Oral Session
Stroke & Ischemia: Bench to Bedside
Joint Annual Meeting ISMRM-ESMRMB & ISMRT 31st Annual Meeting • 07-12 May 2022 • London, UK

17:00 |
0140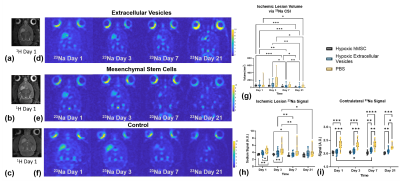 |
Mechanism of recovery following stem cell therapy in ischemic stroke: cell or secretome?
Shannon Helsper1,2, Xuegang Yuan3, Richard Jeske2, Li Sun4, David G. Meckes Jr.4, Yan Li2, and Samuel C. Grant1,2
1National High Magnetic Field Laboratory, Florida State University, Tallahassee, FL, United States, 2Chemical & Biomedical Engineering, FAMU-FSU College of Engineering, Tallahassee, FL, United States, 3University of California, Los Angeles, CA, United States, 4Department of Biomedical Sciences, Florida State University, Tallahassee, FL, United States
This study interrogates human mesenchymal stem cell (hMSC) derived treatments (cells versus secretome) in a preclinical transient ischemic stroke model. Biochemical markers of tissue recovery measured longitudinally over 21 d via sodium chemical shift imaging and proton relaxation-enhanced MR spectroscopy demonstrated that the arterial injection of extracellular vesicles produced in vitro by hMSC improved outcomes over ischemic stroke, albeit not to the level of direct cellular implantation. For the first time, novel MRI-compatible labeling provided the initial visualization of biodistribution and estimated permanence of hMSC-derived extracellular vesicles in the ischemic brain.
|
|
| 17:12 | 0141 |
Cortical thickness at 3 years post-ischemic stroke: seeking vascular imaging signatures
Mohamed Salah Khlif1, Emilio Werden1, Laura Bird2, Natalia Brumley-Egorova1, and Amy Brodtmann1
1The Florey Institute of Neuroscience and Mental Health, Parkville, Australia, 2Turner Institute for Brain and Mental Health, Monash University, Clayton, Australia
Cortical thinning has been used both for diagnosis and disease monitoring. Few studies have examined longitudinal changes in cortical thickness following ischemic stroke. We compared cortical thinning, vortex-wise and region-wise, between ischemic stroke survivors and stroke-free control participants at 3 months and 3 years post-stroke using linear mixed-effect regression and correcting for age and sex. At 3 years, there was widespread cortical thinning in ischemic stroke, especially in the ipsilesional cortex, in lobes implicated in motor, sensory, and memory processing and recovery.
|
|
| 17:24 | 0142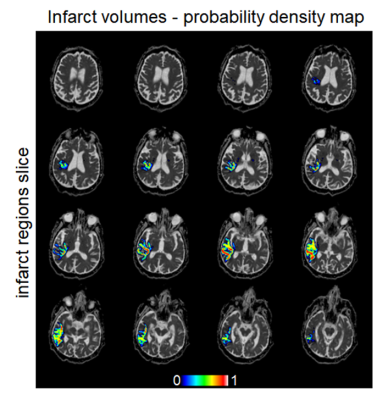 |
Acute Ischemic Stroke: Infarct Core Estimation from Threshold-based DWI Delineation Depends on the DWI protocol Video Not Available
Jonathan Rafael-Patiño1,2, Elda Fischi-Gomez1, Sebastian Otálora3, Veronica Ravano1,2,4, Guillaume Saliou1, Steven David Hajdu1, Tobias Kober1,2,4, Roland Wiest3, Patrik Michel5, Richard McKinley3, and Jonas Richiardi1
1Radiology Department, Centre Hospitalier Universitaire Vaudois and University of Lausanne., Lausanne, Switzerland, 2LTS5, École Polytechnique Fédérale de Lausanne (EPFL), Lausanne, Switzerland, 3Support Center for Advanced Neuroimaging (SCAN), University Institute of Diagnostic and Interventional Neuroradiology, University of Bern, Inselspital, Bern University Hospital., Bern, Switzerland, 4Advanced Clinical Imaging Technology, Siemens Healthcare AG., Lausanne, Switzerland, 5Stoke Center, Neurology Service, Lausanne University Hospital and University of Lausanne, Lausanne, Switzerland
In acute stroke assessment, reference clinical trials such as DEFUSE-3 use absolute thresholds on ADC maps to define the infarct core. Yet, the variance of ADC values, but not the mean, change with the number of diffusion directions and the specific directions in a 4-directions sampling scheme. The resulting shifts in ADC distribution tails result in an overestimation of the infarct core. This has implications for multi-centric trials, where infarct sizes and locations may be biased simply due to diffusion protocol differences and/or different head positions with respect to B0.
|
|
| 17:36 | 0143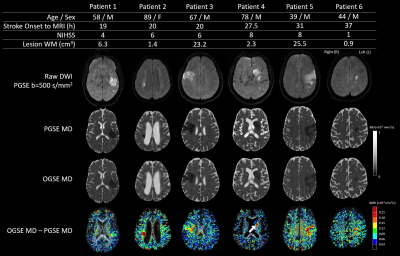 |
Heterogeneous diffusivity changes within human stroke lesions measured with oscillating gradient spin echo diffusion MRI
Mi Zhou1, Robert Stobbe1, Brian Buck2, Ken Butcher2, Paige Fairall2, Annie Boyd1, Derek Emery3, Thorsten Feiweier4, and Christian Beaulieu1
1Biomedical Engineering, University of Alberta, Edmonton, AB, Canada, 2Neurology, University of Alberta, Edmonton, AB, Canada, 3Radiology and Diagnostic Imaging, University of Alberta, Edmonton, AB, Canada, 4Siemens Healthcare GmbH, Erlangen, Germany Short diffusion time oscillating gradient spin echo (OGSE) showed less water diffusion reduction in acute human stroke lesions (n=28) than the typical clinically used long diffusion time pulsed gradient spin echo (PGSE) method. The diffusion time dependency is far greater in ischemic lesions, particularly white matter, than in contralateral healthy brain. These effects were heterogeneous across the lesion with larger OGSE-PGSE differences in regions indicative of larger axons. The range of MD decrease in lesions across patients as measured with OGSE and PGSE showed a linear correlation and is consistent with concomitant axon beading and swelling implied from prior simulations. |
|
| 17:48 | 0144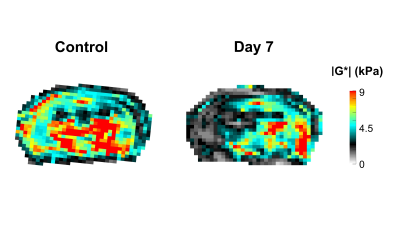 |
Sensing brain plasticity after stroke using magnetic resonance elastography
Giacomo Annio1,2, Gabrielle Mangin1, Marco Barbero-Mota1, Giuseppina Caligiuri1, Antonino Nicoletti1, Katharina Schregel3, and Ralph Sinkus1,4
1INSERM UMRS1148 - Laboratory for Vascular Translational Science, University Paris, Paris, France, 2School of Biomedical Engineering and Imaging Sciences, King’s College London, London, United Kingdom, 3Department of Neuroradiology, Heidelberg University Hospital, Heidelberg, Germany, 4School of Biomedical Engineering and Imaging Sciences, King's College London, London, United Kingdom
Stroke is the leading cause of death globally. The infarcted area undergoes a deprivation of oxygen and energy, followed by multiple transient events and reorganization processes called ischemic cascade. MRI is the reference tool for accurate diagnosis, volumetric assessments and age determination of the lesion. The aim of the present study was to investigate the time course of changes in tissue biomechanics after an ischemic event in mice using MRE and study the relationship between stroke volume and tissue biomechanics, to explore a potential role of MRE in assessing the post stroke recovery.
|
The International Society for Magnetic Resonance in Medicine is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians.