Power Pitch
Pitch: Antenatal, Neonatal & Pediatric MRI: Innovative Techniques & Image Optimization
Joint Annual Meeting ISMRM-ESMRMB & ISMRT 31st Annual Meeting • 07-12 May 2022 • London, UK

Power Pitch Session: How it Works
1st Hour: 2-minute Power Pitches in the Power Pitch Theater.
2nd Hour: 60-minute digital poster presentations at the smaller screens around the perimeter of the Power Pitch Theater.
| 17:00 | 0737.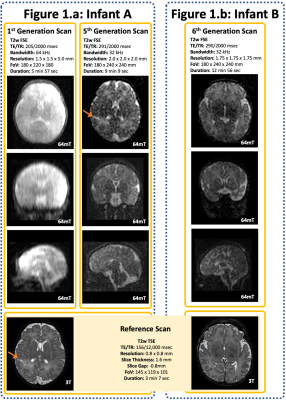 |
Optimisation of Structural MR Imaging Sequences in a Neonatal Cohort at 64 mT
Paul Cawley1,2, Francesco Padormo1,3, UNITY Consortium4, Louise Dillon1, Emer Hughes1, Jennifer Almalbis1, Joanna Robinson1,2, Alessandra Maggioni1,2, Daniel Cromb1,2, Lori Arlinghaus5, Houchun Harry Hu5, Steve Williams4, Serena Counsell1, Tomoki Arichi1, Mary Rutherford1, Joseph V. Hajnal1, and A. David Edwards1,2
1Centre for the Developing Brain, King's College London, London, United Kingdom, 2Neonatal Intensive Care Unit, Guy's & St Thomas' Hospital NHS Foundation Trust, London, United Kingdom, 3Medical Physics, Guy's & St Thomas' Hospital NHS Foundation Trust, London, United Kingdom, 4Centre for Neuroimaging Sciences, King's College London, London, United Kingdom, 5Hyperfine, Inc., Guildford, CT, United States
Point-of-care Magnetic Resonance scanning is a novel and potentially transformative technology, utilising Ultra-Low Field permanent magnets to facilitate bedside neuroimaging. Through iterative T2w sequence optimisation, we demonstrate the feasibility of using ultra-low field portable 64mT MR scanning in neonates. This pilot data demonstrates that images can provide sufficient contrast for tissue differentiation and identify pathological lesions. Scanning with ongoing intensive care was both feasible and safe.
|
|
| 17:02 | 0738.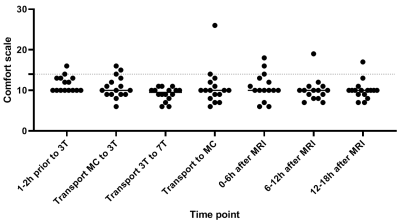 |
Vital Signs, Temperature and COMFORT Scale Scores in Infants During Ultra-High-Field MR Imaging.
Inge van Ooijen1,2, Kim Annink1, Jeroen Dudink1, Thomas Alderliesten1, Floris Groenendaal1, Maria Luisa Tataranno1, Maarten Lequin2, Hans Hoogduin2, Frederik Visser2, Alexander Raaijmakers2,3, Dennis Klomp2, Evita Wiegers2, Manon Benders1, Jannie Wijnen2, and Niek van der Aa1
1Department of Neonatology, University Medical Center Utrecht, Utrecht, Netherlands, 2Department of Radiology, University Medical Center Utrecht, Utrecht, Netherlands, 3Department of Biomedical Engineering, Eindhoven University of Technology, Eindhoven, Netherlands
7T MRI in infants could improve cerebral diagnostic quality, but safety should be evaluated before standard use. In this study, twenty infants without respiratory support between term-equivalent age and 3 months corrected age, were scanned on 7T directly after 3T MRI. Vital signs (heart rate, oxygen saturation and respiratory rate), temperature (rectal, body and brain), COMFORT scale scores and adverse events were monitored throughout the process. None of these parameters changed around 7T MRI. Also, heart rate and temperature were not significantly different during 7T, when compared to 3T MRI. Therefore scanning infants at 7T appears to be safe.
|
|
| 17:04 | 0739.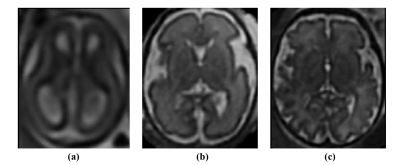 |
Automatic Assessment of Fetal Gestational Age using Bayesian Deep learning Method
Axel Largent1, Jonathan Murnick1,2, Yuan-Chiao Lu1, Kushal Kapse1, Nicole Andersen1, Todd Richmann1, Josepheen De Asis-Cruz1, Jessica Quistorff1, Catherine Lopez1, Nickie Andescavage1,3, and Catherine Limperopoulos1,2,4
1Department of Diagnostic Imaging and Radiology, Children’s National Hospital, Developing Brain Institute, Washington, DC, United States, 2Departments of Radiology and Pediatrics, George Washington University, Washington, DC, United States, 3Department of Neonatology, Children's National Hospital, Washington, DC, United States, 4Neurology School of Medicine and Health Sciences, George Washington University, 20010, DC, United States
Monitoring fetal brain development is crucial for early diagnosis of brain malformations and other congenital disorders. Standard methods to monitor brain maturation are mainly based on subjective and time-consuming visual analysis of the progression of sulcation. Our study proposed a Bayesian deep-learning method (DLM) for automatic assessment of fetal-gestational age (GA), and accurate and efficient identification of fetuses with abnormal brain development. Our Bayesian DLM showed excellent performance in predicted GA (mean-absolute-error = 0.928 weeks) and compared favorably with other state-of-the-art methods. This method may be used in clinical practice for monitoring fetal-brain development and early diagnosis of fetal brain malformations.
|
|
| 17:06 | 0740.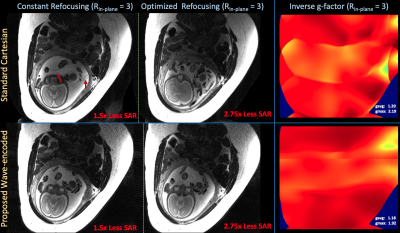 |
Improved acquisition efficiency in T2-weighted fetal MRI with optimized variable flip angles and prospective wave-encoding
Yamin Arefeen1, Borjan Gagoski2,3, Berkin Bilgic4,5, Ellen Grant2,3, and Elfar Adalsteinsson1,6,7
1Massachusetts Institute of Technology, Cambridge, MA, United States, 2Fetal-Neonatal Neuroimaging and Developmental Science Center, Boston Children’s Hospital, Boston, MA, United States, 3Harvard Medical School, Boston, MA, United States, 4Athinoula A. Martinos Center for Biomedical Imaging, Charlestown, MA, United States, 5Department of Radiology, Harvard Medical School, Boston, MA, United States, 6Harvard-MIT Health Sciences and Technology, Cambridge, MA, United States, 7Institute for Medical Engineering and Science, Cambridge, MA, United States
Fetal MRI utilizes Half-Fourier-acquisition-single-shot-turbo-spin-echo (HASTE) for motion robust imaging. However, specific-absorption-rate (SAR) constraints from the refocusing pulse train lengthens scan time and increases vulnerability to motion-induced artifacts. Variable refocusing flip angle (VFA) acquisitions improve efficiency, but may suffer from poor contrast-to-noise-ratios (CNR). We propose an optimization technique for VFA that retains ~90% CNR with 2.5x SAR reduction. Furthermore, we demonstrate the first application of wave-encoding in fetal MRI at Rin-plane = 3-fold prospectively under-sampled acquisitions. Combining HASTE, VFA, and wave-encoding improves acquisition time with reduced repetition times and shorter echo-trains and could enable simultaneous-multislice acquisitions for further acceleration.
|
|
| 17:08 | 0741.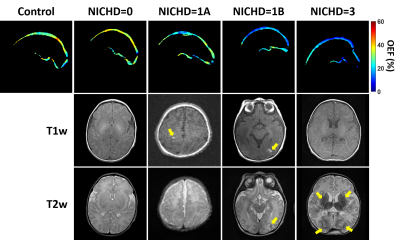 |
Regional assessment of cerebral oxygen extraction fraction in neonates with hypoxic-ischemic-encephalopathy: a pilot study
Dengrong Jiang1, W. Christopher Golden2, Aylin Tekes1, Charlamaine Parkinson2, Bruno Soares1, Avner Meoded1, Hanzhang Lu1,3,4, Frances Northington2, and Peiying Liu1,5
1Department of Radiology, Johns Hopkins University School of Medicine, Baltimore, MD, United States, 2Department of Pediatrics, Johns Hopkins University School of Medicine, Baltimore, MD, United States, 3Department of Biomedical Engineering, Johns Hopkins University School of Medicine, Baltimore, MD, United States, 4F.M. Kirby Research Center for Functional Brain Imaging, Kennedy Krieger Research Institute, Baltimore, MD, United States, 5Department of Diagnostic Radiology and Nuclear Medicine, University of Maryland School of Medicine, Baltimore, MD, United States
Hypoxic-ischemic-encephalopathy (HIE) is the leading cause of neonatal mortality and severe neurological impairment in childhood. Quantification of cerebral oxygen-extraction-fraction (OEF) in neonates with HIE may provide valuable information to guide the treatment and predict clinical outcome. In this pilot study, we used a novel MRI technique, accelerated-T2-relaxation-under-phase-contrast (aTRUPC), to measure regional OEF in neonates with HIE. We demonstrated a trend towards lower cortical OEF in HIE neonates compared to healthy controls. In addition, neonates with severer brain injury had lower cortical OEF. These findings suggest that regional OEF measurement may be useful in evaluating cerebral injuries in HIE.
|
|
| 17:10 | 0742.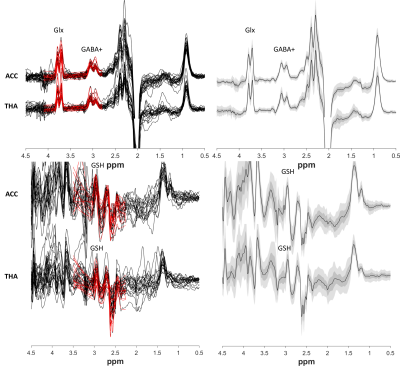 |
The effects of preterm birth on GABA+, Glx and GSH in the neonatal brain
Maria Yanez Lopez1, Anthony N Price1, Nicolaas AJ Puts2, Emer J Hughes1, Richard AE Edden3, Grainne M McAlonan2, Tomoki Arichi1, and Enrico De Vita4
1Centre for the Developing Brain, School of Biomedical Engineering and Imaging Sciences, King’s College London, London, United Kingdom, 2Department of Forensic and Neurodevelopmental Sciences, Institute of Psychiatry, Psychology & Neuroscience, King's College London, London, United Kingdom, 3Russell H. Morgan Department of Radiology and Radiological Science, The Johns Hopkins University School of Medicine, Baltimore, MD, United States, 4Biomedical Engineering Department, School of Biomedical Engineering and Imaging Sciences, King’s College London, London, UK, London, United Kingdom We have performed the first simultaneous measurement of GABA+, Glx and GSH in the preterm brain. Our main findings show that GABA+ and Glx significantly increased with postmenstrual age in preterm neonates during the 31-45 week period. We additionally found that metabolites underpinning glutamate and GABA neurotransmission levels in preterm babies were significantly lower than normative neonatal values, even when measured at the term time equivalent timepoint. We also identified higher GABA+ and Glx in the thalamus compared with the cortex. Our findings provide further support for the application of edited MRS in neurodevelopment. |
|
| 17:12 | 0743.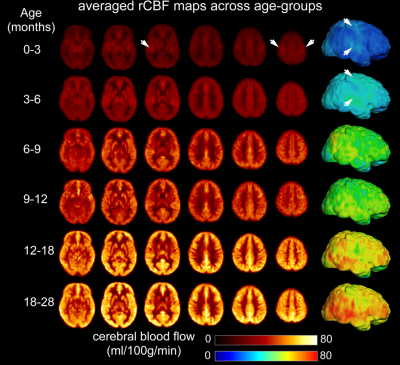 |
A biphasic pattern of cerebral blood flow increases during infancy revealed with 3D multi-shot, stack-of-spirals pCASL and phase-contrast MRI
Minhui Ouyang1,2, John Detre3, Jessica L Hyland1, Kay Laura Sindabizera1, Yun Peng4, J. Christopher Edgar1,2, and Hao Huang1,2
1Department of Radiology, Children's Hospital of Philadelphia, Philadelphia, PA, United States, 2Department of Radiology, Perelman School of Medicine, University of Pennsylvania, Philadelphia, PA, United States, 3Department of Neurology, Perelman School of Medicine, University of Pennsylvania, Philadelphia, PA, United States, 4Department of Radiology, Beijing Children’s Hospital, Capital Medical University, Beijing, China
Infancy is one of the most prominent times of daily energy expenditure across the lifespan. Here, using cutting-edge pCASL with high-resolution at isotropic 2.5mm and phase-contrast MRI, we delineated the developmental trajectory of the infant’s global and regional cerebral blood flow (rCBF) supporting the metabolic needs for brain development in 0-28months. Significant age-related CBF increases during infancy were better modeled with biphasic linear models, with break-point ages observed earlier in sensorimotor and auditory cortices and later in association cortices. The established population-averaged rCBF maps across infancy can serve as normative rCBF atlases for neuroscientific research or clinical care.
|
|
| 17:14 | 0744.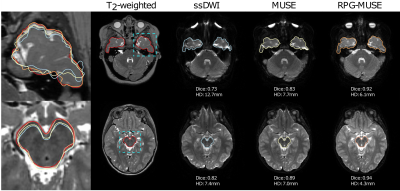 |
Improved geometric fidelity in brain DWI of pediatric patients using Multiplexed Sensitivity Encoding (MUSE)
Jens Krister Johansson1, Kerstin Lagerstrand2,3, Liz Ivarsson4, Pär-Arne Svensson4, Hanna Hebelka1,4, and Stephan Maier1,5
1Department of Radiology, Institute of Clinical Sciences, Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden, 2Medical radiation sciences, Institute of Clinical Sciences, Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden, 3Department of Medical Physics and Biomedical Engineering, Sahlgrenska University Hospital, Gothenburg, Sweden., Gothenburg, Sweden, 4Department of Radiology, Sahlgrenska University Hospital, Gothenburg, Sweden., Gothneburg, Sweden, 5Department of Radiology,, Brigham and Women's Hospital, Boston, MA, United States, Boston, MA, United States This study demonstrates that DWI with MUSE and RPG correction significantly reduces the geometric distortions and results in increased overall image quality without altering ADC in a pediatric patient population, compared to single-shot EPI. This improvement was confirmed both through quantitative and qualitative analysis. |
|
| 17:16 | 0745.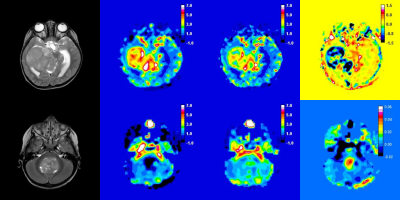 |
Prediction of survival in paediatric brain tumour patients using multicentre leakage-corrected perfusion MRI
Stephanie Withey1,2,3, Lesley MacPherson4, Adam Oates4, Stephen Powell3, Jan Novak2,3,5, Laurence Abernethy6, Barry Pizer7, Richard Grundy8, Paul S. Morgan8,9,10, Simon Bailey11, Dipayan Mitra12, Theodoros N. Arvanitis2,13, Dorothee P. Auer10,14,15, Shivaram Avula6, and Andrew C. Peet2,3
1RRPPS, University of Birmingham NHS Foundation Trust, Birmingham, United Kingdom, 2Oncology, Birmingham Women’s and Children’s NHS Foundation Trust, Birmingham, United Kingdom, 3Institute of Cancer and Genomic Sciences, University of Birmingham, Birmingham, United Kingdom, 4Radiology, Birmingham Women’s and Children’s NHS Foundation Trust, Birmingham, United Kingdom, 5Department of Psychology, Aston University, Birmingham, United Kingdom, 6Radiology, Alder Hey Children’s NHS Foundation Trust, Liverpool, United Kingdom, 7Oncology, Alder Hey Children’s NHS Foundation Trust, Liverpool, United Kingdom, 8The Children’s Brain Tumour Research Centre, University of Nottingham, Nottingham, United Kingdom, 9Medical Physics, Nottingham University Hospitals, Nottingham, United Kingdom, 10Division of Clinical Neuroscience, University of Nottingham, Nottingham, United Kingdom, 11Sir James Spence Institute of Child Health, Royal Victoria Infirmary, Newcastle upon Tyne, United Kingdom, 12Neuroradiology, Royal Victoria Infirmary, Newcastle upon Tyne, United Kingdom, 13Institute of Digital Healthcare, University of Warwick, Coventry, United Kingdom, 14Nottingham University Hospitals Trust, Neuroradiology, Nottingham, United Kingdom, 15NIHR Nottingham Biomedical Research Centre, Nottingham, United Kingdom
Dynamic susceptibility (DSC-) MRI provides measures of relative cerebral blood volume (rCBV) in paediatric brain tumours. Correction of rCBV for the effects of contrast agent leakage can be done using post-processing techniques. Eighty-five patients with a range of paediatric brain tumours underwent DSC-MRI scans at 4 centres using variable protocols. Leakage-corrected and uncorrected DSC-MRI parameters were calculated and patients were followed up. Median DSC-MRI parameters significantly predicted overall survival.
|
|
| 17:18 | 0746. |
Virtual Reality Patient Training for Magnetic Resonance Imaging
Alexandra G. O'Neill1, Brian A. Hargreaves2, Karla Epperson2, Bruce L. Daniel2, and Christoph Leuze2
1Mathematics, Manhattan College, Riverdale, NY, United States, 2Radiology, Stanford University, Stanford, CA, United States
For many patients, particularly pediatric patients, MRI exams can be intimidating primarily due to the confined space and loud noises. This can result in failed, non-diagnostic, or degraded exams at cost and even risk to the patient. We present a virtual reality application for mobile devices, such as mobile phones, of a Magnetic Resonance Imaging simulation and training software to serve as a tool for medical professionals to prepare children for MRI scans. Initial evaluations show promising results for reducing movement in test subjects and potential for reducing worry or anxiety among individuals preparing for MRI.
|
|
| 17:20 | 0747. | What do children need to learn for an MRI-scan? Gamification of learning goals into the cosmo@home app
Sam Geuens1, Sanne Nauts2, Anas Abdelrazeq3, Michael Aertsen1, Gunnar Buyse1, Philippe Demaerel1, Jurgen Lemiere1, Jessica Nijs1, Greet Pauwels4, Marlies Potoms5, Saini Privender2, Kate Sauer4, Marie Sjölinger 6, Olov Ståhl6, Marlies Treunen7, Sofie Van Cauter8,9, Leen Wouters8,9, and Barbara Weyn7
1University Hospitals Leuven, KU Leuven, Leuven, Belgium, 2Philips, Eindhoven, Netherlands, 3RWTH Aachen University, Aachen, Germany, 4AZ Sint-Jan Brugge, Brugge, Belgium, 5Jessa Ziekenhuis, Hasselt, Belgium, 6RISE, Stockholm, Sweden, 7KU Leuven, Leuven, Belgium, 8Ziekenhuis Oost-Limburg, Genk, Belgium, 9Center for Translational Psychological Research TRACE, Ziekenhuis Oost-Limburg, Genk, Belgium
Undergoing an awake MRI-scan can be very stressful for young children and bears the risk that image quality is poor due to motion artefacts. Behavioral training by an experienced trainer has shown success in preparing children before a scan, however, this approach is costly and trainer dependent. We have designed a mobile app to prepare children for an upcoming MRI-scan at home. This app was tested by 52 children in four different hospitals. First data show that children and parents appreciate the app very much and that learning goals can be reached with a digital application at home.
|
The International Society for Magnetic Resonance in Medicine is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians.