Combined Educational & Scientific Session
Enriching Our Toolbox to Link Tumor Morphology with Behavior
ISMRM & ISMRT Annual Meeting & Exhibition • 03-08 June 2023 • Toronto, ON, Canada

| 13:30 | PET/MR Patrick Veit-Haibach | |
| 13:50 | Hypoxia Imaging with PET/CT and PET/MRI Deena Neriman | |
| 14:10 | 0889.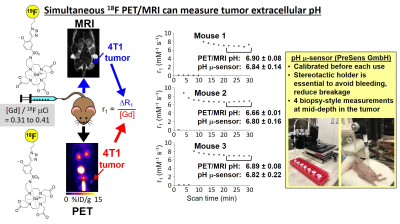 |
Simultaneous PET/MRI can measure extracellular pH in the tumor microenvironment
Alyssa C Pollard1,2, Jorge de la Cerda1, F William Schuler1, Tyler R Pollard1, Aikaterini Kotrotsou1, Loreno Palagi3, Chetan Dhakan1, Federica Pisaneschi1, and Mark D Pagel4
1Department of Cancer Systems Imaging, MD Anderson Cancer Center, Houston, TX, United States, 2Department of Chemistry, Rice University, Houston, TX, United States, 3Department of Molecular Biotechnology and Health Sciences, University of Torino, Torino, Italy, 4Department of Cancer Systems Imaging, UT MD Anderson Cancer Center, Houston, TX, United States Keywords: PET/MR, Contrast Agent, pH imaging Acidosis is a useful biomarker for tumor diagnoses and for evaluating early response to anti-cancer treatments. T1-based MRI contrast agents have been developed with a r1 relaxivity that is responsive to extracellular pH (pHe) in the tumor microenvironment. However, the concentration of these agents in the tumor must also be known to determine r1 relaxivity. We have developed PET/MRI co-agents that can be evaluated with simultaneous PET/MRI during pre-clinical studies with mouse models of human cancers. The PET agent reports on the concentration of the agents, which can be used to determine r1 relaxivity and estimate pHe in tumors. |
| 14:18 | 0890.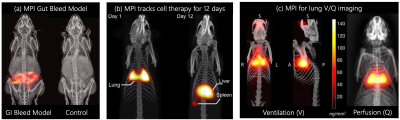 |
Brownian superparamagnetic iron oxide nanoparticles enable therapeutic cell viability monitoring with Magnetic Particle Imaging
Renesmee Kuo1, Chinmoy Saayujya2, Kim Hwang Yeo2, Irati Rodrigo2, Prashant Chandrasekharan2, Quincy Huynh2, Benjamin Fellows2, John Pauly1, and Steven Conolly2
1Stanford University, Stanford, CA, United States, 2University of California, Berkeley, Berkeley, CA, United States Keywords: Molecular Imaging, Cell Tracking & Reporter Genes Molecular imaging tools can noninvasively track cells in vivo. However, no techniques today can rapidly monitor cell therapies to allow for nimble treatment optimization for each patient, the epitome of Personalized Medicine. Magnetic Particle Imaging (MPI) is a new tracer imaging technology that could soon provide MDs unequivocal therapy treatment feedback in just three days. MPI with Brownian SPIOs shows promise towards noninvasive sensing of cell viability via viscosity changes in apoptotic cells. This unique ability could greatly improve the efficacy of cell therapies by enabling rapid personalization of the treatment. |
| 14:26 | 0891.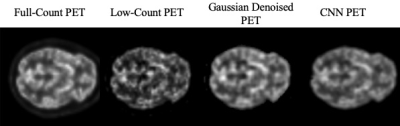 |
Anatomical MRI-guided deep learning-based low-count PET image recovery without the need for training data – a PET/MR study
Tianyun Zhao1, Thomas Hagan1, Christine DeLorenzo1,2, and Chuan Huang1,3
1Biomedical Engineering, Stony Brook University, Stony Brook, NY, United States, 2Psychiatry, Stony Brook Medicine, Stony Brook, NY, United States, 3Radiology, Stony Brook Medicine, Stony Brook, NY, United States Keywords: PET/MR, PET/MR The advent of simultaneous PET/MRI enables the possibility of using MRI to guide PET image reconstruction/recovery. Deep-learning approaches have been explored in low-count PET recovery, with current approaches focus on supervised learning, which requires a large amount of training data. A recently proposed unsupervised learning image-recovery approach does not require this but relies on the optimal stopping criterion. In this work, we developed an unsupervised learning-based PET image recovery approach using anatomical MRI as input and a novel stopping criterion. Our method achieved better image recovery in both global image similarity metrics and regional standard uptake value (SUV) accuracy. |
| 14:34 | 0892.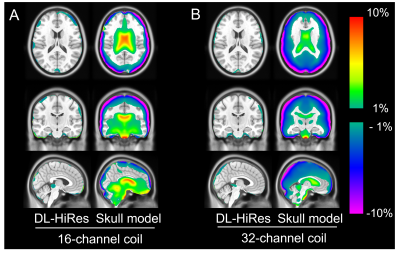 |
Evaluation of deep learning high-resolution Dixon PET/MR attenuation correction using 16-channel head-neck and 32-channel head coils
Chunwei Ying1, Yasheng Chen2, Matthew R. Brier2, Shaney Flores1, Richard Laforest1, Tammie L. S. Benzinger1,2,3, and Hongyu An1,2
1Mallinckrodt Institute of Radiology, Washington University School of Medicine, St Louis, MO, United States, 2Department of Neurology, Washington University School of Medicine, St Louis, MO, United States, 3Department of Neurosurgery, Washington University School of Medicine, St Louis, MO, United States Keywords: PET/MR, Brain, attenuation correction We evaluated the accuracy of a deep learning-based PET/MR attenuation correction (AC) method with vendor-provided high-resolution Dixon in- and opp-phase images as inputs (DL-HiRes). We found that the DL-HiRes AC method significantly outperformed the vendor-provided skull model AC method for both 16-channel head-neck coil and 32-channel head coil (p<0.001). Moreover, the DL-HiRes method had similar AC accuracy using different head coils. |
| 14:42 | 0893.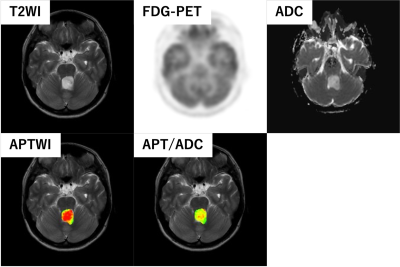 |
Amide proton transfer image corrected by apparent diffusion coefficient improved diagnostic accuracy in grading brain tumors on a PET/MR system
Koji Sagiyama1, Osamu Togao2, Takeshi Kamitani1, Koji Yamashita3, Yuzo Yamasaki1, Kazufumi Kikuchi1, Takuya Hino1, and Kousei Ishigami1
1Department of Clinical Radiology, Graduate School of Medical Sciences, Kyushu University, Fukuoka, Japan, 2Department of Molecular Imaging and Diagnosis, Graduate School of Medical Sciences, Kyushu University, Fukuoka, Japan, 3Department of Radiology Informatics and Network, Graduate School of Medical Sciences, Kyushu University, Fukuoka, Japan Keywords: Tumors, PET/MR, Amide Proton Imaging, Apparent Diffusion Coefficient, ADC Amide proton transfer (APT) imaging is useful for grading brain tumors; however, its diagnostic accuracy is compromised by the heterogeneity of the tumor's structure. In this study, we investigated using a PET-magnetic resonance (PET/MR) system whether dividing the APT by the apparent diffusion coefficient (ADC) improves the diagnostic ability of high-grade and low-grade brain tumors by correcting for the effects of tissue structure. The corrected APT (APT/ADC) showed the best diagnostic performance in grading brain tumors compared to APT, ADC, and standardized uptake value (SUV) alone. |
| 14:50 | 0894.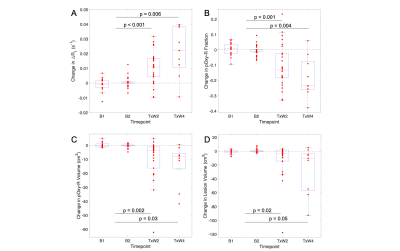 |
Oxygen-Enhanced MRI Assessment of Radiotherapy-Induced Treatment Effects in Patients with Head and Neck Cancer
Michael J Dubec1,2, John Gaffney3, David L Buckley2,4, Michael Berks1, Anubhav Datta1,5, Damien J McHugh1,2, Ross A Little1, Susan Cheung1, Christina Hague3, Julian C Matthews6, Ananya Choudhury1,3, Marcel van Herk1, Andrew McPartlin7, Geoff JM Parker8,9, and James PB O'Connor1,5,10
1Division of Cancer Sciences, University of Manchester, Manchester, United Kingdom, 2Christie Medical Physics and Engineering, The Christie NHS Foundation Trust, Manchester, United Kingdom, 3Clinical Oncology, The Christie NHS Foundation Trust, Manchester, United Kingdom, 4Biomedical Imaging, University of Leeds, Leeds, United Kingdom, 5Radiology, The Christie NHS Foundation Trust, Manchester, United Kingdom, 6Neuroscience and Experimental Psychology, University of Manchester, Manchester, United Kingdom, 7Radiation Medicine, Princess Margaret Cancer Centre, Toronto, ON, Canada, 8Bioxydyn Ltd, Manchester, United Kingdom, 9Centre for Medical Image Computing, University College London, London, United Kingdom, 10Radiotherapy and Imaging, Institute of Cancer Research, London, United Kingdom Keywords: Cancer, Head & Neck/ENT, Tumour Hypoxia, Radiotherapy, OE-MRI, MR Linac Hypoxia is common to most solid tumours and mediates treatment resistance. Oxygen-enhanced (OE)-MRI can identify, map and quantify hypoxia in multiple tumour types including H&N cancer. We build upon previous work to show that OE-MRI biomarkers: (i) can be deployed on multiple MRI systems; (ii) are repeatable; (iii) can detect cohort level response to radiotherapy; (iv) can identify which individual lesions have significant changes in their oxygenation, hypoxic volume and hypoxic fraction. |
| 14:58 | 0895.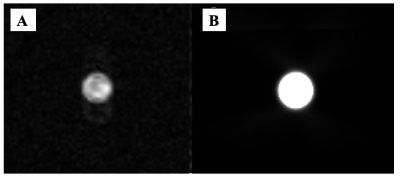 |
In-Vivo Simultaneous Hyperpolarized 129Xe MRI and [15O]-water PET Multi-Modal Imaging: A Proof of Concept Study
Ramanpreet K. Sembhi1, Matthew S. Fox1,2, Heeseung Lim2,3, Justin W. Hicks2,4, Shawn N. Whitehead5, Jonathan D. Thiessen2,4, Grace Parraga4,6, and Alexei V. Ouriadov1,2,7
1Department of Physics and Astronomy, The University of Western Ontario, London, ON, Canada, 2Lawson Health Research Institute, London, ON, Canada, 3Siemens Healthcare Limited, London, ON, Canada, 4Department of Medical Biophysics, The University of Western Ontario, London, ON, Canada, 5Department of Anatomy and Cell Biology, The University of Western Ontario, London, ON, Canada, 6Robarts Research Institute, London, ON, Canada, 7School of Biomedical Engineering, The University of Western Ontario, London, ON, Canada Keywords: PET/MR, Hyperpolarized MR (Gas) In this proof-of-concept study, simultaneous 129Xe-based MRI and [15O]-water PET images were collected and compared from rat brain. For initial validation phase in phantoms, we have dissolved 129Xe in [15O]-water to simultaneously use both imaging modalities and confirm that PET/MRI images reflect the true density of the 15O/129Xe. The comparison results show similarity between both imaging modalities and tracers, moving towards the next step in validating the Xenon imaging technique as a potential for brain perfusion measurement. The acquisitions were carried out using a 3T PET/MRI (Siemens Biograph mMR). |
| 15:06 | 0896.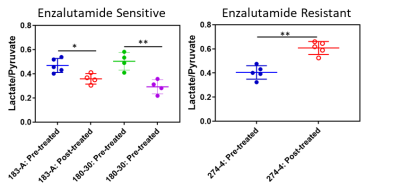 |
Combining Hyperpolarized Magnetic Resonance and Positron Emission Tomography to Interrogate Prostate Cancer Metabolism
Jose Santiago Enriquez1,2, Prasanta Dutta1, Ryan C Armijo1, Muxin Wang1, Jenny Jie Han1, Peter Shepherd3, Daniel Frigo1,2, Mark Titus3, Federica Pisaneschi1, and Pratip Bhattacharya1,2
1Cancer System Imaging, UT MD Anderson Cancer Center, Houston, TX, United States, 2UT MD Anderson Cancer Center UT Health Science Center Houston Graduate School of Biomedical Sciences, Houston, TX, United States, 3Genitourinary Medical Oncology, UT MD Anderson Cancer Center, Houston, TX, United States Keywords: PET/MR, Cancer, Prostate Cancer, Metabolic Imaging, Hyperpolarized MR Many advanced prostate cancer patients receiving anti-androgens (Enzalutamide) as the first line of treatment, develop resistance which relapses into metastatic castrate-resistant prostate cancer (mCRPC). Treatment options for mCRPC patients are limited and continue to pose a significant oncological challenge with an alarming low survival rate of only 28%. The overarching goal of this research is thus to develop personalized metabolic imaging modality to target treatment strategies of different metabolic sub-types of prostate cancer by targeting pyruvate-to-lactate metabolism by hyperpolarized [1-13C]-pyruvate MR and fatty acid oxidation by 18F-FPIA PET. |
| 15:14 | 0897.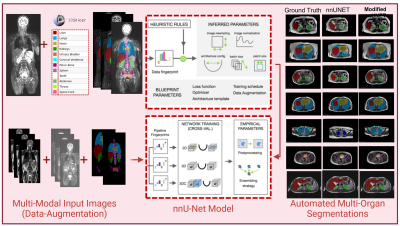 |
Deep Learning Based Automated Multi-Organ Segmentation in Lymphoma Patients using Whole Body Multiparametric MRI Images
Anum Masood1,2, Sølvi Knapstad2, Håkon Johansen3, Trine Husby3, Live Eikenes 1, Pål Erik Goa2,3, and Mattijs Elschot 1,3
1Department of Circulation and Medical Imaging, NTNU, Trondheim, Norway, 2Department of Physics, NTNU, Trondheim, Norway, 3Department of Radiology and Nuclear Medicine, St. Olavs Hospital, Trondheim University Hospital, Trondheim, Norway Keywords: Segmentation, Data Processing, Automated Segmentation, Deep Learning, nnUnet Widespread of lymphoma cancer makes manual segmentation of metastatic lymph nodes a tedious task. Lymphoma cancer is assigned an anatomic stage using the Ann Arbor system which relies on the segmentation and localization of affected lymph nodes with respect to anatomical stations. We present a framework for multi-organ segmentation for multiparametric MRI images. Our modified nnUnet using a transfer learning approach achieved 0.8313 mean DSC and 0.659 IoU in lymphoma cancer dataset. |
| 15:22 | 0898.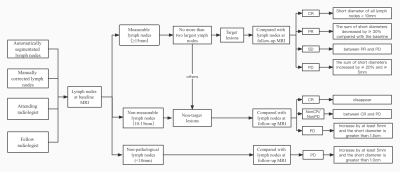 |
Semiautomated Pelvic Lymph Node Treatment Response Evaluation for Patients with Advanced Prostate Cancer: Based on MET-RADS-P Guidelines
xiang liu1 and xiaoying wang1
1peking university first hospital, Beijing, China Keywords: Cancer, Prostate, metastases This retrospective study aims to develop and evaluate a deep learning-based algorithm for semiautomated treatment response assessment of pelvic lymph nodes. A total of 162 patients who had undergone at least two scans for follow-up assessment after advanced prostate cancer metastasis treatment were enrolled. A previously reported deep learning model was used to perform automated segmentation of pelvic lymph nodes. Our results showed that the accuracies of automated segmentation-based response assessment were high for all the target lesions, nontarget lesions and nonpathological lesions according to MET-RADS-P criteria and achieved good consistency with the attending radiologist and fellow radiologist. |
The International Society for Magnetic Resonance in Medicine is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians.