Digital Poster
Coronavirus Disease (COVID-19): Novel MR Research in the Brain & Beyond
ISMRM & ISMRT Annual Meeting & Exhibition • 03-08 June 2023 • Toronto, ON, Canada

| Computer # | |||
|---|---|---|---|
1898.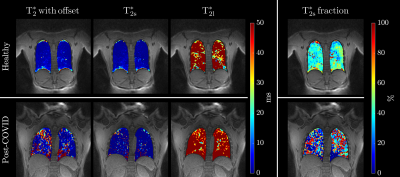 |
81 | Free Breathing δUTE Sequence for T2* Mapping of Lung in Healthy and Post-COVID Adults
Vadim Malis1, Yoshimori Kassai2, Won Bae1,3, Diana Vucevic1, Yoshiharu Ohno4, and Mitsue Miyazaki1
1Radiology, UC San Diego, San Diego, CA, United States, 2Canon Medical, Ōtawara-shi, Japan, 3VA San Diego Healthcare System, San Diego, CA, United States, 4Fujita Health University, Toyoake, Japan Keywords: Pulse Sequence Design, Lung, UTE, Ultra-Short TE δUTE sequence collects multiple closely spaced short TE (<2ms) echoes resulting in a more accurate T2* mapping of anatomies with short T2 time. Application to lungs reveals inhomogeneities in T2* maps in post-COVID-19 adults. |
|
| 1899. | 82 | Dysfunctional Respiratory Patterns in Symptomatic Post-Acute Covid-19 Patients on Dynamic High Temporal Resolution Free-Breathing Lung MRI
Lea Azour1, Artem Mikheev1, Henry Rusinek1, Mahesh Bharath Keerthivasan2, Mary Bruno1, William Moore1, and Hersh Chandarana1
1Radiology, NYU Langone Health, New York, NY, United States, 2Siemens Medical Solutions, New York, NY, United States Keywords: Lung, COVID-19 Dynamic high temporal resolution free-breathing MRI allows for quantification of respiratory duration, depth and rate—parameters separate from those provided by pulmonary function tests. Post-acute Covid patients with persisting cardiopulmonary symptoms demonstrated larger tidal area, longer duration of inspiration, and larger variability in respirations. |
|
1900.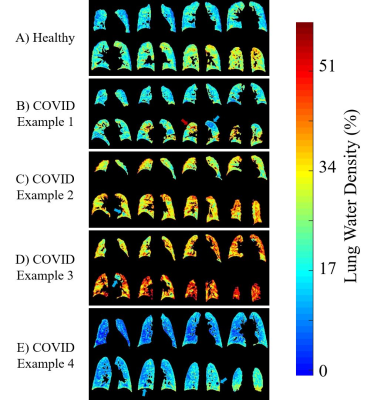 |
83 | Persistent Abnormalities in Lung Water Density Observed After COVID-19 Recovery
Christopher Ellis Keen1, Justin Grenier1, Peter Šereš1, Robert Stobbe1, James White2, Christian Beaulieu1, Ian Paterson3, and Richard Thompson1
1Department of Biomedical Engineering, University of Alberta, Edmonton, AB, Canada, 2Libin Cardiovascular Institute, University of Calgary, Calgary, AB, Canada, 3Division of Cardiology, University of Alberta, Edmonton, AB, Canada Keywords: Lung, COVID-19 The long term effects of COVID-19, including those affecting the lung, represent a new global health burden. Lung water density (LWD) MRI is an emerging quantitative technique that can be used to measure relative LWD (rLWD) in 3D. 187 patients were imaged 5 months after COVID-19 recovery using LWD MRI and were compared to 91 healthy controls. The COVID-recovered group displayed significantly higher mean rLWD values as compared to healthy controls. Additionally, local and global patterns of abnormally increased and decreased rLWD were observed in the COVID-recovered group. |
|
1901.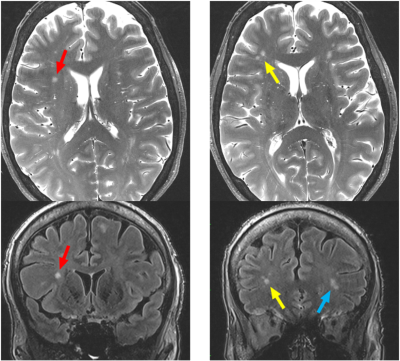 |
84 | Structural and Neuroradiological Findings in COVID-19 Patients with Post-COVID Neurological Symptoms with Ultrahigh Field 7T MRI
Shams Rashid1,2, Oleksandr Khegai1, Nathalie Jette3, Puneet Belani1, Puneet Pawha1, Sera Saju1, Ameen Al Qadi1, Allison Navis3, Brian Mathew3, Jonathan Goldstein3, Kapil Gururangan3, Qing Hao3, Anuradha Singh3, Jacqueline Becker4, Bradley Delman1, and Priti Balchandani1,2
1Diagnostic, Molecular and Interventional Radiology, Icahn School of Medicine at Mount Sinai, New York, NY, United States, 2BioMedical Engineering and Imaging Institute, Icahn School of Medicine at Mount Sinai, New York, NY, United States, 3Neurology, Icahn School of Medicine at Mount Sinai, New York, NY, United States, 4General Internal Medicine, Icahn School of Medicine at Mount Sinai, New York, NY, United States Keywords: Infectious disease, COVID-19, Ultrahigh Field, hippocampal subfields, amygdala subnuclei We present preliminary findings of neuroradiological analysis and FreeSurfer-based cortical segmentation analysis which show changes in deep gray matter structures from ultrahigh field MR neuroimaging at 7T in patients with post-COVID neurological symptoms. 8 hippocampal subfields and 4 amygdala subnuclei had significantly increased volume in a cohort of 12 COVID-19 patients with post-COVID neurological symptoms compared to matched healthy controls. These changes may indicate neuroinflammation of the hippocampus and amygdala in COVID-19, which may be related to the neurological symptoms of memory impairment, “brain fog” and anxiety in our COVID patient cohort.
|
|
1902.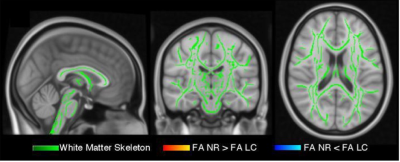 |
85 | Structural Brain Differences and Cognitive Performance between patients with Long-COVID and Normal Recovery
Breanna Nelson1,2, Nishtha Parag1, Lea Farah1, Portia Kuivi1, Alysha Alimohamed1, Harneet Bariana1, Bella Way1, Catie Song1, Ava Grier1, Chiara DeMarni1, Jacob Stubbs1,2, Megan Harper1, Wayne Su1, Johnson Chen3, Jessamyn McKenzie1, Vesna Sossi1, Mypinder Sekhon3, Donna Lang1,2, Jonathan Stoessl1,3, Cheryl Wellington1,
Noah Silverberg1,3, and William Panenka1,2
1University of British Columbia, Vancouver, BC, Canada, 2BC Children's Hospital Research Institute, Vancouver, BC, Canada, 3Vancouver Coastal Health, Vancouver, BC, Canada Keywords: White Matter, COVID-19 Previous research suggests that COVID-19 infection may be associated with brain changes that are similar to a decade of aging.1 It is unknown whether symptom duration influences brain structure. We compared participants with COVID-19 symptoms for more than 2 months (long-COVID) (n=43) to participants who recovered within 2 months (normal recovery) (n=56). We assessed white matter with diffusion tensor imaging, regional brain volumes using Freesurfer, and cognition using the NIH Toolbox. Although the effect of age on MRI indices and cognition was readily detectable, we found no differences between long-COVID and normal recovery on brain structure or cognitive performance. |
|
1903.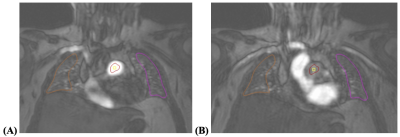 |
86 | Application of Pulmonary Perfusion Analysis in Phenotyping COVID-19 Cardiopulmonary Disease with Magnetic Resonance Imaging
Andrew C. Lancaster1, Yoko Kato2, Chia-Ying Liu3, Yoshimori Kassai3, Jaclyn Sesso2, Joao A. C. Lima2,4, and Bharath Ambale-Venkatesh4
1School of Medicine, Johns Hopkins University, Baltimore, MD, United States, 2Division of Cardiology, Department of Medicine, Johns Hopkins University School of Medicine, Baltimore, MD, United States, 3Canon Medical Systems Corporation, Otawara, Japan, 4Department of Radiology and Radiological Sciences, Johns Hopkins University School of Medicine, Baltimore, MD, United States Keywords: Vessels, COVID-19, Perfusion Pulmonary perfusion analysis of cardiac magnetic resonance imaging in patients with previous COVID-19 may help phenotype patients with advanced cardiopulmonary disease. Lung perfusion analysis was performed and results were correlated with clinical data in patients who were treated for COVID-19 at Johns Hopkins institutions. Older age and hospitalization for COVID-19 were found to be related to worse pulmonary perfusion, as measured by the perfusion parameter 50% max intensity, suggesting that one long-term sequela of severe COVID-19 that requires hospitalization, particularly in older patients, is a global bilateral decrease in the speed at which the lungs are perfused. |
|
1904. |
87 | MRI for characterization of cardiac function in suspected myocarditis as post-acute sequelae of COVID-19
El-Sayed H. Ibrahim1, Jason Rubenstein1, Antonio Sosa1, Kevin Koch1, Jadranka Stojanovska2, and Ivor Benjamin1
1Medical College of Wisconsin, Milwaukee, WI, United States, 2New York University, New York, NY, United States Keywords: Myocardium, COVID-19 Among COVID-19 induced cardiac complications, myocarditis has clinical significance because it can result in permanent myocardial damage which leads to poor outcome. In this study, we studied 65 consecutive COVID-19 patients who underwent cardiac MRI post COVID-19 due to concerns of post-COVID myocarditis or other cardiomyopathies, where MRI was used to identify suspected versus excluded myocarditis based on LGE and T1/ECV/T2 mappings. The results demonstrated the value of MRI systolic strain and diastolic strain rate as sensitive markers for early detection of subclinical cardiac dysfunction and characterizing the heart contractility pattern in high-risk patients with suspected myocarditis versus excluded myocarditis. |
|
1905.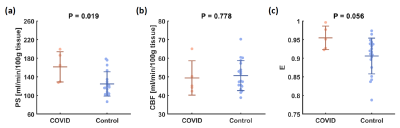 |
88 | Blood-brain barrier breakdown in COVID-19 ICU survivors: a preliminary study
Wen Shi1, Dengrong Jiang2, Hannah Rando3, Shivalika Khanduja3, Zixuan Lin2, Kaisha Hazel2, George Pottanat2, Ebony Jones2, Cuimei Xu2, Doris D.M. Lin2, Sevil Yasar4, Sung-Min Cho5, and Hanzhang Lu1,2
1Department of Biomedical Engineering, Johns Hopkins University School of Medicine, Baltimore, MD, United States, 2Department of Radiology, Johns Hopkins University School of Medicine, Baltimore, MD, United States, 3Department of Surgery, Johns Hopkins University School of Medicine, Baltimore, MD, United States, 4Department of Medicine, Johns Hopkins University School of Medicine, Baltimore, MD, United States, 5Department of Neurology, Neurosurgery, Surgery, Anesthesiology, and Critical Care Medicine, Johns Hopkins University School of Medicine, Baltimore, MD, United States Keywords: Infectious disease, COVID-19 COVID-19 affects multiple organ systems in the acute phase, however, limited knowledge is known about the long-term impact on the brain following COVID-19 pneumonia, especially for those severe COVID-19 ICU survivors. Here, we used a water-extraction-with-phase-contrast-arterial-spin-tagging (WEPCAST) MRI which can non-invasively measure BBB permeability to water. The results showed significantly higher permeability-surface-area product (PS) in COVID-19 ICU survivors, which provided preliminary evidence that there was a BBB breakdown in COVID-19 ICU survivors at 4 months after initial infection. |
|
1906.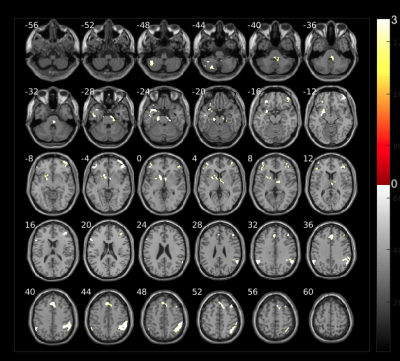 |
89 | COVID-19 olfactory rehabilitation assessment through fMRI and VBM
Pablo García-Polo1,2, Angel Torrado-Carvajal2, Mar Jiménez3, Juan Bachiller3, Vicente Martínez3, Adolfo Toledano4, Cristina Gómez2, and Susana Borromeo2
1GE Healthcare, Madrid, Spain, 2University Rey Juan Carlos, Móstoles, Spain, 3Hospital Quironsalud Madrid, Pozuelo de Alarcón, Spain, 4Hospital Universitario Fundación Alcorcón, Alcorcón, Spain Keywords: Infectious disease, COVID-19, Anosmia Olfactory fMRI has provided an objective assessment of olfactory function in normal brain and pathological subjects. Optimizing the fMRI acquisition is of paramount importance when studying olfactory areas due to high B0 inhomogeneities and thin cortical areas involved. Fully synchronizing the acquisition to the odorants delivery with patient respiration increases the effectiveness of the experiment. Using this technique in COVID-19 patients with anosmia could determine the correct rehabilitation therapy for these subjects and new treatment pathways. |
|
1907.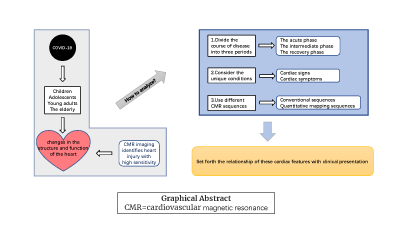 |
90 | Cardiovascular Magnetic Resonance Imaging Appearance During the Acute, Intermediate and Convalescent Phase of COVID-19 Patient
Yufan Qian1, Weibo Chen2, Yan Zhou1, Lei Zhao3, and Lian-Ming Wu1
1Shanghai Jiao Tong University School of Medicine Affiliated Renji Hospital, Shanghai, China, 2Philips Healthcare, Shanghai, China, 3Beijing Anzhen Hospital, Capital Medical University, Shanghai, China Keywords: Heart, COVID-19, review The purpose is to find the cardiac involvement features of COVID-19 using cardiac MRI, and set forth the relationship of these cardiac features with their clinical presentation. We analyzed the results under the separate cardiovascular magnetic resonance sequences combining different stages, as well as consider the unique conditions when cardiovascular signs and symptoms are present. |
|
1908.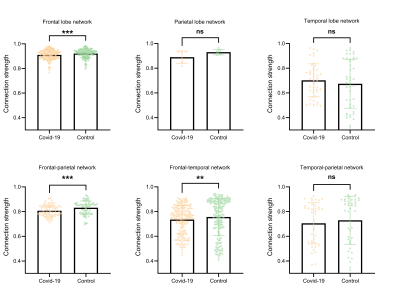 |
91 | Potential brain neural mechanisms underlying Long-COVID-19 syndrome
Tingting Pan1,2, Yaping Wu2, Xuan Yu2, Yan Bai2, and Meiyun Wang1,2
1Henan academy of sciences, Zhengzhou, China, 2Department of Medical Imaging, Henan Provincial People's Hospital & the People's Hospital of Zhengzhou University, Zhengzhou, China Keywords: Brain Connectivity, COVID-19 The neural mechanisms underlying the neuropsychiatric disorders suffered by Long-Covid-19 patients remain unknown. Non-invasive [18F]-fluorodeoxyglucose positron emission tomography/computed tomography (18F-FDG PET/CT) brain imaging is an effective way to study this issue. In the present study, based on 18F-FDG PET brain imaging and analysis of the brain metabolic network, we found significant reductions in metabolic levels in the frontal, temporal, and parietal lobes in patients with Long-Covid-19. A significant reduction in metabolic connectivity between temporal and frontal networks in patients with Long-Covid-19 may be the underlying neural mechanism underlying cognitive impairment. |
|
1909.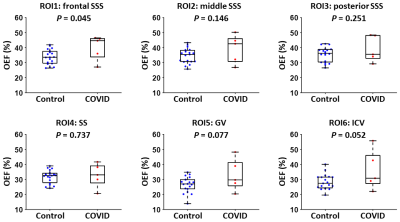 |
92 | Frontal-specific elevation of cerebral oxygen extraction fraction in COVID-19 ICU survivors: a pilot study
Dengrong Jiang1, Hannah Rando2, Shivalika Khanduja2, Jie Song3, Kaisha Hazel1, George Pottanat1, Ebony Jones1, Cuimei Xu1, Wen Shi4, Zhiyi Hu4, Doris Lin1, Sevil Yasar5, Sung-Min Cho2, and Hanzhang Lu1
1Department of Radiology, Johns Hopkins University School of Medicine, Baltimore, MD, United States, 2Department of Surgery, Johns Hopkins University School of Medicine, Baltimore, MD, United States, 3Department of Biomedical Engineering, Johns Hopkins University School of Engineering, Baltimore, MD, United States, 4Department of Biomedical Engineering, Johns Hopkins University School of Medicine, Baltimore, MD, United States, 5Department of Medicine, Johns Hopkins University School of Medicine, Baltimore, MD, United States Keywords: Infectious disease, COVID-19 Compared to patients with mild COVID-19 disease, critically ill patients requiring intensive-care-unit (ICU) admission are at higher risk of developing post-acute COVID-19 syndrome (PCS). The mechanisms underlying PCS are under investigation and may involve neurovascular damage, which can disrupt oxygen delivery and utilization in the brain. Cerebral oxygen-extraction-fraction (OEF) is an important parameter for the brain’s oxygen utilization. In this work, we evaluated the post-acute changes of regional OEF in COVID-19 ICU-survivors, and found that ICU-survivors had significantly increased OEF in the frontal lobe compared to controls. This suggests that regional OEF may provide a sensitive biomarker in studying PCS. |
|
1910.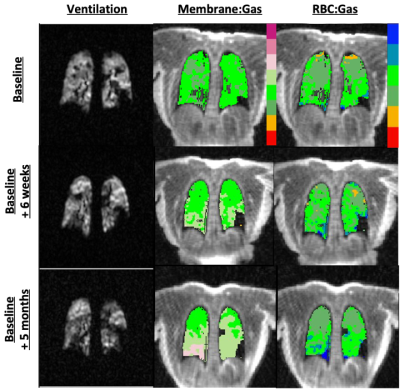 |
93 | Repeatability of Quantitative Measures in Long COVID using Hyperpolarized 129Xe MRI
Keegan Staab1, Jonathan Percy2, Andrew D. Hahn3, Stanley J. Kruger3, Alejandro P. Comellas4, Jessica C. Sieren3, Eric A. Hoffman3, and Sean B. Fain3
1Biomedical Engineering, University of Iowa, Iowa City, IA, United States, 2Physics, University of Iowa, Iowa City, IA, United States, 3Radiology, University of Iowa, Iowa City, IA, United States, 4Internal Medicine, University of Iowa, Iowa City, IA, United States Keywords: Lung, COVID-19 Repeatability visits with hyperpolarized 129Xe MRI of ventilation and gas exchange measures were acquired at baseline and 3-6 weeks after baseline in patients with persistent dyspnea, fatigue, and neurocognitive symptoms (“Long” COVID). Findings did not support the same repeatability of measures found in a previous study of IPF, suggesting instability of pulmonary pathophysiology is a characteristic of Long COVID. |
|
1911.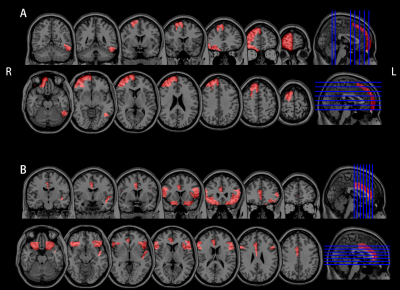 |
94 | Evident Cerebral Perfusion Recovery in COVID-19 Patients: Results Based on Arterial Spin Labeling MRI
Yu Shen1,2, Xianchang Zhang3, Yaping Wu1,2, Yan Bai1,2, Wei Wei1,2, Lijuan Chen1,2, and Meiyun Wang1,2
1Department of Medical Imaging, Henan Provincial People’s Hospital & Zhengzhou University People’s Hospital, Zhengzhou, China, 2Henan Key Laboratory of Neurological Imaging, Zhengzhou, China, 3MR Collaboration, Siemens Healthcare Ltd, Beijing, China Keywords: Neuroinflammation, COVID-19, perfusion,follow up COVID-19 may affect the brain of patients, ranging in severity from confusion to life-threatening strokes. This study investigated the potential cerebral perfusion change in COVID-19- infected patients using pseudo-continuous arterial spin labeling (pCASL) sequence by follow up after patients recovered for 4, 12 and 18 months. It’s found that both cerebral blood flow (CBF) and bolus arrival time (BAT) values derived from pCASL demonstrated an increasing tendency over time in several brain areas in COVID-19 survivors after whole brain analysis. Our findings indicated that COVID-19 survivors may experience compensatory brain function recovery and this recovery process would be slow. |
|
1912.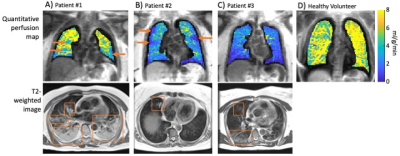 |
95 | Quantitative pulmonary perfusion in patients with COVID-19 using dynamic contrast enhanced MRI at 0.55T
Adrienne E Campbell-Washburn1, Shreya M Kanth2, Julio A Huapaya2, Matthew Thurston1, Christine Mancini1, Kendall J O'Brien1, Amanda Potersnak1, Haiyan Wang1, David Regenold3, Scott Baute1, Marcus Y Chen1, Ahsan Javed1, and Anthony F Suffredini2
1National Heart, Lung, and Blood Insitute, National Institutes of Health, Bethesda, MD, United States, 2Critical Care Medicine Department, Clinical Center, National Institutes of Health, Bethesda, MD, United States, 3National Institute of Allergy and Infection Diseases, National Institutes of Health, Bethesda, MD, United States Keywords: Lung, COVID-19 COVID-19 infection has been reported to cause pulmonary perfusion defects associated with pulmonary embolism and infiltrates. We used quantitative dynamic contrast enhanced 0.55T MRI, with pharmacokinetic modelling, to monitor lung perfusion longitudinally in 139 patients with COVID-19. We observed significant associations between disease severity and perfusion during the convalescent phase (91-365d post symptom onset); and between abnormal perfusion during the acute phase (0-40d) and low pulmonary function later during recovery. Quantitative pulmonary perfusion measured by MRI may be a useful metric to study patients with COVID-19 infection, and early results suggest long-term perfusion abnormalities in patients with severe disease. |
|
1913.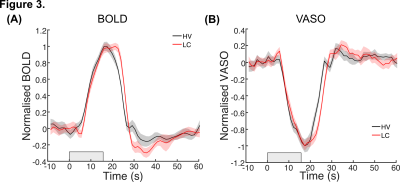 |
96 | Investigating the effects of Long COVID on cerebrovascular reactivity using VASO at 3T
Sharyfah Alasiri1,2, Elisa Zamboni2,3, Isaac Watson2,4, Heather Owston5, Heidi Baseler3,6, Dennis McGonagle7, and Aneurin Kennerley2,8
1Biomedical Sciences, University of York, York, United Kingdom, 2York Neuroimaging Centre, University of York, York, United Kingdom, 3Psychology, University of York, York, United Kingdom, 4School of Physics, Engineering, and Technology, University of York, York, United Kingdom, 5Medical and Biological Engineering, University of Leeds, Leeds, United Kingdom, 6Hull York Medical School, University of York, York, United Kingdom, 7School of Medicine, University of Leeds, Leeds, United Kingdom, 8Institute of Sport, Manchester Metropolitan University, Manchester, United Kingdom Keywords: Blood vessels, COVID-19, cerebrovascular reactivity Strategies to help sufferers from Long COVID (LC) mostly focus on symptoms management. There is an urgent need for understanding whether and how the cerebrovascular system is implicated in emergent symptoms. Here we use advanced cerebral blood volume (CBV)-based imaging techniques to appropriately quantify changes in vascular reactivity in patients affected by LC compared to healthy volunteers. A slower vasodilation mechanisms, leading to inappropriate oxygen supply during neuronal function, could be used as biomarker and help clinical diagnosis. |
|
1914.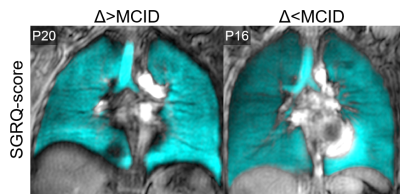 |
97 | 129Xe MRI Ventilation Predicts Longitudinal Quality-of-Life Improvement in Post-Acute COVID-19 Syndrome
Harkiran K Kooner1,2, Maksym S Sharma1,2, Marrissa J McIntosh1,2, Inderdeep Dhaliwal3, J Michael Nicholson3, and Grace Parraga1,2,3
1Department of Medical Biophysics, Western University, London, ON, Canada, 2Robarts Research Institute, London, ON, Canada, 3Division of Respirology, Department of Medicine, Western University, London, ON, Canada Keywords: Hyperpolarized MR (Gas), Lung Post-acute COVID-19 syndrome (PACS) is an umbrella term for symptoms and poor quality-of-life, four weeks+ after acute COVID-19 infection, reported in up to 30% of COVID-19 survivors. The longitudinal trajectory of PACS remains largely unknown. 129Xe MRI ventilation defects did not help to explain longitudinal quality-of-life outcomes in PACS and thus, texture analysis was used to evaluate potential ventilation features that could explain quality-of-life. We identified the 129Xe MRI ventilation texture features that predicted clinically relevant quality-of-life improvements 15-months post-infection, outperforming clinical models. These findings also suggest that ventilation texture features capture underlying pathophysiology not reflected by ventilation-defect-percent. |
|
1915. |
98 | Leakage phase perfusion in healthy volunteers and subjects post-COVID-19: results from the C-MORE study
Paul John Clifford Hughes1, Laura Saunders1, Louise V Wain2,3, Christopher E Brightling2, Stefan Neubauer4,5, Betty Raman4, C-MORE/PHOSP-COVID Collaborative Group6, and Jim Wild1
1POLARIS, University of Sheffield MRI Unit, IICD, The University of Sheffield, Sheffield, United Kingdom, 2Institute for Lung Health, Leicester NIHR Biomedical Research Centre, University of Leicester, Leicester, United Kingdom, 3Department of Health Sciences, University of Leicester, Leicester, United Kingdom, 4Division of Cardiovascular Medicine, Radcliffe Department of Medicine, National Institute for Health Research (NIHR) Oxford Biomedical Research Centre (BRC), University of Oxford, Oxford, United Kingdom, 5Division of Cardiovascular Medicine, Radcliffe Department of Medicine, University of Oxford, Oxford, United Kingdom, 6Full group details can be found in Appendix 1 of, https://doi.org/10.1016/S2213-2600(21)00383-0, London, United Kingdom Keywords: Lung, Lung Disruption to pulmonary perfusion is seen in several diseases, with most work focusing on the first-pass to calculate metrics of pulmonary blood volume and flow and mean transit time. The additional information from the leakage-phase acquisition has shown utility in multiple organs but it is less commonly used in the lung. This work aimed to assess the differences between fitting data with and without the first-pass bolus to estimate the volume transfer constant and fractions of blood in the extravascular-extracellular space and plasma in a multicentre setting. |
|
1916.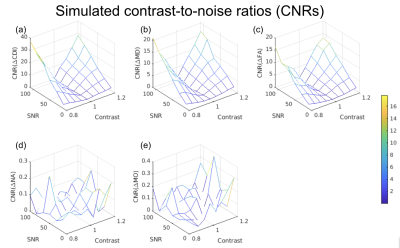 |
99 | Single-shell diffusion MRI for imaging white-matter microstructure in COVID-19: DTI vs. correlated diffusion imaging
Nick Teller1, Jordan A. Chad1,2, Alexander Wong3, Hayden Gunraj3, Xiang Ji4, Bradley J. MacIntosh2,4, Asaf Gilboa1,5, Eugenie Roudaia1, Allison B. Sekuler1,5, Benjamin Lam4, Chris Heyn4, Sandra E. Black4, Simon J. Graham2,4, and J. Jean Chen1,2,6
1Rotman Research Institute, North York, ON, Canada, 2Department of Medical Biophysics, University of Toronto, Toronto, ON, Canada, 3Department of System Design Engineering, University of Waterloo, Waterloo, ON, Canada, 4Sunnybrook Research Institute, Sunnybrook Health Science Centre, Toronto, ON, Canada, 5Department of Psychology, University of Toronto, Toronto, ON, Canada, 6Institute of Biomedical Engineering, University of Toronto, Toronto, ON, Canada Keywords: Data Analysis, Diffusion/other diffusion imaging techniques, Correlated diffusion imaging, single-shell diffusion MRI. This study examines microstructural white-matter differences between self-isolated COVID-19 patients and controls using correlated diffusion (CDI) and diffusion-tensor imaging (DTI) based on single-shell acquisitions. Correlated diffusion imaging reveals microstructural differences between patients and controls in frontal, olfactory, and cerebellar regions previously unseen with diffusion-tensor imaging. Our results suggest CDI as a feasible single-shell imaging technique that is sensitive to distinct impacts in various brain regions. |
|
1917.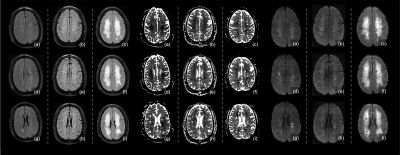 |
100 | End-of-life symptoms and imaging signs in COVID-19 patients with renal failure induced encephalopathy
Li Jiang1 and Yulin Ge1
1Radiology, NYU Grossman School of Medicine, New York, NY, United States Keywords: Neuroinflammation, Toxicity, Encephalopathy, COVID, renal, toxic COVID-19 continues to be a threat to global public health. A large number of studies have reported various neurological symptoms in COVID-19 patients even after the respiratory symptoms have resolved. In severe cases, the neurological complications induced by SARS-CoV-2 can lead to extensive neuroimaging abnormality. Additionally, previous studies have shown that, among COVID-19 patients who went through dialysis, the short-term mortality rate is high. In this study, we reported three cases of deceased patients who had severe encephalopathy while going through dialysis, to better understand their fatal disease course and associated brain MRI and clinical symptoms complicated by COVID-19. |
|
The International Society for Magnetic Resonance in Medicine is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians.