung imaging plays an important role in routine screening for lung nodules and lung cancer. Magnetic resonance imaging (MRI) has recently emerged as an alternative to computed tomography (CT) to image lung nodules. Lower field MRI offers high image quality, due to improved field homogeneity, and lower cost. We imaged 11 patients who had a total of 29 nodules visible on clinically motivated CT scans. T2-weighted images showed good agreement with CT in terms of nodule size and diameters and malignant nodules were more often visible on diffusion weighted images (b = 800).
|
|
| 15:45 | 0663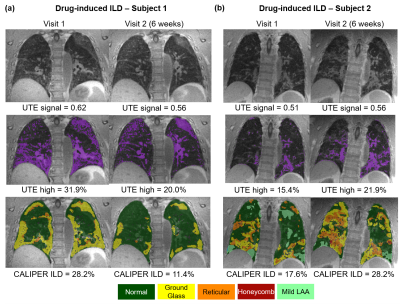 |
Longitudinal comparison of quantitative UTE lung MRI and CT biomarkers in interstitial lung disease
Ho-Fung Chan1, Timothy J Baldwin1, Harry Barker1, Neil J Stewart1, James A Eaden1,2, Paul J.C Hughes1, Nicholas D Weatherley1, Joshua Astley1,3, Bilal A Tahir1,3, Kevin M Johnson4, Ronald A Karwoski5, Brian J Bartholmai6, Marta Tibiletti7, Colm T Leonard8,9, Sarah Skeoch8,10, Nazia Chaudhuri8,9, Ian N Bruce8,9, Geoff J.M Parker7,11, Stephen M Bianchi2, and Jim M Wild1
1Infection, Immunity and Cardiovascular Disease, University of Sheffield, Sheffield, United Kingdom, 2Academic Directorate of Respiratory Medicine, Sheffield Teaching Hospitals NHS Foundation Trust, Sheffield, United Kingdom, 3Oncology and Metabolism, University of Sheffield, Sheffield, United Kingdom, 4Radiology and Medical Physics, University of Wisconsin, Madison, WI, United States, 5Biomedical Imaging Resource, Mayo Clinic, Rochester, MN, United States, 6Radiology, Mayo Clinic, Rochester, MN, United States, 7Bioxydyn Limited, Manchester, United Kingdom, 8University of Manchester, Manchester, United Kingdom, 9Manchester University NHS Foundation Trust, Manchester, United Kingdom, 10Royal United Hospitals Bath NHS Foundation Trust, Bath, United Kingdom, 11Centre for Medical Image Computing, University College London, London, United Kingdom
UTE lung MRI approaches the diagnostic quality of CT, opening up the possibility for longitudinal follow-up of interstitial lung disease (ILD) progression. Two quantitative biomarkers of UTE lung signal were developed for monitoring longitudinal change in ILD and benchmarked against quantitative CT CALIPER measurements. Normalized UTE lung signal and UTE high percentage (based on 95% cutoff of healthy UTE lung values) was significantly different between nine healthy volunteers and sixteen ILD patients. Longitudinal change in UTE biomarkers correlated with change in CT CALIPER ILD% in the ILD patients, and most-strongly correlated to CT ground-glass changes in the lung parenchyma.
|
|
| 15:57 | 0664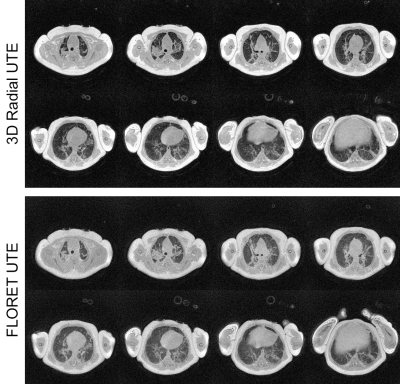 |
Improving Efficiency of Ultra-short Echo Time MRI in Neonatal Lungs with a FLORET Spiral Trajectory
Andrew D Hahn1,2, Nara S Higano3,4,5, Matthew M Willmering3,4,6, Neil J Stewart6,7, Jason C Woods3,4,5,6,8,9, and Sean B Fain1,2
1Department of Radiology, University of Iowa, Iowa City, IA, United States, 2Department of Medical Physics, University of Wisconsin, Madison, Madison, WI, United States, 3Division of Pulmonary Medicine, Cincinnati Children's Hospital, Cincinnati, OH, United States, 4Department of Radiology, Cincinnati Children's Hospital, Cincinnati, OH, United States, 5Department of Pediatrics, University of Cincinnati, Cincinnati, OH, United States, 6Center for Pulmonary Imaging Research, Cincinnati Children's Hospital, Cincinnati, OH, United States, 7POLARIS, Imaging Sciences, Department of Infection, Immunity and Cardiovascular Disease, University of Sheffield, Sheffield, United Kingdom, 8Department of Radiology, University of Cincinnati, Cincinnati, OH, United States, 9Department of Physics, University of Cincinnati, Cincinnati, OH, United States
State-of-the-art structural pulmonary MRI of neonatal intensive care unit patients has previously been performed using 3D radial UTE. Performance is high yet scan times can be 15 minutes or more due to the low sampling efficiency of radial trajectories. Here we explore FLORET UTE in this application and demonstrate comparable image quality to the state-of-the-art in approximately 25% of the scan time. Lung parenchymal SNR is maintained, and the spiral trajectory provides a higher parenchymal signal relative to muscle. Shorter scan times reduce the opportunity for bulk motion and risk to this sensitive population.
|
|
| 16:09 | 0665 |
Imaging lung water redistribution using 0.55T ultrashort echo time MRI
Felicia Seemann1, Ahsan Javed1, Rachel Chae1, Amanda Potersnak1, Scott Baute1, Kendall O’Brien1, Rajiv Ramasawmy1, Robert J Lederman1, and Adrienne E Campbell-Washburn1
1Cardiovascular Branch, National Heart, Lung, and Blood Institute, National Institutes of Health, Bethesda, MD, United States
Quantification of changes in lung water using MRI may provide clinical value in early diagnosis of heart failure. In this study, we demonstrate the ability of our 3D free-breathing spiral ultrashort-TE sequence to quantify and capture changes in lung water using a high-performance 0.55T MRI system. A phantom containing mixtures of water and deuterium oxide at varying concentrations was used to validate water density quantification. Our proposed approach captured the gravity-induced redistribution of lung water, achieved by imaging subjects in the supine and prone positions.
|
The International Society for Magnetic Resonance in Medicine is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians.