Oral Session
COVID-19: Latest MRI Findings & Applications
Joint Annual Meeting ISMRM-ESMRMB & ISMRT 31st Annual Meeting • 07-12 May 2022 • London, UK

| 17:00 | 0730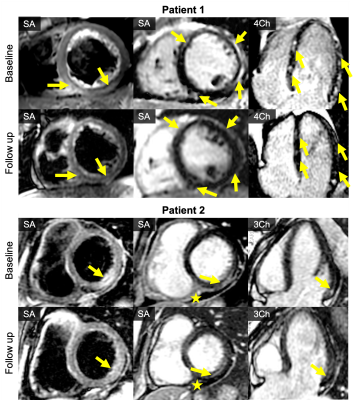 |
Myocarditis associated with mRNA COVID-19 vaccines: MRI findings
Jitka Starekova1, David A Bluemke1,2, William S Bradham1,3, Thomas M Grist1,2,4, Mark L Schiebler1, and Scott B Reeder1,2,3,4,5
1Radiology, University of Wisconsin-Madison, Madison, WI, United States, 2Medical Physics, University of Wisconsin-Madison, Madison, WI, United States, 3Medicine, University of Wisconsin-Madison, Madison, WI, United States, 4Biomedical Engineering, University of Wisconsin-Madison, Madison, WI, United States, 5Emergency Medicine, University of Wisconsin-Madison, Madison, WI, United States Mass immunization campaigns continue in attempts to contain the ongoing COVID-19 pandemic. COVID-19 vaccines authorized for use in the United States include BNT162b2 (Pfizer-BioNTech), mRNA-1273 (Moderna), and JNJ-78436735 (Johnson & Johnson). To date multiple cases of vaccine-associated inflammation of the heart have been reported. In this work, we describe cardiac MRI findings in 9 patients (adults and children) with clinical and imaging-based diagnosis of myocarditis and/or pericarditis diagnosed shortly after COVID-19 mRNA vaccination at our institution.
|
|
| 17:12 | 0731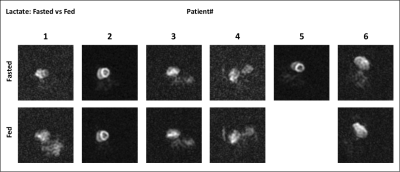 |
Myocardial Metabolic Changes Detected Post-COVID-19 with Hyperpolarized Pyruvate
Vlad G Zaha1, Junjie Ma1, Jae Mo Park1, Munes Fares1, Nicholas Hendren1, Spencer Carter1, Anjali Rao1, Ravi Vamsee1, Madhusudan Ganigara1, Mohamed Nagiub1, Mohammad Tarique Hussain1, Ricardo La Hoz1, James Cutrell1, Pradeep Mammen1, Mark Drazner1, James de Lemos1, Craig Malloy1, and Justin Grodin1
1University of Texas Southwestern Medical Center, Dallas, TX, United States
Noninvasive detection of myocardial inflammation can be challenging. Up to 73% of patients recovered from COVID-19 had increased native T1 on cardiac MRI1 representing inflammation or edema. Therefore, we tested whether hyperpolarized (HP) [1-13C]pyruvate detectis post-COVID-19 inflammation in the myocardium. HP [1-13C]lactate has been suggested as a surrogate imaging marker of inflammation in the heart2,3, attributed to increased glycolytic activity in infiltrating white cells plus a possible increase in activity of lactate dehydrogenase. We demonstrate the feasibility of imaging with HP [1-13C]pyruvate as noninvasive method to detect metabolic changes that may identify cardiac inflammation in the convalescent stage after COVID-19.
|
|
| 17:24 | 0732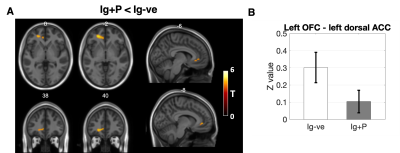 |
Persistent anosmia following COVID-19 results in significant connectivity differences within olfactory regions: a resting state fMRI analysis
Jed Wingrove1,2, Janine Makaronidis1,2, Ferran Prados2,3,4, Baris Kanber2,3,4, Marios C Yiannakas3, Gloria Castellazzi3,5,6, Claudia AM Gandini Wheeler-Kingshott3,7,8, and Rachel Batterham1,2
1Centre for Obesity Research, University College London, London, United Kingdom, 2Biomedical Research Centre at UCLH and UCL, National Institute for Health Research, London, United Kingdom, 3NMR Research Unit, Queen Square MS Centre, Department of Neuroinflammation, UCL Queen Square Institute of Neurology, University College London, London, United Kingdom, 4Centre for Medical Image Computing, Department of Medical Physics and Biomedical Engineering, University College London, London, United Kingdom, 5Department of Electrical, Computer and Biomedical Engineering, University of Pavia, Pavia, Italy, 6IRCCS C., Mondino Foundation, Pavia, Italy, 7Brain Connectivity Centre, IRCCS Mondino Foundation, Pavia, Italy, 8Department of Brain and Behavioural Sciences, University of Pavia, Pavia, Italy
Anosmia or loss of smell is a common COVID-19 symptom. We studied a group of individuals with persistent anosmia and those who had recovered olfactory function following COVID-19 infection as well as healthy volunteers. Using resting state EPI and seed based analysis we found significant differences in connectivity between olfactory nodes and prefrontal regions known to be involved in smell processing. Furthermore, our analysis also identified connectivity differences between olfactory regions and brain areas involved in appetite control, highlighting areas of the brain that may be affected by COVID-19 related anosmia.
|
|
| 17:36 | 0733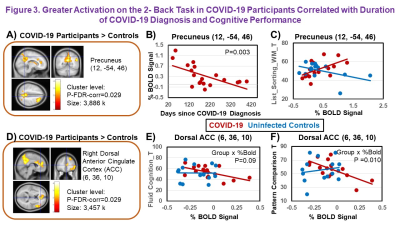 |
Abnormal Brain Activation in Post-acute Sequelae of COVID-19 Video Permission Withheld
Linda Chang1,2,3, Meghann C. Ryan4, Huajun Liang1, Xin Zhang1, Eric Cunningham1, Eleanor Wilson5, Andrea Levine6, Shyamasundaran Kottilil5, and Thomas M. Ernst1,2
1Diagnostic Radiology and Nuclear Medicine, University of Maryland School of Medicine, Baltimore, MD, United States, 2Neurology, Johns Hopkins University School of Medicine, Baltimore, MD, United States, 3Neurology, University of Maryland School of Medicine, Baltimore, MD, United States, 4Program in Neuroscience, University of Maryland School of Medicine, Baltimore, MD, United States, 5Medicine, Division of Infectious Disease, University of Maryland School of Medicine, Baltimore, MD, United States, 6Medicine, Critical Care Medicine, University of Maryland School of Medicine, Baltimore, MD, United States
Post-acute sequelae of COVID-19 is highly prevalent after the acute infection. Neuropsychiatric symptoms are particularly common; however, the pathophysiology of how the brain is affected remains unclear. This study aimed to evaluate whether convalescent COVID-19 participants have abnormal brain activation that is related to quantitative neurobehavioral measures. 21 COVID-19 participants and 20 healthy controls were evaluated with the NIH-Toolbox® and blood-oxygenation level dependent-functional MRI (BOLD-fMRI), using the N-back tasks. Despite similar performance on the NIH-Toolbox-cognitive battery, COVID-19 participants had greater brain activation than controls in the precuneus and dorsal anterior cingulate cortex, which also predicted poorer dexterity, endurance, and locomotion.
|
|
| 17:48 | 0734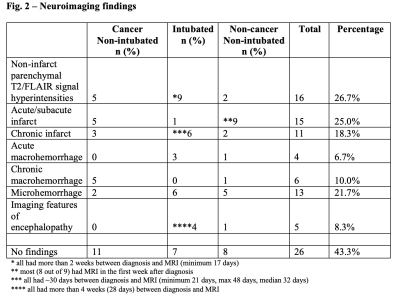 |
Neuroimaging Findings & Neurological Symptoms in COVID-19 Patients with & without Cancer: A Retrospective Multi-Center Observational Study
Lily McCarthy1, Oleksandr Khegai2, Jonathan Goldstein3, Puneet Belani4, Puneet Pawha4, Shingo Kihira4, Brian Mathew3, Kapil Gururangan3, Qing Hao3, Anuradha Singh3, Allison Navis3, Bradley Delman4, Nathalie Jette3, and Priti Balchandani2
1Icahn School of Medicine at Mount Sinai, New York, NY, United States, 2BioMedical Engineering and Imaging Institute, Icahn School of Medicine at Mount Sinai, New York, NY, United States, 3Neurology, Icahn School of Medicine at Mount Sinai, New York, NY, United States, 4Radiology, Icahn School of Medicine at Mount Sinai, New York, NY, United States
COVID-19 is known to result in neurological manifestations which sometimes correlate with neuroimaging abnormalities. Understanding these abnormalities requires further systematic study. We undertook a retrospective analysis of 60 MRIs from hospitalized COVID-19 patients (20 intubated, 20 non-brain cancer, and 20 non-intubated/non-cancer) with neurological manifestations. Neuroimaging showed non-infarct parenchymal T2/FLAIR signal hyperintensities (26.7%), acute/subacute infarcts (25%), microhemorrhages (21.7%), chronic infarcts (18.3%), chronic macrohemorrhages (10%), and acute macrohemorrhages (6.7%). Common neurological symptoms were confusion/encephalopathy/delirium (70%), generalized weakness (38.3%), and impaired responsiveness/coma (38.3%). Thus, COVID-19 may be associated with neuroimaging abnormalities. Differences in abnormalities were seen based on permutations of cancer and intubation.
|
|
| 18:12 | 0735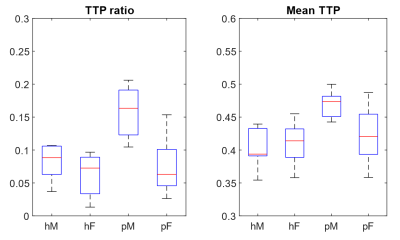 |
Lung perfusion disturbances detected with MRI in non-hospitalized post-COVID individuals with dyspnea, with sex difference.
Jimmy Zhou Yu1,2, Tobias Granberg2,3, Roya Shams2, Sven Petersson2, Adrian Szum2, Magnus Sköld4, Sven Nyrén1,2, and Johan Lundberg2,3
1Department of Molecular Medicine and Surgery, Karolinska Institutet, Stockholm Solna, Sweden, 2Radiology department, Karolinska University Hospital, Stockholm, Sweden, 3Department of Neuroscience, Karolinska Institutet, Stockholm Solna, Sweden, 4Department of Medicine, Karolinska Institutet, Stockholm Solna, Sweden
Mechanisms underlying dyspnea in non-hospitalized patients with persistent post-COVID is unknown. Lung perfusion abnormalities have been reported in acute COVID-19, and may also be important in post-COVID. Dynamic contrast enhanced (DCE)-MRI [MS1] was applied to study lung perfusion in 28 non-hospitalized patients with persistent dyspnea 4-13 months post-COVID. Time-to-peak (TTP)[MS2] maps were numerically summarized as normalized as 2 numeric values: mean TTP and TTP ratio. Comparison was made against 22 age and sex matched controls. Perfusion abnormalities were found, with a striking sex difference with men showing more pronounced perfusion abnormalities. Perfusion abnormalities correlated with self-rated dyspnea in men.
|
|
18:24 |
0736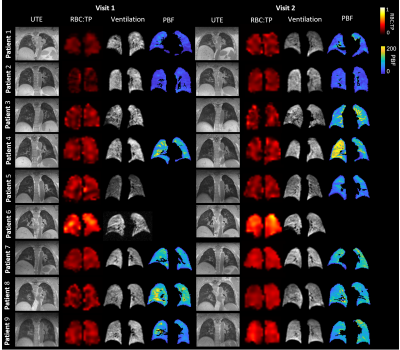 |
Multinuclear lung MRI assessment of COVID-19 patients at 6 and 12 weeks after hospital admission
Laura C. Saunders1, Guilhem J. Collier1, Ho-Fung Chan1, Paul J. C. Hughes1, Laurie J. Smith1, Helen Marshall1, James A. Eaden1, Jody Bray1, David J. Capener1, Leanne Armstrong1, Jennifer Rodgers1, Martin Brook1, Alberto M. Biancardi1, James Watson2, Zoë Gabriel2, Madhwesha R. Rao1, Graham Norquay1, Oliver Rodgers1, Fred Wilson3, Tony Cahn3,
Andy Swift1, Smitha Rajaram2, Fergus Gleeson4,5, James T. Grist5, Gary H. Mills2,6, James Meiring2, Lisa Watson2, Paul J. Collini6, Rod Lawson2, Roger Thompson1, and Jim M. Wild1
1Infection, Immunity and Cardiovascular Disease, University of Sheffield, Sheffield, United Kingdom, 2Sheffield Teaching Hospitals, Sheffield, United Kingdom, 3GlaxoSmithKline, Stevenage, United Kingdom, 4Oxford NHS Foundation Trust, Oxford, United Kingdom, 5University of Oxford, Oxford, United Kingdom, 6University of Sheffield, Sheffield, United Kingdom
This work uses a multinuclear 1H and 129Xe protocol to assess pathophysiological changes in patients with COVID-19 pneumonia, without signs of interstitial lung disease, at 6 and 12 weeks after hospital admission. 1H and 129Xe protocol: ultra-short echo time, dynamic contrast enhanced lung perfusion, 129Xe lung ventilation, 129Xe diffusion weighted MRI, 129Xe 3D spectroscopic imaging. Though significant improvements in lung ventilation homogeneity (decreased low ventilation percentage and ventilation coefficient of variation), gas transfer (increased RBC:TP, decreased TP T2*) and perfusion (increased pulmonary blood volume and flow) were seen between 6 and 12 weeks, low RBC:TP ratio persisted for some patients.
|
The International Society for Magnetic Resonance in Medicine is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians.