Digital Poster
Breathe In, Breathe Out & Hold Your Breath
ISMRM & ISMRT Annual Meeting & Exhibition • 03-08 June 2023 • Toronto, ON, Canada

| Computer # | |||
|---|---|---|---|
4655.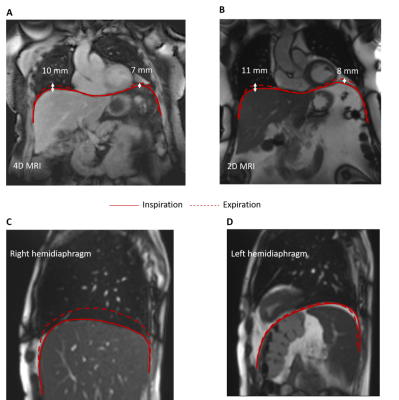 |
61 |
MRI of the diaphragm: characterizing motion and microstructural
properties in ICU patients
Myrte Wennen1,2,
Tim J. Marcus3,
Annemijn Jonkman1,
Lilian Meijboom3,
Marc Kachelriess4,
Yannick Berker5,6,7,
Gustav J. Strijkers3,
Coen A. C. Ottenheijm8,
Leo M. A. Heunks1,
Aart J. Nederveen3,
and Oliver J. Gurney-Champion3
1Intensive Care, Erasmus Medical Centre, Rotterdam, Netherlands, 2Radiology and Nuclear Medicine, Amsterdam University Medical Centers, Rotterdam, Netherlands, 3Radiology and Nuclear Medicine, Amsterdam University Medical Centers, Amsterdam, Netherlands, 4Division of X-Ray imaging and CT, German Cancer Research Center (DKFZ), Heidelberg, Germany, 5Hopp Children's Cencer Center Heidelberg (KiTZ), Heidelberg, Germany, 6Clinical Cooperation Unit Pediatric Oncology, German Cancer Research Center (DKFZ) and German Cancer Consortium (DKTK), Heidelberg, Germany, 7National Center for Tumor Diseases (NCT), Heidelberg, Germany, 8Department of Physiology, Amsterdam University Medical Centers, Amsterdam, Netherlands Keywords: Lung, Motion Correction, Diaphragm Diaphragm weakness is common in intensive care patients and has a detrimental effect on clinical outcome. Weakness in these patients may be explained by disuse atrophy or injury resulting from systemic inflammation among other factors. MRI can be used to study the motion and tissue characteristics of the diaphragm. We present the design of an MRI protocol for quantifying motion and tissue characteristics of the diaphragm. 4D MRI, relaxometry and dynamic contrast enhanced MRI were successfully applied in healthy volunteers and COVID-19 patients. Our method may aid in finding treatments and prevention strategies for diaphragm weakness in critically ill patients. |
|
4656.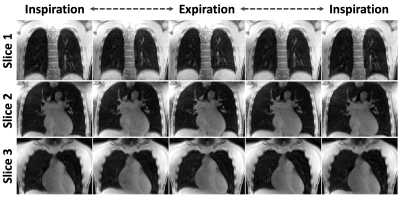 |
62 |
Spiral-GRASP-UTE: 4D Real-Time MRI of the Lung with Sub-Second
Temporal Resolution
Ding Xia1,
Ye Tian2,
Thomas Benkert3,
and Li Feng1
1Biomedical Engineering and Imaging Institute and Department of Radiology, Icahn School of Medicine at Mount Sinai, New York, NY, United States, 2Ming Hsieh Department of Electrical and Computer Engineering, University of Southern California, Los Angeles, CA, United States, 3MR Applications Predevelopment, Siemens Healthcare GmbH, Erlangen, Germany Keywords: Lung, Lung The purpose of this work was to develop a dynamic lung MRI framework, called Spiral-GRASP-UTE, for 4D real-time imaging of the lung with sub-second temporal resolution. Spiral-GRASP-UTE combines continuous ultra-short echo time (UTE) variable-density stack-of-spirals acquisition with a recently developed GRASP-Pro reconstruction technique that is based on a low-rank subspace model. Compared to other state-of-the-art lung MRI methods using 3D radial Kooshball sampling, Spiral-GRASP-UTE enables fast free-breathing dynamic lung imaging (2-3 minutes) and a high temporal resolution of less than one second per volume. This eliminates the need for respiratory motion detection and compensation, which is often challenging in lung MRI. |
|
4657.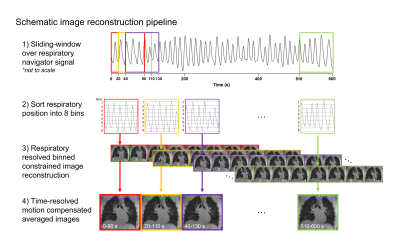 |
63 |
Dynamic lung water imaging during exercise stress
Felicia Seemann1,
Ahsan Javed1,
Jaffar M Khan1,
Christopher G Bruce1,
Rachel Chae1,
Korel Yildirim1,
Amanda Potersnak1,
Haiyan Wang1,
Rajiv Ramasawmy1,
Robert J Lederman1,
and Adrienne E Campbell-Washburn1
1National Heart, Lung , and Blood Institute, National Institutes of Health, Bethesda, MD, United States Keywords: Image Reconstruction, Lung, Exercise MRI Dynamic quantification of lung water during exercise stress is of clinical interest for early diagnosis of heart failure. In this study, we demonstrate a method to derive quantitative time-resolved lung water density maps from a continuous 3D MRI acquisition during supine exercise stress by using a motion corrected sliding-window image reconstruction. An animal model of dynamic lung water accumulation was used to validate the method, and feasibility was demonstrated in healthy subjects imaged in transitions between rest and exercise, measuring a lung water density increase of 23±10% during peak exercise. |
|
4658.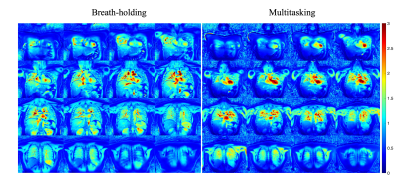 |
64 |
Motion-resolved pulmonary imaging for simultaneous fractional
ventilation and T1 mapping using MR Multitasking
Chaowei Wu1,2,
Hsu-Lei Lee1,
Nan Wang1,3,
Fei Han4,
Vibhas Deshpande5,
Andreas Voskrebenzev6,
Jens Vogel-Claussen6,
Anthony G Christodoulou1,2,
Yibin Xie1,
and Debiao Li1,2
1Biomedical Imaging Research Institute, Cedars-Sinai Medical Center, Los Angeles, CA, United States, 2Department of Bioengineering, University of California, Los Angeles, Los Angeles, CA, United States, 3Radiology Department, Stanford University, Stanford, CA, United States, 4Siemens Healthcare, Los Angeles, CA, United States, 5Siemens Healthcare, Austin, TX, United States, 6Institute for Diagnostic and Interventional Radiology, Hannover Medical School, Hannover, Germany Keywords: Lung, Quantitative Imaging Pulmonary imaging has taken on greater importance during the COVID-19 pandemic. Regional fractional ventilation (FV) and T1 from MR imaging are potential biomarkers for pulmonary tissue and functional abnormality. However, FV imaging is limited to 2-D acquisition or 3-D with low spatial resolution, and T1 imaging typically requires long breath-holding that is not practical in many scenarios. Furthermore, there is no existing technique for simultaneous acquisition of both pieces of information. To address these limitations, we propose a novel motion-resolved pulmonary imaging technique for simultaneous FV and T1 mapping using MR Multitasking, and demonstrate its feasibility in 7 healthy volunteers. |
|
4659.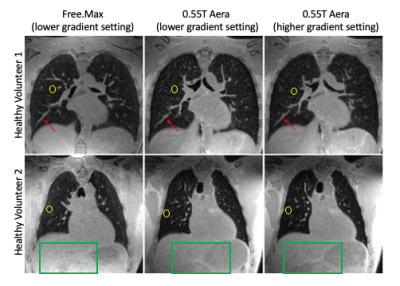 |
65 |
High resolution pulmonary imaging on a commercial 0.55T MRI
scanner
Ahsan Javed1,
Rajiv Ramasawmy1,
Pan Su2,
Thomas Benkert3,
Waqas Majeed2,
Kelvin Chow2,
and Adrienne E Campbell-Washburn1
1National Institutes of Health, Bethesda, MD, United States, 2Siemens Medical Solutions USA Inc, Malvern, PA, United States, 3MR Application Predevelopment, Siemens Healthcare GmbH, Erlangen, Germany Keywords: Lung, Lung We determined the feasibility of diagnostic high resolution pulmonary imaging on a commercial 0.55T scanner and compared the image quality to a ramped down prototype 0.55T scanner. 0.55T scanners can improve accessibility of MRI, due to their lower cost, ease of installation, and wider bore geometry. Previously, we showed robust pulmonary imaging at 0.55T using a prototype scanner with high performance gradients. In this work, we leverage our robust self-gated, concomitant and motion corrected reconstruction pipeline to enable diagnostic pulmonary imaging on a commercial 0.55T scanner with lower gradient performance. |
|
4660. |
66 |
129Xe MRS Gas-Exchange Abnormalities in Poorly-controlled Asthma
Alexander M Matheson1,
Marrissa J McIntosh1,
Narinder Paul2,
Anurag Bhalla3,
Cory Yamashita3,
and Grace Parraga1,2,3
1Medical Biophysics, Robarts Research Institute, Western University, London, ON, Canada, 2Department of Medical Imaging, Western University, London, ON, Canada, 3Division of Respirology, Department of Medicine, Western University, London, ON, Canada Keywords: Lung, Hyperpolarized MR (Gas) Large and small airway-wall and lumen abnormalities and occlusion are hallmark findings in asthma, but pathologic abnormalities have also been reported in the pulmonary vasculature. 129Xe MR-spectroscopy provides a way to quantify 129Xe gas in the airways and as it diffuses through the alveolar tissue-membrane and binds to red-blood-cells in the pulmonary capillaries. Static and dynamic 129Xe MR-spectroscopy were undertaken in participants with poorly controlled asthma in whom there was significantly different 129Xe MR RBC:membrane ratio compared to healthy-volunteers. Cardiopulmonary oscillations were observed in all 129Xe compartments; the oscillation amplitude in the gas-compartment was related to oscillometry airways impedance measurements. |
|
4661.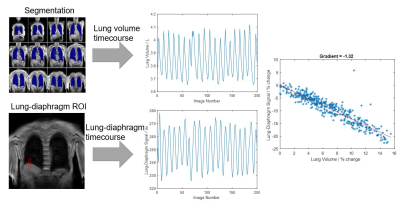 |
67 |
Investigating the Relationship between Lung Volume and the
Lung-Diaphragm Signal at 3T: Implications for Ventilation
Measures
Zachary Peggs1,2,
Jonathan Brooke2,
Jan Paul1,
Christopher Bradley1,
Andrew Cooper1,
Charlotte E Bolton2,
Ian P Hall2,
Susan Francis1,2,
and Penny Gowland1,2
1Sir Peter Mansfield Imaging Centre, University of Nottingham, Nottingham, United Kingdom, 2NIHR Nottingham Biomedical Research Centre (BRC), Respiratory Medicine, School of Medicine, University of Nottingham, Nottingham, United Kingdom Keywords: Lung, Data Analysis, COPD The relationship between lung volume and lung MR signal is key to quantifying ventilation using 1H MRI. This relationship was probed using a highly accelerated 3D FFE acquisition at 3T. Linear regression between the percentage change in lung-diaphragm navigator signal and lung volume showed that the relationship between these parameters was not always linear, especially in patient groups. Polynomial regression was used to assess the extent of the hysteresis between inspiration and expiration, with more hysteresis observed in chronic obstructive pulmonary disease (COPD) patients. |
|
4662.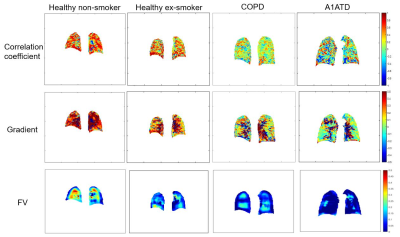 |
68 |
Functional Pulmonary Proton MRI: Voxel-wise Linear-fitting
Ventilation (VOLVE) Assessment in Chronic Obstructive Pulmonary
Disease (COPD)
Zachary Peggs1,2,
Jonathan Brooke2,
Jan Paul1,
Christopher Bradley1,
Andrew Cooper1,
Charlotte E Bolton2,
Ian P Hall2,
Susan Francis1,2,
and Penny Gowland1,2
1Sir Peter Mansfield Imaging Centre, University of Nottingham, Nottingham, United Kingdom, 2NIHR Nottingham Biomedical Research Centre (BRC), Respiratory Medicine, School of Medicine, University of Nottingham, Nottingham, United Kingdom Keywords: Lung, Quantitative Imaging, COPD The VOLVE (VOxel-wise Linear fit VEntilation, VOLVE) method, whereby voxel-wise linear fitting between the lung-diaphragm navigator signal and lung parenchyma MR signal is used to assess regional ventilation, was investigated in chronic obstructive pulmonary disease (COPD) and alpha-1 antitrypsin deficiency (A1ATD). Fractional ventilation (FV) maps derived from phase-resolved functional lung imaging (PREFUL) were also determined. Significant differences between the healthy and the lung disease groups were found, indicating the sensitivity of these techniques to emphysematous lung disease. |
|
4663.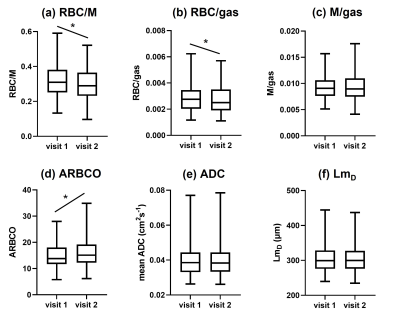 |
69 |
Longitudinal 129Xe MRI assessment of lung gas transfer and
microstructure over 1 year in patients with asthma and/or COPD
Helen Marshall1,
Guilhem J Collier1,
Ho-Fung Chan1,
Laurie J Smith1,
Paul JC Hughes1,
Dave Capener1,
Jody Bray1,
Sinoy Joseph1,
Ryan Munro1,
Olly Rodgers1,
James Ball1,
Neil J Stewart1,
Graham Norquay1,
Martin L Brook1,
Leanne Armstrong1,
Latife Hardaker2,
Titti Fihn-Wikander3,
Rod Hughes4,
and Jim Wild1
1University of Sheffield, Sheffield, United Kingdom, 2Priory Medical Group, York, United Kingdom, 3AstraZeneca, Gothenburg, Sweden, 4AstraZeneca, Cambridge, United Kingdom Keywords: Lung, Hyperpolarized MR (Gas) Longitudinal changes of 129Xe MRI metrics in patients with asthma and/or COPD have not yet been reported. 140 patients with asthma and/or COPD were scanned at 2 visits, 1 year apart, using 129Xe gas transfer and diffusion MRI. From visit 1 to visit 2 red blood cell (RBC) / membrane (M) and RBC/gas decreased and the amplitude of red blood cell oscillations (ARBCO) increased when all patients were considered. RBC/M and RBC/gas decreased in asthma+COPD, and RBC/M decreased and ARBCO increased in asthma from visit 1 to visit 2. M/gas and acinar microstructure metrics did not change significantly between visits. |
|
4664. |
70 |
129Xe MRI Assessment of Disease Progression in Patients with
COPD treated with Azithromycin: Multi-Site Repeatability and
Preliminary Results
Jaime Mata1,
John Mugler III1,
Bastiaan Driehuys2,
David Mummy2,
Laura Bell3,
Alexandre Coimbra3,
Paula Belloni3,
Peter Niedbalski4,
and Yun Michael Shim1
1University of Virginia, Charlottesville, VA, United States, 2Duke University, Durham, NC, United States, 3Genentech, San Francisco, CA, United States, 4University of Kansas, Lawrence, KS, United States Keywords: Lung, Hyperpolarized MR (Gas), COPD, clinical trial Harmonization of imaging methodology among three sites was successfully achieved. Preliminary results for longitudinal treatment with azithromycin demonstrated the sensitivity of 129Xe MRI in detecting ventilation changes, presumably caused by Sars-Cov2 infection or termination of azithromycin treatment at week 24 due to hearing loss. This preliminary data supports that 129Xe MRI is a sensitive tool for detecting subtle changes in COPD early and may potentially reduce the length of clinical trials that aim to visualize therapeutic responses. |
|
4665.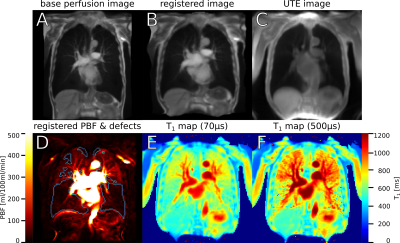 |
71 |
Local correlation of echo-time dependent observed lung T1 and
quantitative perfusion in patients with chronic obstructive
pulmonary disease
Simon Michael Florian Triphan1,2,
Marilisa Konietzke1,2,3,
Jürgen Biederer1,2,4,5,
Hans-Ulrich Kauczor1,2,
Claus Peter Heußel1,6,
and Mark Oliver Wielpütz1,2
1Diagnostic and Interventional Radiology, University Hospital Heidelberg, Heidelberg, Germany, 2Translational Lung Research Center Heidelberg (TLRC), German Center for Lung Research (DZL), Heidelberg, Germany, 3Boehringer Ingelheim Pharma GmbH & Co. KG, Biberach, Germany, 4Faculty of Medicine, University of Latvia, Riga, Latvia, 5Christian-Albrechts-Universität zu Kiel, Kiel, Germany, 6Department of Diagnostic and Interventional Radiology with Nuclear Medicine, Thoraxklinik at the University Hospital of Heidelberg, Heidelberg, Germany Keywords: Lung, Quantitative Imaging, T1 mapping, perfusion quantification, UTE Observed TE-dependent T1 has been shown to correlate with MRI perfusion scores. Here, 22 patients with COPD were examined using DCE MRI and 2D UTE. Perfusion and T1(TE) was quantified based on these, respectively. Correlations of T1(TE) with perfusion measures were examined, with the strongest inter-patient correlation at TE2=500μs but stronger local correlations at TE1=70μs and TE3=1200μs than at TE2. The average T1 in defect areas according to DCE was shorter than in normal areas, with the smallest difference at TE2. This implies that the local TE-dependence in defect voxels is further away from previously published behaviour in healthy volunteers. |
|
4666.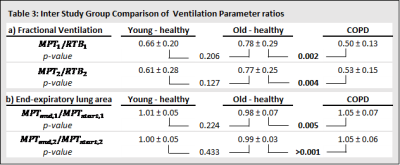 |
72 |
Dynamic single slice 2D coronal lung MRI detects metronome-paced
tachypnea (MPT) - induced hyperinflation in COPD patients
Robin Aaron Müller1,2,
Filip Klimeš1,2,
Andreas Voskrebenzev1,2,
Lea Behrendt1,2,
Till Frederik Kaireit1,2,
Julian Magnus Wilhelm Glandorf1,2,
Maximilian Zubke1,2,
Marius Wernz1,2,
Agilo Luitger Kern1,2,
Martin R. Prince3,4,
Christopher B. Cooper5,
R. Graham Barr6,
Jens M. Hohlfeld2,7,8,
and Jens Vogel-Claussen1,2
1Institute of Diagnostic and Interventional Radiology, Hannover Medical School, Hannover, Germany, 2Biomedical Research in Endstage and Obstructive Lung Disease Hannover (BREATH), German Center for Lung Research (DZL), Hannover, Germany, 3Department of Radiology, Weill Cornell Medical College, New York, NY, United States, 4Department of Radiology, Columbia College of Physicians and Surgeons, New York, NY, United States, 5Departments of Medicine and Physiology, David Geffen School of Medicine, Los Angeles, CA, United States, 6Department of Medicine, New York-Presbyterian/Columbia University Irving Medical Center, New York, NY, United States, 7Department of Respiratory Medicine, Hannover Medical School, Hannover, Germany, 8Fraunhofer Institute of Toxicology and Experimental Medicine, Hannover, Germany Keywords: Lung, Lung, COPD Metronome-paced tachypnea (MPT) is a technique where a patient breathes rapidly with a fixed frequency (40 breaths / minute). MPT induces dynamic hyperinflation and allows investigation of potential stress-driven effects on ventilation parameters. Fifteen patients with chronic obstructive pulmonary disease (COPD) and thirty healthy subjects underwent MRI with a 2D coronal lung MR image acquired repeatedly with a temporal resolution of 200 ms during resting tidal breathing (RTB) and MPT. The decrease of fractional ventilation (FV) and the increase of end-expiratory lung area (EELA) during MPT was significantly higher in COPD patients compared to respective healthy subjects. |
|
4667.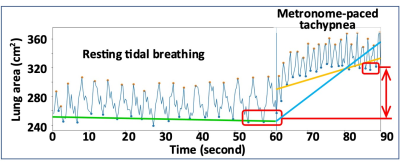 |
73 |
Metronome-paced Tachypnea-Induced Dynamic Hyperinflation on
Pulmonary cine MRI in Chronic Obstructive Pulmonary Disease:
SPIROMICS HF Study
Xuzhe Zhang1,
Martin R. Prince1,
Christopher B. Cooper2,
Michael C. Backman1,
Stephen M. Dashnaw1,
Eric A. Hoffman3,
Bharath Ambale-Venkatesh4,
Joao A. C. Lima4,
Prachi Agarwal5,
Joyce D. Schroeder6,
Jens Vogel-Claussen7,
David A. Bluemke8,
John P. Finn2,
R. Graham Barr1,
and Wei Shen1
1Columbia University, New York, NY, United States, 2University of California, Los Angeles, Los Angeles, CA, United States, 3University of Iowa, Iowa City, IA, United States, 4Johns Hopkins University, Baltimore, MD, United States, 5University of Michigan, Ann Arbor, MI, United States, 6University of Utah, Salt Lake City, UT, United States, 7Hannover Medical School, Hanover, Germany, 8University of Wisconsin, Madison, WI, United States Keywords: Lung, Lung, chronic obstructive pulmonary disease, pulmonary cine MRI, metronome-paced tachypnea, dynamic hyperinflation, transfer learning, unsupervised domain adaptation Metronome-paced tachypnea-induced dynamic hyperinflation of the lungs is typically assessed with spirometry; this method does not measure the dynamic change in lung volume over time. We implemented metronome-paced tachypnea with cardiopulmonary cine MRI. We developed an automated lung area segmentation algorithm using unsupervised domain adaptation (UDA) to measure dynamic hyperinflation in a SubPopulations and Intermediate Outcomes In COPD and Heart Failure Study (SPIROMICS HF) sample (n=65). Preliminary results showed that the integration of metronome-paced tachypnea and pulmonary cine MRI can quantify dynamic hyperinflation; dynamic hyperinflation identified on MRI appears to be associated with COPD severity. |
|
4668.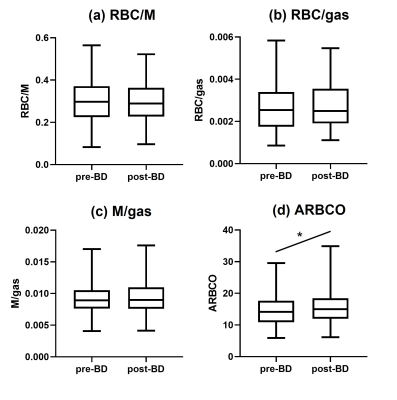 |
74 |
129Xe gas transfer lung MRI before and after bronchodilator
inhalation in patients with asthma and/or COPD
Helen Marshall1,
Guilhem J Collier1,
Laurie J Smith1,
Ho-Fung Chan1,
Paul JC Hughes1,
Dave Capener1,
Jody Bray1,
Sinoy Joseph1,
Ryan Munro1,
Olly Rodgers1,
James Ball1,
Neil J Stewart1,
Graham Norquay1,
Martin L Brook1,
Leanne Armstrong1,
Latife Hardaker2,
Titti Fihn-Wikander3,
Rod Hughes4,
and Jim M Wild1
1University of Sheffield, Sheffield, United Kingdom, 2Priory Medical Group, York, United Kingdom, 3AstraZeneca, Gothenburg, Sweden, 4AstraZeneca, Cambridge, United Kingdom Keywords: Lung, Hyperpolarized MR (Gas) Lung ventilation increases after bronchodilator inhalation in patients with asthma or COPD but there is little MRI data on how bronchodilator inhalation affects gas transfer. 117 patients with asthma and/or COPD were scanned with 129Xe gas transfer MRI before and after bronchodilator inhalation. There were no significant changes in red blood cell (RBC) / membrane (M), RBC/gas or M/gas in response to bronchodilator when all patients were considered, but RBC/gas and M/gas increased post-bronchodilator in a sub-group of patients with asthma+COPD. The amplitude of RBC oscillations increased post-bronchodilator in patients with asthma or COPD, and when all patients were considered. |
|
4669.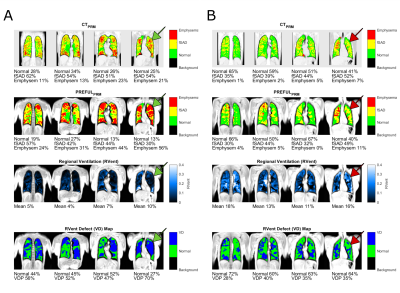 |
75 |
Detection of Emphysema using Phase-Resolved functional Lung
Imaging Parametric Response Mapping (PREFULPRM)
Andreas Voskrebenzev1,2,
Till Frederik Kaireit1,2,
Marcel Gutberlet1,2,
Filip Klimeš1,2,
Lea Behrendt1,2,
Hoen-oh Shin1,2,
Hans-Ulrich Kauczor3,4,
Tobias Welte2,5,
Frank Wacker1,2,
and Jens Vogel-Claussen1,2
1Institute of Diagnostic and Interventional Radiology, Medical School Hannover, Hannover, Germany, 2Biomedical Research in Endstage and Obstructive Lung Disease Hannover (BREATH), German Center for Lung Research (DZL), Hannover, Germany, 3Department of Diagnostic and Interventional Radiology, University Hospital of Heidelberg, Heidelberg, Germany, 4Translational Lung Research Center Heidelberg (TLRC), Member of the German Lung Research Center (DZL), Heidelberg, Germany, 5Clinic of Pneumology, Medical School Hannover, Hannover, Germany Keywords: Lung, Data Processing Ventilation measurements using signal differences between expiratory and inspiratory respiration states gained popularity as a biomarker for ventilation abnormalities. One method, which incorpartes such measurements is Phase-resolved functional lung imaging (PREFUL). A further classification of abnormalities such as emphysema and air-trapping beyond the current gas-exchange measurement is desirable. Therefore a MR adaption of CT’s parametric-response mapping (CTPRM) method is proposed as an additional post-processing method for PREFUL. The analysis of 34 patients with chronic obstructive pulmonary disease (COPD), shows that there is a high regional (Overlap normal 91%) and total lung concordance (r>0.86) for the proposed method PREFULPRM and CTPRM. |
|
4670.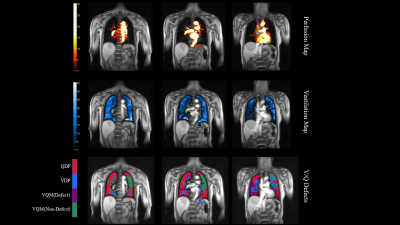 |
76 |
Assessment of pulmonary function in pulmonary embolism using
phase-resolved functional pulmonary MRI (PREFUL-MRI) under free
breathing
Tao Ouyang1,
Yichen Tang1,
Chen Zhang2,
Jens Vogel-Claussen3,
Andreas Voskrebenzev3,
Xiuqin Jia1,
and Qi Yang1
1Department of Radiology, Beijing Chaoyang Hospital, Capital Medical University, Beijing, China, 2MR Scientific Marketing, Siemens Healthcare, Beijing, China, 3Institute for Diagnostic and Interventional Radiology, Hannover Medical School, Hannover, Germany Keywords: Lung, Perfusion This study investigated the difference in pulmonary function (including perfusion and ventilation defects) using PREFUL-MRI between pulmonary embolism patients and healthy volunteers. Three coronal slices were acquisitor with MAGNETOM Prisma 3T MR scanner per subject. The results showed that perfusion and ventilation defect percentages derived from PREFUL-MRI in PE patients were higher than in healthy subjects. And the PREFUL-MRI parameters showed a strong correlation with spirometry parameters in PE patients. Our study suggests that PREFUL-MRI allows for the quantification of lung function under free breathing and non-contrast in PE patients, making this a promising tool for future monitoring of patients |
|
4671.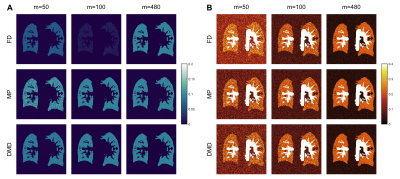 |
77 |
Using Dynamic Mode Decomposition for Functional Lung Imaging
Efe Ilicak1,2,
Safa Ozdemir1,2,
Jascha Zapp1,2,
Lothar R. Schad1,2,
and Frank G. Zöllner1,2
1Computer Assisted Clinical Medicine, Heidelberg University, Mannheim, Germany, 2Mannheim Institute for Intelligent Systems in Medicine, Heidelberg University, Mannheim, Germany Keywords: Lung, Data Processing Fourier Decomposition and related techniques have demonstrated the viability of obtaining regional pulmonary functions. To this end, novel post-processing techniques have been previously proposed to obtain ventilation and perfusion related information from dynamic acquisitions. To improve upon these methods, here we propose the use of an advanced data processing framework based on dynamic mode decomposition (DMD) for functional lung MRI. Phantom and in vivo results indicate that DMD achieves similar performance compared to established techniques and improves robustness in cases with fewer number of measurements. |
|
4672.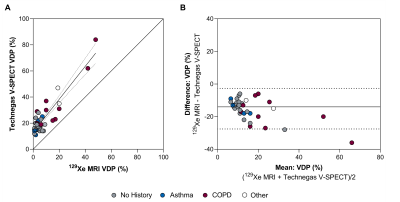 |
78 |
Comparison of ventilation defects quantified by Technegas
V-SPECT and hyperpolarized 129Xe MRI
Nisarg Radadia1,
Yonni Friedlander2,3,
Norman B Konyer2,
Mobin Jamal1,
Chynna Huang3,
Troy Farncombe 4,5,
Christopher Marriott 4,5,
Christian Finley3,6,7,
John Agzarian3,6,7,
Myrna Dolovich1,2,3,
Michael D Noseworthy 2,4,8,
Parameswaran Nair1,3,
Yaron Shargall3,6,7,
and Sarah Svenningsen1,2,3
1Department of Medicine, Division of Respirology, McMaster University, Hamilton, ON, Canada, 2Imaging Research Centre, St. Joseph's Healthcare Hamilton, Hamilton, ON, Canada, 3Firestone Institute for Respiratory Health, St. Joseph's Healthcare Hamilton, Hamilton, ON, Canada, 4Department of Radiology, McMaster University, Hamilton, ON, Canada, 5Department of Nuclear Medicine, St. Joseph's Healthcare Hamilton, Hamilton, ON, Canada, 6Division of Thoracic Surgery, Department of Surgery, McMaster University, Hamilton, ON, Canada, 7Division of Thoracic Surgery, St. Joseph's Healthcare Hamilton, Hamilton, ON, Canada, 8Department of Electrical and Computer Engineering, McMaster University, Hamilton, ON, Canada Keywords: Lung, Hyperpolarized MR (Gas) Previous studies have demonstrated the comparability of ventilation assessed by SPECT and hyperpolarized gas MRI methods; however, these comparisons were qualitative and limited to visual scoring methods based on radiologist reporting. Thus, we quantified the relationship between ventilation-defect-percent (VDP) assessed from same-day Technegas ventilation-SPECT and hyperpolarized 129Xe MRI, in patients with early-stage lung cancer. We observed that ventilation defects quantified by Technegas V-SPECT and 129Xe MRI VDP were correlated and increased in patients with COPD. A bias towards higher Technegas V-SPECT VDP was detected and may be explained by differences in contrast agent properties, image acquisition conditions, and/or quantification pipelines. |
|
4673.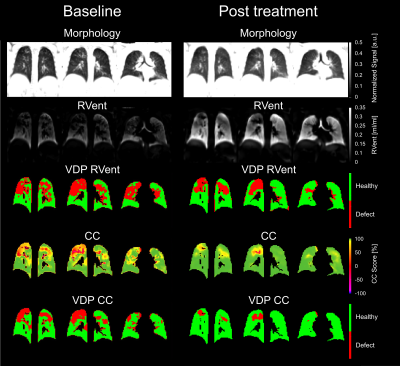 |
79 |
Effect of Kaftrio therapy on pulmonary ventilation derived by 3D
phase-resolved functional lung MRI in cystic fibrosis patients
Filip Klimeš1,2,
Andreas Voskrebenzev1,2,
Marcel Gutberlet1,2,
Milan Speth1,2,
Robert Grimm3,
Martha Dohna1,
Gesine Hansen2,4,
Frank Wacker1,2,
Diane Renz1,
Anna-Maria Dittrich2,4,
and Jens Vogel-Claussen1,2
1Institute of Diagnostic and Interventional Radiology, Hannover Medical School, Hannover, Germany, 2Biomedical Research in Endstage and Obstructive Lung Disease Hannover (BREATH), German Center for Lung Research (DZL), Hannover, Germany, 3MR Application Predevelopment, Siemens Healthcare GmbH, Erlangen, Germany, 4Department for Pediatric Pneumology, Allergology and Neonatology, Hannover Medical School, Hannover, Germany Keywords: Lung, Lung Kaftrio therapy was shown to improve global clinical ventilation parameters in cystic fibrosis (CF) patients. 3D phase-resolved functional lung (PREFUL) MRI offers a contrast-free assessment of pulmonary ventilation during free breathing. The aim of this study was to determine whether 3D PREFUL parameters are suitable to measure response to Kaftrio therapy and their association with clinical outcomes in CF patients. All assessed MRI and clinical parameters significantly improved after initiation of Kaftrio. Relative change between baseline and post-treatment scans of 3D PREFUL ventilation defect percentage maps was in agreement with forced expiratory volume in 1 second and lung clearance index. |
|
4674. |
80 |
Same-day Comparison of 129Xe MRI Ventilation Across Two MRI
Manufacturers
Rachel L Eddy1,2,3,
Vanessa M Diamond2,
Girija Bhatnagar2,
Alexandra Schmidt1,
Jonathon A Leipsic1,4,
Don D Sin1,3,
Bradley S Quon1,3,
and Jonathan H Rayment2,5
1Centre for Heart Lung Innovation, St. Paul's Hospital, University of British Columbia, Vancouver, BC, Canada, 2BC Children's Hospital Research Institute, Vancouver, BC, Canada, 3Division of Respiratory Medicine, Department of Medicine, University of British Columbia, Vancouver, BC, Canada, 4Department of Radiology, University of British Columbia, Vancouver, BC, Canada, 5Department of Pediatrics, University of British Columbia, Vancouver, BC, Canada Keywords: Lung, Hyperpolarized MR (Gas) Hyperpolarized 129Xe gas MRI (XeMRI) is gaining traction globally as a primary endpoint in clinical trials, however it is unknown how images and measurements directly compare across different MRI scanner platforms. Here we compared same-day ventilation XeMRI across two MRI manufacturers at two sites in Vancouver Canada in patients with cystic fibrosis and healthy controls, to determine the interoperability across MRI platforms. Between-site ventilation images showed strong spatial overlap, and quantitative ventilation defect percent measurements showed strong agreement across all participants. These results support the use of XeMRI in multi-center studies irrespective of MRI platform. |
|
The International Society for Magnetic Resonance in Medicine is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians.