Oral Session
Muscle
Joint Annual Meeting ISMRM-ESMRMB & ISMRT 31st Annual Meeting • 07-12 May 2022 • London, UK

14:45 |
0666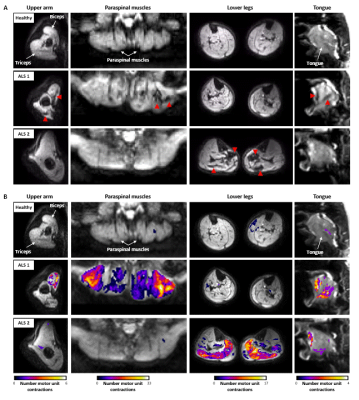 |
Whole-body fasciculation detection in Amyotrophic Lateral Sclerosis (ALS) using motor unit MRI (MUMRI)
Linda Heskamp1, Matthew G. Birkbeck1,2,3, Julie Hall1,4, Ian S. Schofield1, Hugo de Oliveira5, Timothy L. Williams5, Roger G. Whittaker1, and Andrew M. Blamire1
1Newcastle University Translational and Clinical Research Institute, Newcastle University, Newcastle upon Tyne, United Kingdom, 2Newcastle Biomedical Research Centre, Newcastle University, Newcastle upon Tyne, United Kingdom, 3Northern Medical Physics and Clinical Engineering, Freeman Hospital, Freeman Hospital, Newcastle upon Tyne NHS Foundation Trust, Newcastle upon Tune, United Kingdom, 4Department of Neuroradiology, Royal Victoria Infirmary, Newcastle upon Tyne, United Kingdom, 5Directorate of Clinical Neurosciences, Royal Victoria Infirmary, Newcastle upon Tyne, United Kingdom
The spontaneous contraction of motor units in muscle, i.e. fasciculation, has been recognised as an important diagnostic marker in amyotrophic lateral sclerosis (ALS). Fasciculation can be imaged with a novel MRI technique called motor unit MRI. This technique uses a diffusion weighted sequence on which fasciculation presents as short-living signal voids. We demonstrated an increased fasciculation rate in ALS patients compared to healthy controls by assessing the four body regions relevant in the diagnosis of ALS. The affected body regions differed between patients. This is in line with the heterogeneous disease onset and supports our proposed whole-body approach.
|
|
| 14:57 | 0667 |
Age-related changes in human skeletal muscle microstructure and architecture assessed by DT-MRI and their association with muscle strength
Donnie Cameron1,2, David A. Reiter3, Fatemeh Adelnia4, Ceereena Ubaida-Mohien5, Christopher M. Bergeron6, Seongjin Choi7, Kenneth W. Fishbein6, Richard G. Spencer6, and Luigi Ferrucci5
1Norwich Medical School, University of East Anglia, Norwich, United Kingdom, 2Department of Radiology, Leiden University Medical Center, Leiden, Netherlands, 3Emory University School of Medicine, Atlanta, GA, United States, 4Vanderbilt University Institute of Imaging Science, Vanderbilt University, Nashville, TN, United States, 5Translational Gerontology Branch, National Institute on Aging, National Institutes of Health, Baltimore, MD, United States, 6Laboratory of Clinical Investigation, National Institute on Aging, National Institutes of Health, Baltimore, MD, United States, 7Department of Neurology, University of Maryland School of Medicine, Baltimore, MD, United States
Here we apply diffusion-tensor-(DT)-MRI to study muscle microstructural and architectural changes with healthy ageing in 94 participants (median age=56, range=22-89yrs). Fractional anisotropy (FA) and mean diffusivity (MD), were calculated for 12 thigh muscles, as were pennation angle, fascicle length, fibre curvature, and physiological cross-sectional area (PCSA) for the rectus femoris and biceps femoris longus. Knee extension/flexion torques were also measured. FA and MD were significantly associated with age (β=0.34 and −0.34, p<0.05), as were architecture parameters. Pennation angle and PCSA were positively associated with strength. This may prove useful for studying muscle response to interventions designed to delay sarcopenia.
|
|
| 15:09 | 0668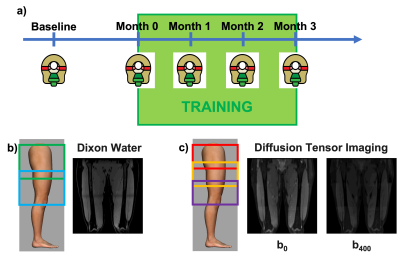 |
Muscle hypertrophy in resistance training assessed with Diffusion Tensor Imaging Video Permission Withheld
Valentina Mazzoli1, Elka Rubin 1, Marco Barbieri1, Andrew Schmidt1, Lauren Watkins1, Akshay Chaudhary1, Feliks Kogan1, and Garry Gold1
1Department of Radiology, Stanford University, Stanford, CA, United States
5 healthy subjects consistently performed a declined squad training routine for 3 months. Every subject received an MRI scan before undergoing the training and subsequently every month until the end of the training. We observed a decrease in AD, MD and FA over the course of training, with a significant change after 1 month. Muscle volume increased, with changes only apparent at 3 months. Changes in diffusion parameters were predictive of changes in global volume. Our study shows that DTI can be a sensitive tool to study muscle hypertrophy and could be used for early monitoring of training and rehabilitation.
|
|
| 15:21 | 0669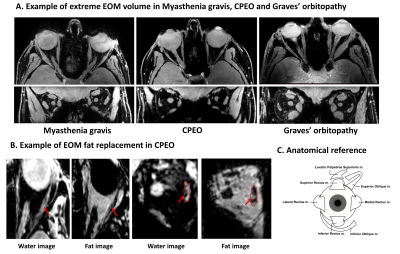 |
Extra-ocular muscle volume, T2water and fat fraction are slightly increased in patients with myasthenia gravis
Kevin R. Keene1,2, Jan J.G.M. Verschuuren1, Irene C. Notting3, Martijn R. Tannemaat1, Jan-Willem M. Beenakker2,3, and Hermien E. Kan2
1Department of Neurology, Leiden University Medical Center, Leiden, Netherlands, 2C.J. Gorter Center of High Field MRI, Department of Radiology, Leiden University Medical Center, Leiden, Netherlands, 3Department of Opthalmology, Leiden University Medical Center, Leiden, Netherlands
Quantitative MRI of the extra-ocular muscles might have diagnostic value and play a role in therapeutic monitoring in myasthenia gravis (MG). Our data show a slight increase in volume, fat fraction and T2water in extra-ocular muscles of MG patients compared to controls. Volume and fat fraction changes were most pronounced in chronic MG patients, T2water changes were most pronounced in recently diagnosed and untreated MG patients. The absence of gross structural changes implies that eye muscle weakness might be reversible, even in chronic patients with residual ophthalmoplegia.
|
|
| 15:33 | 0670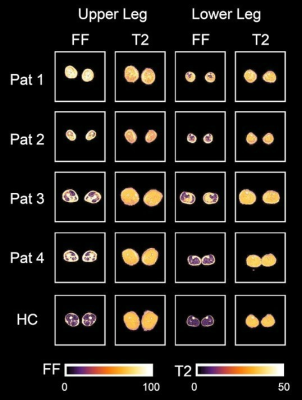 |
Evaluating correlations of quantitative muscle MRI of leg muscles and clinical outcome measurements in patients with LGMD2A
Lara Schlaffke1, Marlena Rohm1, Robert Rehmann1,2, Anne-Katrin Güttsches1, Martijn Froeling3, Matthias Vorgerd1, and Johannes Forsting1
1Neurology, University Clinic Bergmannsheil Bochum gGmbH, Bochum, Germany, 2Neurology, Klinikum Dortmund, University Witten-Herdecke, Dortmund, Germany, 3Radiology, UMC Utrecht, Utrecht, Netherlands
Quantitative MRI (qMRI) techniques like Dixon fat-fraction (FF) and quantitative water-T2 relaxation time (T2) are promising non-invasive tools in the evaluation of neuromuscular diseases like LGMD2A. In this study, we were able to show moderate to strong correlations between quantitative MRI values, especially FF, with clinical outcome measures and daily life activities. Analysis of T2 relaxation time in non-fat-infiltrated leg muscles of LGMD2A patients showed a significantly higher water T2 values compared to healthy controls. Therefore, T2 relaxation times may offer an earlier detection of disease-related change of muscular tissue in limb girdle muscular dystrophy compared to irreversible fat-fractions.
|
|
15:45 |
0671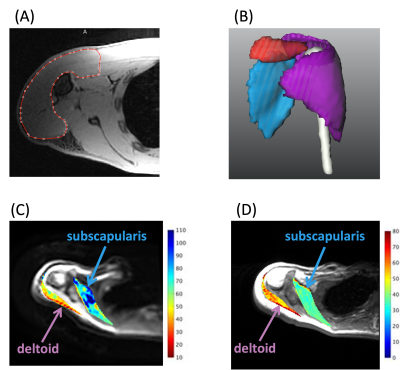 |
Quantitative MRI Analysis of Muscle Denervation
Tim Yiran Li1, Erin Argentieri2, Emily Pedrick2, Darryl B. Sneag2, and Ek T. Tan2
1Weill Cornell Medical College, New York, NY, United States, 2Hospital for Special Surgery, New York, NY, United States
Macroscopic muscle volume evaluation and quantitative MRI of diffusion microstructure may provide objective, longitudinal assessment of muscle denervation. Analysis of subjects with Parsonage-Turner syndrome (neuralgic amyotrophy) showed both reduced muscle volume and reduced muscle diameter. Macroscopic muscle volume demonstrated a strong positive correlation with microscopic diffusion-based muscle diameter, and a strong negative correlation with T2-mapping. Denervated muscles exhibited longitudinal changes in quantitative MRI metrics, whereas non-denervated (control) muscles showed minimal quantitative changes.
|
|
| 15:57 | 0672 |
Strain rates along the fiber are heterogeneously distributed over the length of lower leg muscles during dynamic exercise Video Permission Withheld
Melissa Tamara Hooijmans1, Thom T.J. Veeger2, Valentina Mazzoli3, Hans C. van Assen4, Lukas M. Gottwald1, Aart J. Nederveen1, Jurriaan H. de Groot5, Gustav J. Strijkers6, and Hermien E. Kan2,7
1Radiology and Nuclear Medicine, Amsterdam University Medical Centers, Amsterdam Movement Sciences, Amsterdam, Netherlands, 2C.J. Gorter Center for High Field MRI, Department of Radiology, Leiden University Medical Center, Leiden, Netherlands, 3Department of Radiology, Stanford University, Stanford, CA, United States, 4Department of Radiology, Leiden University Medical Center, Leiden, Netherlands, 5Department of Rehabilitation Medicine, Leiden University Medical Center, Leiden, Netherlands, 6Department of Biomedical Engineering and Physics, Amsterdam Movement Sciences, Amsterdam University Medical Center, Amsterdam, Netherlands, 7Duchenne Center Netherlands, Leiden, Netherlands
In this study we assessed strain rates along and close to perpendicular to the fiber in the lower-leg muscles, by combining 3D phase contrast with DTI-derived fiber orientations, during dynamic exercise with and without load. Our data revealed spatially heterogeneous strain rate patterns along the fiber within lower-leg muscles, with smallest and largest strain rates in the most proximal and distal segments of the Gastrocnemii muscles, respectively, and opposed (expansion and contraction) strain rate patterns between some of the Tibialis Anterior (TA) muscle compartments. Additional loading resulted in higher strain rates in TA compartments but lower in the Gastrocnemii muscles.
|
|
| 16:09 | 0673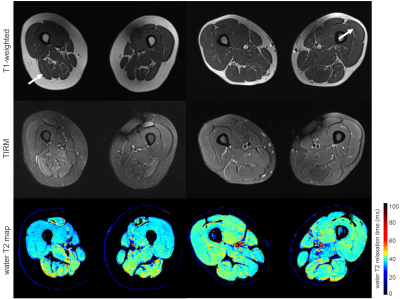 |
The value of water T2 relaxation time in the early detection of neuromuscular diseases: a retrospective biopsy-controlled analysis in 83 patients
Fabian Balsiger1, Noah Locher2, Benedikt Wagner1, and Olivier Scheidegger1,2
1Support Center for Advanced Neuroimaging (SCAN), Institute for Diagnostic and Interventional Neuroradiology, Inselspital, Bern University Hospital, University of Bern, Bern, Switzerland, 2Centre for Neuromuscular Diseases, Department of Neurology, Inselspital, Bern University Hospital, University of Bern, Bern, Switzerland
The diagnostic ability of quantitative water T2 mapping using multi-slice multi-echo sequences for the early detection of neuromuscular diseases (NMDs) was compared to fat-suppressed T2-weighted turbo inversion recovery magnitude (TIRM) MRI. Water T2 mapping had a significantly higher sensitivity and diagnostic ability in detecting muscle abnormalities than the subjective grading of TIRM MRI, prior to late-stage fatty infiltration signal alternations in T1-weighted MRI. Normal appearing TIRM MRI does not rule out disease activity in muscles in NMDs. Our findings suggest considering water T2 mapping over TIRM MRI for early detection of NMDs in clinical practice.
|
The International Society for Magnetic Resonance in Medicine is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians.